DOI: 10.31038/AWHC.2023623
Abstract
This study investigated the context in which young women fake orgasm, as well as their reasons. A key component of this study was to examine the way that sexual scripts and societal pressures influence young women who fake orgasm. In-depth interviews were conducted with 12 college women between the ages of 19-22 who had faked orgasms during sexual intercourse. Interview transcripts were analyzed for common themes. These college women faked orgasm for a variety of reasons and in the context of a diversity of relationships. Limitations, suggestions for future research, and recommendations for sexuality education are discussed.
Introduction
Faking orgasm, also known as feigning or pretending to orgasm, has been seen in popular media for decades. When Harry met Sally, was the first movie to highlight a woman faking orgasm. In the iconic restaurant scene, Sally claims that “at one time or another most women have faked it” [1]. Television shows, including Seinfeld [2], Parks and Recreation [3], and I Am Cait [4] have all dealt with the topic, and popular magazines, such as Cosmopolitan, have feature articles on faking orgasm including “7 Sad But True Reasons Women Fake Orgasm” [5] and “Funny Ways People Faked” [6]. These examples from popular media acknowledge that faking orgasm is something some women do, and at the same time raise important questions for researchers about how common it truly is and the reasons why women fake orgasm. It has been suggested it is one of the “least well-studied human sexual behaviors” [7].
Prevalence of Faking Orgasm
Several researchers have looked at the prevalence of women faking orgasm (e.g., Caron, 2021; Darling & Davidson, 1986; Ellison, 2000; Fahs, 2014; Hite, 1976; Muehlenhard & Shippee, 2010; Wiederman, 1997) [8-14]. Four of the earlier studies to address the prevalence of women faking orgasm provided important groundwork for more recent studies. One of these earlier studies was the research by Shere Hite published in her 1976 book, The Hite report: A nationwide study of female sexuality, which was based on the responses of 3,019 women, ages 14 to 78 [12]. The Hite Report revealed that most women experienced orgasm during clitoral stimulation rather than through vaginal penetration (a somewhat revolutionary finding for that time) and that these women felt that men’s attitudes about sex needed to expand to include the stimulation women needed. Important to the current study was her finding that more than half (57%) of women reported faking orgasm [12]. A decade later, a second study was published by Darling and Davidson specifically focused on faking orgasm (referred to as “pretending orgasm”). Their sample included 868 nurses from around the United States and revealed that, of the 745 women who had engaged in penile-vaginal intercourse, more than half (58%) had pretended to orgasm [9]. Another decade later, a third study focusing on faking orgasm involved a sample of 161 college women ages 18-27 from a Midwestern state university [14]. His findings were consistent with the two previous studies in that more than half (56%) of the women reported faking an orgasm during sexual intercourse [14]. In 2000, a fourth study discussing women faking orgasm was published by Ellison in her book, Women’s sexualities: Generations of women share intimate secrets of sexual self-acceptance. Similar to Hite, Ellison reported the results of her national survey, as well as in-depth interviews with women [10]. Of the 2,311 women between the ages of 23 and 95 who answered the questions about faking orgasm, 70% indicated they had faked an orgasm at least once with their partner [10].
More recent studies in the last two decades confirm what these earlier studies have shown: many women have faked orgasm. Muehlenhard and Shippee’s 2010 study of Kansas University college women from the ages of 18-29 found that two-thirds (67%) had faked during intercourse. Their study also looked beyond sexual intercourse and found that some college women pretended to orgasm during oral sex, manual stimulation, and phone sex [13]. Fahs’ (2014) research involving in-depth interviews with 20 women ages 18-59 found that 75% of women had faked orgasm at least once in their life [11]. Nearly half (45%) of these women reported that they faked orgasm regularly during their sexual encounters [11]. And in 2021, Caron published her book, The sex lives of college students: Three decades of attitudes and behaviors based on her annual survey of college students at the University of Maine. Her findings for the 6,654 students ages 18-22 covered a wide range of sexuality topics. In terms of faking orgasm, 70% of sexually active college women in the study said they have faked an orgasm. This is the only study to look at faking orgasm over time. When looking across the 30 years, Caron found that for college women, faking behavior has increased dramatically over time – from less than half to over three-quarters of college women today saying they have faked an orgasm [8].
Reasons Why Women Fake Orgasm
Along with research on the prevalence of women faking orgasms, there are several of studies that have examined the reasons why women fake orgasm. (i.e., Bryan, 2001; Braun et al., 2014; Fahs, 2014; Kaighobadi et al., 2010; Lafrance et al, 2017; Mialon, 2012; Muehlenhard & Shippee, 2010; Roberts et al., 1995) [11,13,15-20]. In addition, Cooper et al. (2014) developed a scale to assess women’s motives for faking orgasm, The Faking Orgasm Scale for Women [7]. These reasons have ranged from concern for their male partner’s feelings and wanting sex to end, to saving the relationship and pressure to perform in order for her to appear “normal.”
The most common reason researchers have found for why a woman might fake orgasm has been out of concern for the feelings of her male sexual partner; women reported they faked orgasm in order to preserve their partner’s feelings, or in some cases, to give him an “ego boost.” This was labeled by Cooper et al. (2014) as “altruistic deceit” and based on gendered beliefs, such as if a woman does not orgasm it will negatively impact the man’s ego. In Roberts et al.’s 1995 study, some of the 75 women interviewed explained how their partner felt he had failed in some way if she did not orgasm, so faking was a way to ensure he did not feel like a failure [20]. Ellison (2000) also found that women viewed faking orgasm as important in taking care of their partner’s feelings. One of the women interviewed stated, “he had to think he was a good lover, satisfying me. Basically, faking was me taking care of the man” [10]. In Bryan’s 2001 study, the women that she surveyed described wanting to boost their partners’ egos and not hurt his feelings. Her orgasm indicated whether or not he was sexually proficient and skilled; it emphasized that sex is a skilled activity, and a woman’s orgasm was the man’s responsibility [15]. Muehlenhard and Shippee (2010) found that 78% of women had pretended orgasm in order to avoid hurting their partner’s feelings, while 47% of women faked orgasm to make their partner feel good about themselves [13]. Mialon (2012) also found that women who care about their partner’s sexual pleasure are more likely to fake; they want to make him happy [19]. And along with protecting his feelings, a woman may want to reinforce her partner’s sexual skills. Fahs found that these were common themes in both her 2011 and 2014 research [11,21]. In Braun et al.’s 2014 research, a common reason women faked orgasm was to save the feelings of their most intimate partner [16]. Most recently, a study of 462 women ages 19 to 73 in the UK found that those who held more gendered beliefs, such as women’s orgasm is necessary for men’s gratification, were more likely to fake orgasm [22].
A second common reason some women fake orgasm is because she wants sex to end (Cooper et al. (2014) labeled this “sexual adjournment” [7]. As a woman in Ellison’s study (2000) described, “I enjoy sex even without orgasm. I fake because my partner tries too hard to get me to orgasm and that turns me off” [10]. In Bryan’s 2001 study, many women faked orgasm in order to stop intercourse [15]. Their reasons for why they wanted to end intercourse included feeling tired, bored, nervous, or in pain [15]. Muehlenhard and Shippee (2010) found that 61% of women in their sample indicated that wanting sex to end was their reason for faking orgasm. The women who wanted sex to end claimed that it was because “they were bored, not in the mood, or tired and wanting sleep” (Muehlenhard & Shippee, 2010). These researchers also found that some women faked orgasm so that their partner would orgasm, and this would lead to the end of sex [13]. In both Fahs’ 2014 study and Lafrance et al.’s 2017 study, women said they purposely faked orgasms in order to end sexual encounters [11,18].
A third common reason found in studies of why women fake an orgasm included her feeling that this keeps her partner happy and the relationship intact. Some women described feeling as though they could lose their boyfriend if they don’t fake [20]. In Ellison’s 2000 study, she describes this as a common theme. One interviewee explained the reason she fakes orgasm is because she needs to please her partner so that ‘then he won’t leave me and I’ll have a boyfriend” [10]. In Bryan’s 2001 study, the researcher found that there were a broad variety of partner-related reasons, and these included, “to maintain the relationship” [15]. In Kaighobadi et al.’s 2010 study about women faking orgasm in order to retain their mate, they found that women who were more insecure in their relationships and who perceived a higher risk of partner infidelity were more likely to fake orgasm [17].
Finally, some researchers have found that the reason a woman has faked orgasm was to convince their partner that she is normal; otherwise the feeling is that there may be something wrong with her. Bryan (2001) found that some women were motivated to fake orgasm because they felt embarrassed, ashamed, or abnormal because they were not going to have an orgasm when they thought they should [15]. Bryan’s research found that women “feared appearing inexperienced or naieve;” therefore, they felt pressure to experience an orgasm [15]. Along with feelings of abnormality come feelings of guilt or shame. In Fahs’ 2014 research, some women felt her inability to orgasm implied that there was something wrong with her, as one woman explained, “I don’t want him to know that I’m one of those women who can’t get aroused from a penis inside of her” [11].
Sexual Scripts
As these studies reveal, faking orgasm is not only common, but increasing, and women of all ages indicate a variety of reasons for faking, including concern for a partner’s feelings, wanting sex to end, to save the relationship, and pressure to appear “normal.” However, the idea that today’s young women fake orgasms seems nonsensical when viewed through a modern lens.
In a society that has seen a rise in feminism, discussions of women’s empowerment and sexual pleasure, women’s marches, empowering television shows and movies, and a myriad of information available online about sexual functioning and women’s pleasure, one would think that the number of women faking orgasm would be small or have decreased over the past few decades, not increased [23]. On the other hand, sex seems to be everywhere, but is seldom talked about honestly and openly. For example, pornography is accessible, but too often unrealistic, and sex education rarely includes discussions about female pleasure [21,24]. It is no wonder that, according to Casey et al. (2013), traditional sexual scripts for women are still in existence. These scripts include women not desiring sex, having a weak “sex drive,” resisting advances, being more highly valued if she is less sexually experienced, as well as the notion that women should prefer relational sex, want commitment and monogamy, and should seek emotional intimacy and trust with sex [25].
These traditional sexual scripts also provide ideas surrounding women’s experience with orgasm. According to Lavie-Ajayi and Joffe (2009) [26] in their article Social Representations of Female Orgasm, these scripts center on three ideas: 1) women’s orgasm as the central indicator of sexual pleasure and the goal of sex, 2) vaginal orgasms are thought of as better than clitoral orgasms, and 3) while it is common for women not to experience orgasm through intercourse, if she doesn’t, it is a sign of her deficiency. These orgasm scripts suggest reasons why women might fake during a sexual encounter. Essentially, the message for women has been that “we have been taught that orgasms are obligatory” [27]. Women, as well as men, have been socialized to believe that orgasm is the goal of sex, and without an orgasm, sex is pointless. This puts an incredible amount of pressure on both parties involved, and it may be easier to fake an orgasm than to deviate from these social norms [26].
The Purpose of this Study
While a number of studies have been done over the past several decades on the frequency of and reasons for faking orgasm, many involve women across a range of ages. Few studies have examined younger women. This qualitative study investigated the context in which today’s young women fake orgasm and examined their reasons for faking orgasm. A key component of this study was to explore the ways that traditional sexual scripts and societal pressures may continue to influence college women who fake orgasm. Specifically, this study involved in-depth interviews with younger college women who have faked orgasm during sexual intercourse. The following research questions were explored:
- How often and in what context do college women fake orgasm?
- What are college women’s reasons for faking orgasm?
- How do college women feel about faking and what is their sense of how their partner(s) and friends feel(s) about women faking orgasm?
- What do the college women’s accounts of faking orgasm reveal about their sexual scripts?
Methodology
The Sample
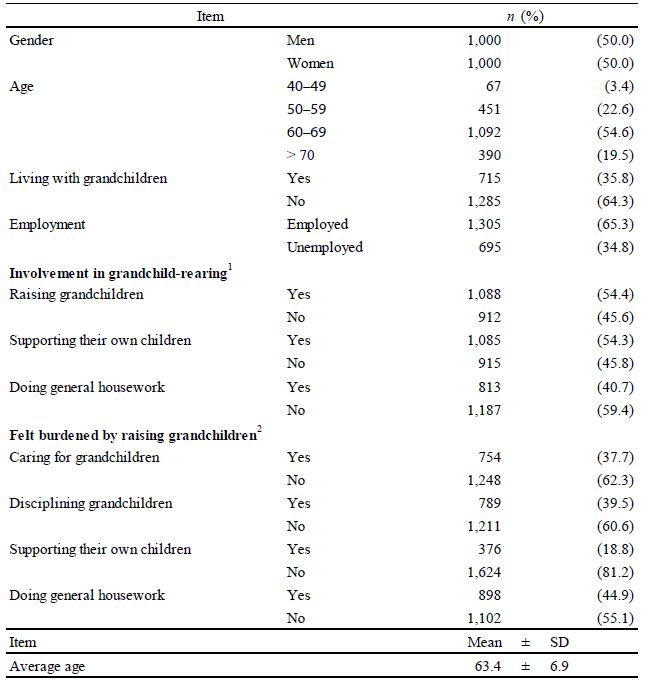
The criteria for inclusion in the study were college women ages 18-22 who had faked an orgasm during sexual intercourse. All 12 women described faking orgasm in the context of a sexual relationship with a man. Participants were recruited through announcements made in classes and e-mail announcements sent to several university discussion boards. The final sample included 12 women (Table 1) attending a public university in the northeastern United States. The age of the participants ranged from 19 to 22 years old, with the average being 21 years old. All 12 of the participants identified as White and cisgender. Ten of the participants identified as heterosexual, one identified as bisexual, and one identified as queer. The number of sexual partners each participant had ranged from 1 to 35 (M=11.6; SD=11). The number of sexual partners each participant faked with ranged from 1-20 (M=6.4; SD=6.8). Most women reported faking orgasm with most of their sexual partners. The percentage of partners they faked orgasm with ranged from 14% to 100% (M=65.4%; SD=26.3).
Table 1: Demographics of Participants (N=12)
|
Participant Pseudonyms
|
Age
|
Race
|
Sexual Orientation
|
Number of Sexual Partners*
|
Number of partners they faked with
|
Percent of Partners Faked With
|
| Abigail |
22
|
White
|
Straight
|
1
|
1
|
100%
|
| Bella |
21
|
White
|
Straight
|
6
|
4
|
66%
|
| Charlotte |
21
|
White
|
Straight
|
7
|
7
|
100%
|
| Delilah |
21
|
White
|
Straight
|
1
|
1
|
100%
|
| Emma |
22
|
White
|
Straight
|
27
|
20
|
74%
|
| Faith |
21
|
White
|
Straight
|
3
|
2
|
66%
|
| Grace |
21
|
White
|
Straight
|
5
|
3
|
60%
|
| Hannah |
22
|
White
|
Bisexual
|
9
|
2
|
22%
|
| Irene |
19
|
White
|
Straight
|
3
|
2
|
66%
|
| Jasmine |
22
|
White
|
Straight
|
22
|
3
|
14%
|
| Kaylee |
19
|
White
|
Queer
|
20
|
12
|
60%
|
| Lily |
22
|
White
|
Straight
|
35
|
20
|
57%
|
*All reported that their sexual partners were male
Interview Procedure
The interview was comprised of a series of questions focusing on the experience of faking orgasm. The Human Subjects Committee of the university approved the interview protocol. Interviews began with basic demographic questions (e.g., age, race, number of sex partners). The subjects were then asked a series of questions that centered on how often and the context for faking, what their reasons were for faking, how they and their sexual partner(s) and friends felt about women faking orgasm, and their sexual scripts.
College women who met the criteria (age 18-22 who had faked an orgasm during sexual intercourse) and expressed interest in participating in the study were provided with a copy of the consent form before an interview was scheduled. Consent was implied when they agreed to arrange an interview after reviewing the consent form. Consent was also verbally provided by the participants at the start of the interview. Interviews were conducted face-to-face in a private space on the university campus. Participants were assured that any and all responses would be kept confidential. No names or identifying information was included in the data report; a pseudonym was assigned to each participant, and any names of partners or friends mentioned in the interview were changed. Each interview lasted approximately ninety minutes. Interviews were tape recorded and extensive notes were taken. At the end of the interview, participants were given the opportunity to review the notes with their responses for omissions or clarifications. The taped interviews were later transcribed and afterwards the content from the taped interview was deleted.
Interview Analysis
Interview transcripts were analyzed using established methods of qualitative inquiry, including coding and categorizing processes that make use of both deductive and inductive approaches [28]. Thematic analysis was utilized to analyze and code the interviews. The first and second author read the first three interview transcripts independently, and initial coding of the transcripts involved marking comments that fit under the four research questions of focus for the study: frequency/context, reasons, feelings, and scripts. For example, a response that encompassed a woman’s reason for faking orgasm would have the initial code word “reason” added next to it. Next, coding categories or themes were created under these areas of focus through a process of open coding [28]. For something to be considered a theme, at least half of the women (six women) needed to discuss this in their responses. For instance, under the responses for “reasons,” if six or more women mentioned that the reason she faked an orgasm was because she worried about her partner’s ego and/or did not want to hurt his feelings, this was categorized under that theme. These were compared and coding categories were further developed.
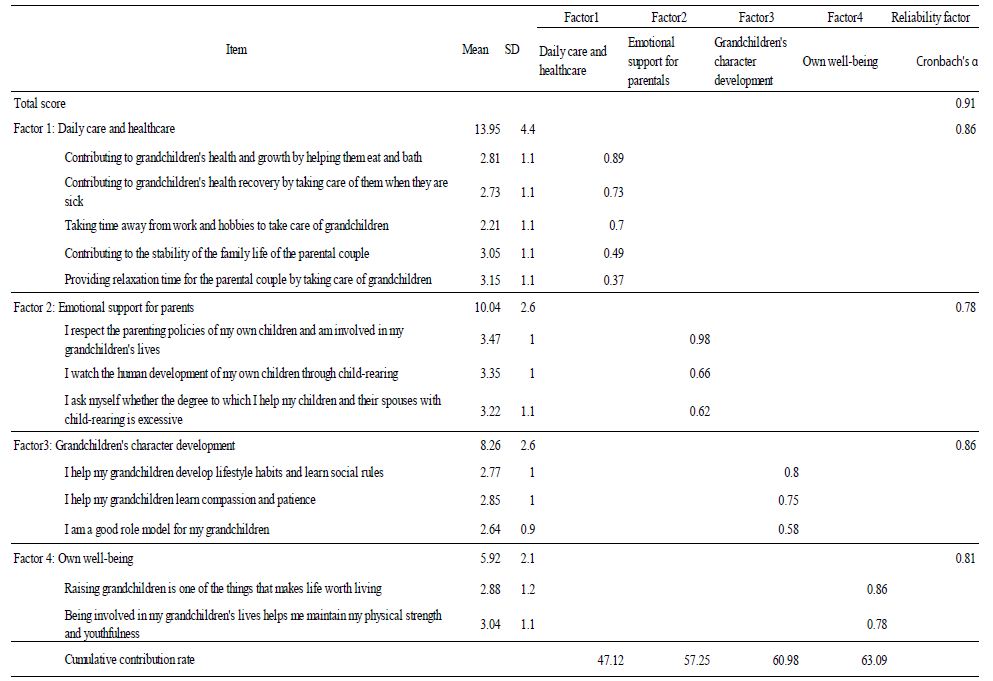
The rest of the interviews were coded by the first author and reviewed by the second author as any changes or additions were made. No new coding categories emerged after approximately 10 interviews were completed, leading to assurances of content saturation. A total of 16 themes emerged from the coding. These are discussed below and presented in Table 2. In terms of frequency and context for faking orgasm, four themes were identified. For reasons for faking orgasm, five themes were determined, and for feelings about faking orgasm a total of four themes were identified. Finally, the fourth research question sought to understand what young women’s accounts of faking orgasm reveal about their sexual scripts. Three sexual scripts were identified and will be discussed.
Table 2: Themes identified for college women’s frequency and context of faking orgasm, reasons for faking orgasm, feelings about faking orgasm, and sexual scripts related to faking.
| Frequency and Context of Faking Orgasm
· How often: It depends
· How she faked: I was a great actress and lied
· When she faked: It was typically with intercourse
· Who she faked with: When I didn’t know him well |
| Reasons for Faking Orgasm
· I did not want to hurt his feelings
· I was uncomfortable being with him
· I felt I was taking too long
· He did not know what he was doing
· It’s expected |
| Feelings about Faking: Hers, Her Partner(s), and Her Friends
· I feel it is pretty normal
· I feel guilty, but it was necessary
· My sexual partner would feel deceived
· My girlfriends feel it is perfectly okay |
| Sexual Scripts
• Media messages of what “normal sex” looks like
• Her orgasm is a reflection of his competence
• Her orgasm signals that sex is complete |
Findings
Themes are reported below for each of the areas of focus for this research: frequency and context of faking orgasm, reasons for faking orgasm, feelings about faking orgasm, and sexual scripts. Direct quotations from the interview transcriptions are included to highlight the findings (Table 2).
Frequency and Context of Faking Orgasm
The first research question asked, “How often and in what context do college women fake orgasm?” The 12 college women were asked a series of questions to understand their experience of faking orgasm. Four unique themes were identified from the in-depth interviews, including how often she faked, how she faked, when she faked, and who she faked orgasm with. These are described below and are listed in Table 2.
How often: It depends. The first theme related to the frequency and context of faking orgasm was related to how often the women faked an orgasm. When asked how often they had faked an orgasm, the most common response was “it depends,” with responses ranging from “only a few times” to “hundreds of times.” For many women, it depended on a range of factors from how inexperienced she was or how inexperienced her partner was, to how well she knew him or how much pressure she felt. While some women said they had faked an orgasm only a few times in one relationship, others indicated they had faked “hundreds of times” in most relationships. Examples of how college women described how often they faked an orgasm are included below:
I did it more at the beginning of our relationship, and then less later into the relationship because I think that we both started learning more what we liked in the bedroom. I would say almost the majority of the time at the beginning of the relationship and then almost not at all as the relationship progressed forward. (Grace)
I would say that every one-night stand that I have had, I pretty much faked with. Like when I have a one-night stand, I would say it’s a guarantee pretty much that I am going to fake. It’s usually different than when I’m with someone that I’m emotionally close to. (Lily)
How she faked: I was a great actress and lied. The second theme related to frequency and context of faking orgasm focused on how she actually faked her orgasm. The majority of women described how faking orgasm involved good acting and included descriptions of the kinds of actions (i.e., body movements and sounds) they would engage in. They also said that when asked by their partner after sex if they had had an orgasm, they deliberately lied to him. Many not only described being good at faking, but also discussed getting better overtime with more sexual experiences. Some sample quotes describing how she faked include:
I verbalize, like moaning and getting grabbier. Definitely working myself up kind of thing and then heavy breathing afterwards. That was always a definite and I was like “Oh my God” ((panting)) kind of thing. I would say that I usually didn’t say anything though, just used my muscles and I would scratch their back too. (Kaylee)
I didn’t use just my body. He was like, ‘Did you get it?’ and I just said “Yes” even though I didn’t, so most of the time it’ll be like physical and moaning except for the two times that I straight up lied out of my mouth. (Charlotte) When she faked: It was typically with intercourse. A third theme related to frequency and context of faking focused on sexual intercourse. All 12 college women described faking orgasm during penile-vaginal intercourse. Two women added that they had also faked an orgasm during oral sex. Some women described that they began faking orgasms during sexual intercourse before they had ever had a real orgasm, but once they experienced an orgasm and knew what it felt like, they got better at faking. Some examples of women explaining when they faked include:
I fake during intercourse because I don’t even have a reason. Oral depends, I don’t know, I fake during both of them, but most commonly during intercourse because like I said, I don’t orgasm just by intercourse alone, so, uh, it is to make him feel better. (Delilah)
I emphasized more or got more convincing when I was faking when we were having sex. I think that because I knew what the orgasm was supposed to feel like because of a previous relationship, I was better at faking when I was doing stuff with other guys. (Irene)
Who she faked with: When I didn’t know him well. The fourth and final theme related to frequency and context of faking centered on how well they knew their sexual partner. All 12 college women talked about how they faked orgasm with someone they did not know well, either in the context of a one-night stand or in the very beginning of the dating relationship. It was described by many as “easier to get away with” if they faked an orgasm with someone whom they did not know and would never see again. Most described faking at the start of a relationship that eventually evolved into something long-term. As their partner got to know their sexual needs, there was no need to fake anymore. Some examples describing who women faked with include:
We were dating for less than a year, I only did it like a couple of times in the beginning ‘cause I kind of almost felt bad ‘cause it’s like obviously you’re putting a lot of effort in, you really are trying. It was just sometimes it was not going to happen and also that was one of my early relationships so I wasn’t as comfortable talking openly about it so I didn’t feel okay asking him to try something different. (Jasmine)
I only dated him for like three months, it was a stupid relationship. We didn’t have sex very many times, so this is kind of awkward, but I faked every single time with him. We only had sex like three times. This is so sad. I never even had an orgasm with him. (Bella)
Reasons for Faking Orgasm
The second research question asked, “What are college women’s reasons for faking orgasm?” A series of interview questions explored their most important reasons and what their rationale was for faking orgasm. Five themes were identified for the reasons women said they fake orgasm, including not wanting to hurt his ego, experiencing uncomfortable emotional and physical feelings with him, worrying she was taking too long, feeling like the guy wasn’t doing anything that was stimulating her, or she felt it was expected that she reach orgasm as part of sex. Each woman had many reasons for faking (not just one) and their reasons varied based on the context of the sexual experience. These five themes are described below and listed in Table 2.
I did not want to hurt his feelings. The first theme related to reasons for faking included concern for his feelings. Most of the college women described faking orgasm because they were worried about his ego and whether or not he would feel like he was a good sexual performer. Examples of things women said included:
I guess mainly I was just trying to make my partners feel better about themselves and that’s why I would never say, “Hey I’ve been faking the entire time we’ve been sleeping together” because that would take away all that validation too. Plus, I feel like it’s kind of a waste of time to be faking quite a bit and then tell the partner that you were faking. Their feelings are really going to get hurt that way. (Hannah)
I think that men get their feelings hurt easily and they’re very sensitive when it comes to sex and they always want to protect their ego and I think that there’s at least in some way pressure on women to fake orgasms so that they protect the feeling of their male partner. (Abigail)
I was uncomfortable being with him. The second theme related to reasons for faking orgasm was because they were really uncomfortable being with their sexual partner and therefore knew the sexual encounter was not going to lead to orgasm. They described being emotionally uncomfortable in terms of not being able to relax with him, not feeling a connection to him, or feeling very self-conscious. Many women also mentioned feeling physically uncomfortable (i.e., pain) and faking orgasm in order for the sex to end. For example:
I think “discomfort” would be the one-word summary of why I faked. I think with the more casual relationships, I never was emotionally close to them so I was emotionally uncomfortable with the situation. I felt like, “I don’t like that you’re seeing my boobs right now and I hardly know you.” With my first boyfriend it was probably more like, “This is my first partner ever, I don’t know what I’m doing.” I’m self-conscious, that’s why I’m uncomfortable and also when you don’t really know what you’re doing. I think physically that’s uncomfortable too. (Charlotte)
I felt like I was taking too long. The third theme related to the reason why women faked orgasm was because it was taking them too long to reach a real orgasm. They were worried that their partner would think something was wrong with them or they felt pressured by their partner continually asking, “Have you come yet?” Some examples of quotes from women describing how they felt they were taking too long included:
It’s more like I felt that I should reach an orgasm sooner, more than because he wasn’t going to give me one cause he’s doing the same things he usually does [when I have an orgasm] but sometimes it’s just not as fast. I feel like sometimes it takes me a lot longer to have an orgasm, but I don’t know why. I feel bad when it takes me a long time ‘cause then I think he feels bad too. (Delilah)
I feel like the guy is going to think that something is wrong with me if I don’t have an orgasm. I don’t want him to think that he just had sex with a weirdo after he finishes. He would ask me if I had orgasms, and I hated that. He did it all the time during sex, it made pleasure really difficult to focus on. (Bella)
He didn’t know what he was doing. The fourth theme related to reasons women gave for why they fake an orgasm was because the man they were with did not seem to know what he was doing in terms of stimulating her. Women described how they were sure they would not be reaching a real orgasm with him and therefore felt their only option was to fake an orgasm. Examples of this included:
I think with the other guys [one night stands] it was different. They didn’t really know what they were doing. If I was going to be in a long-term relationship, it would be different, but I had no confidence in the men that I slept with. I would always be like “Eh, they’re never going to get it,” so I would fake because I’m pretty sure that I just wouldn’t have ever have an orgasm in those encounters. (Emma)
I think that the majority of the time I fake because they are not doing anything and I’m not getting very stimulated throughout the whole thing, so I just don’t feel like it’s going to happen no matter how long it goes. No matter how long we like had sex, I wasn’t going to have an orgasm. (Lily)
It’s expected. The fifth theme related to reasons why women faked orgasms included an expectation and pressure to have an orgasm with intercourse. All of the college women said they believed it was what needed to happen in order for sexual intercourse to be complete. Not only should he orgasm, but she needs to orgasm as well. Women described this expectation and pressure in the following examples:
Guys just think we should have an orgasm, so that’s how it happens. I think there’s a huge amount of pressure on many women to have an orgasm, so they end up faking. I wouldn’t say anyone is happy to fake orgasms because normally the situation that you find yourself in is not ideal. (Abigail)
I feel like guys expect you to orgasm, but among girls I feel like it’s an understanding that having an orgasm during sex is not quite so common. I kind of think that’s where faking comes from because girls all understand how difficult it can be to have an orgasm, but guys just don’t seem to get it. I think that they kind of like originate the pressure, but sometimes I feel like I internalize that and then like I feel like I need to have an orgasm. (Emma).
Feelings about Faking: Hers, Her Partner(s), and Her Friends
The third research question asked, “How do college women feel about faking and what is their sense of how their partner(s) and friends feel about women faking orgasm?” The 12 college women were asked a series of questions to explore their feelings about faking, as well as the feelings of those around them. Four unique themes were identified from the in-depth interviews. Many women stated that both she and her friends feel that faking orgasm was typical or normal behavior. Most admitted feeling guilty, but recognized it was necessary, and they described how they never discussed faking with their sexual partner because they knew his response would not be good. These are described below and are listed in Table 2.
I feel it is pretty normal. The first theme related to the women’s personal feelings about having faked orgasm and centered on how normal this behavior was within a sexual encounter. Women seemed to shrug their shoulders and be unphased about having faked and orgasm. Many were okay with faking orgasm and saw it as a useful tool in many sexual encounters. Examples of women’s description of their feelings include:
I don’t think I’m doing anything bad. Just kind of like neutral. I think it’s pretty normal though, and I don’t think that many women feel bad about faking, especially because they are faking to not hurt their partner’s feelings. (Delilah)
It’s so normal, almost like, it shouldn’t be so normal, it shouldn’t be something that I have to do, I just don’t even think about it. I feel like it’s become like I’m used to it. It is what it is. No one really puts any thought into it. I don’t care that I have done it personally, but it’s probably something that I should change at some point. (Emma)
I feel guilty, but it was necessary. The second theme focused on how women feel about having faked orgasm and involved guilt. However, these women also qualified these guilty feelings by saying that faking was necessary in many situations they found themselves in order for the sexual encounter to be considered a success. Some quotes from college women about these feelings include:
I feel bad that I didn’t address it, I mean lying is really what I feel guilty about, but I didn’t want to make either of them feel bad. Going back, I would definitely talk more about it ‘cause that’s super important but going back I was just too shy at the time to discuss it. (Irene)
It is disappointing to fake cause I didn’t feel like my needs were important enough to tell the guy about. It is always hard for me to say, “That wasn’t good for me.” I am also okay that I didn’t make them feel bad, but also I was lying so then you kind of feel guilty anyway. (Faith)
My sexual partner would feel deceived. The third theme to emerge related to feelings about faking orgasm involved her thoughts on how her sexual partner would feel if he knew. All of the college women indicated they were not willing to tell their sexual partner they had faked because they were sure he would respond in a negative way. All of them were sure he would feel lied to or deceived. This reaction was confirmed by a few women who shared that they had later told a sexual partner about faking, and his response was to feel lied to and deceived. Sample responses included:
I haven’t ever talked about that with any of my sex partners. That would be so awkward and embarrassing for both of us because he would feel like he couldn’t get me off. (Bella)
I don’t want it to come out that I have faked in the past, so it’s not something that I ever bring up with my partner. I don’t want to hurt my partner’s feelings, so I would not want to talk about it. I don’t think that guys like to think that anyone has ever faked with them because that would hurt their confidence, so they probably don’t want to bring it up either. (Kaylee)
My girlfriends feel it is perfectly okay. The fourth theme related to feelings about faking orgasm centered on her friends’ reactions to finding out they fake. The overwhelming response from her girlfriends was that it is perfectly normal behavior and not surprising. Women talked only about their female friends’ response; none of the women discussed how male friends would feel about her faking orgasm with a partner. Some example of friends’ feelings about faking orgasm include:
I talked to my friends before I met you for this interview. I texted everyone. And one of my roommates responded back, “Have I faked an orgasm? Do you mean am I a woman?!” We all just laughed because it’s so regular. I feel like with my friends it’s the norm, and that’s what a lot of women unfortunately do. (Abigail)
So the only people I’ve ever talked about this with are my current roommates. We talked about it and all of us kind of joked like, “Oh girl, have I faked? Hell yes I faked, who hasn’t faked?” But it never went really beyond that. They didn’t have any specific reaction when I told them that I personally had faked. I think that most women just assume that all other women are faking, too. (Charlotte).
Sexual Scripts
An examination of the transcripts revealed three overarching sexual scripts these college women internalized to explain their faking orgasm behavior. These sexual scripts include: 1) media messages of what “normal sex” looks like, 2) her orgasm is a reflection of his competence, and 3) her orgasm signals that sex is complete. These sexual scripts are discussed below. Sample quotes are included to highlight these scripts.
Media messages of what “normal sex” looks like. The first sexual script centered on the media. Many of the women didn’t know exactly where their ideas, reasons for, or feelings about faking orgasm originated from, but they were able to cite the media as playing a very important role. Women discussed movies, television shows, and pornography. Women found these various types of media to be influential in their sex lives and to offer them an understanding of what “normal sex” should look like. Some sample quotes describing women’s experiences with media are below:
I think in my experience the way that men and women act has a lot to do with porn and when they watch it. Like the women through the whole entire thing are having orgasms, multiple orgasms. I think that porn plays such a big role in the expectations today. If you have a partner that looks at porn and always thinks it’s going to be the reality of sex, then that’s going to cause a lot of problems in the relationship. (Delilah)
I haven’t really thought about where I learned about faking orgasm before. I don’t want to say TV shows because that’s cliché, but you know how sometimes on TV you might see stuff like that, I don’t know, but I feel like the women on the TV fake it. It’s not like I’ve ever really given it thought, though I guess, I think I would say TV was a pretty big influence. (Grace)
I think that porn is a big reason why women fake, the way that sex is shown makes men think that sex in real life is going to be different than it actually is. Even in movies and stuff, sex is like this amazing thing that everyone wants to have, like in American Pie, but in real life it’s not ever really that interesting. I think sex can be really boring, especially if the guy has no idea what do to with your body. (Faith)
Her orgasm is a reflection of his competence. The second sexual script centered around her orgasm as a reflection of him. Nearly every single woman interviewed had faked orgasm because they understood that her ability to reach orgasm assured him he was competent. This sexual script suggests these women have learned that sex is about him; it’s about assuring him of his abilities, his sexual prowess, and his manhood. All women described the pressure from their partner to orgasm in order to assure him of his competency. Some examples of this can be found below:
With my boyfriend I would fake because I didn’t want to make him feel bad. And I think the other two guys, I mean, maybe it was just kind of, I guess the best reason would be like societal expectations. I don’t know, I always kind of feel like it’s something that should happen during sex. Even if they didn’t make me orgasm, they did make me feel good in at least some way, and faking was kind of my way of like showing even if they really didn’t make me orgasm, they were doing something good. (Grace)
Um, honestly I fake for him, so as not to hurt their ego because men are babies. They couldn’t handle rejection, so I would basically just fake with them because I didn’t want to hurt their feelings or anything. Men need to feel strong, needed, and important. So, I think that giving a girl an orgasm is very important to their self-esteem; if they are unable to give a girl that orgasm it hurts their self-esteem and makes them feel like they aren’t as sexually powerful as they should be. (Bella)
I think that men kind of originate the pressure to have an orgasm. Sometimes I feel like I internalize that and then like I feel I need to have one. Guys always want you to have an orgasm. I think it makes them feel better and more accomplished and then they get the added bonus that their partner is having a good time too. (Emma).
Her orgasm signals that sex is complete. The third sexual script is that women felt like sex was not complete until she experienced an orgasm. Not only did women feel this way, many also proclaimed that their male partners felt similarly. This pressure to perform in order to make the sex act complete was a recurring sentiment. Some sample quotes are below about women feeling as though their orgasm signals to the male partner that he can now orgasm and then sex is complete:
I wanted it to be over, so faking the orgasm was how I decided that I wanted to end the sexual encounter. I learned that if I wanted to end sex, then I could fake orgasm because that was a signal to him that he should be finishing up soon. (Charlotte)
At the time I felt like an orgasm was supposed to happen and then that was sort of like the mark of the end of the experience so I should basically have one to finish things up. (Irene).
Discussion
This study sought to add to our understanding of how and why women fake orgasm. There have been previous studies on women who fake orgasm, however, several are decades old and/or include a very broad age range of participants. For a behavior that appears to be extremely common in sexually active women, and one that has been increasing among college women over the past 30 years [8], there is a need for more research to understand this phenomenon. This study focused exclusively on a younger cohort of educated, college women who had faked orgasm. It involved in-depth interviews in order to understand the context, reasons, feelings, as well as to determine the sexual scripts that are influencing faking orgasm among today’s young women.
Comparison of Findings to Previous Research
Frequency and context of faking orgasm. In terms of the frequency and context of faking orgasm, there was a great variation in how often these college women reported they had faked orgasms. Some women reported that they faked every single time they had sex, while others had only faked a few times in their life. Other researchers also found that there was a wide range in frequency of faking among their study participants. For example, Bryan’s (2001) [15] found that 20% of women faked orgasm during 20% of their encounters, Fahs (2014) [11] found that 45% of women report that they faked orgasm “regularly” during their sexual encounters, and Ellison (2000) [10] found that while most had faked less than 50 times; 10% of the women claimed to have faked orgasm between “150 and 10,000 times or wrote in another answer such as ‘countless’ or ‘a bazillion’” [10].
Most of the college women in this study discussed pretending to orgasm by using their bodies and lying if their partner asked them about having an orgasm. Many women described “putting on a show” for their male partner so that they would not suspect anything. This was a finding described in other studies of women faking orgasm (e.g., Bryan, 2001) [15]. In addition, they all discussed how faking orgasm typically occurred with sexual intercourse. Few women identified faking during oral sex. Earlier studies (e.g., Darling & Davidson, 1986; Wiederman, 1997) [9,14] also specifically explored women who faked orgasm and found this to be typical.
Two findings related to frequency and context were unique to this research. First, the college women in this study reported that they got better at faking over time. Many noted that the longer they faked, the more convincing they felt they became. And related to this, once they experienced a real orgasm, they felt their ability to convincingly fake future orgasms improved considerably. The other unique finding that has not been discussed in previous research related to the context was that these college women described faking orgasm at the beginning of a relationship. All of the women faked when they were “less close” with their partners and had “less emotional attachment.” For some women (those who had only one-night stands), this pattern continued, but for those who had long-term boyfriends, they stopped faking as the relationship progressed.
Reasons for faking orgasm. In terms of the reasons why women fake, almost every woman interviewed agreed that they faked orgasm in order to save their partner’s feelings. The women were more concerned with their partner’s ego than with their own pleasure during the sexual experience. This finding was similar amongst nearly all of the previous research on reasons why women fake [7, 10, 13, 15, 16, 19, 20, 21]. For many women, it was reported that it was easier to fake and “protect his feelings” than to tell him the truth and deal with an uncomfortable conversation. Other reasons women cited for faking were similar to previous studies noted earlier including being uncomfortable, worrying she was taking too long, and feeling the pressure to orgasm.
Unique findings in this study related to reasons women fake orgasm included college women talking about experiencing physical pain, lack of concern for maintaining the relationship, and because he did not know what he was doing. In this study, many of the women cited feeling physically uncomfortable (not just emotionally uncomfortable) and cited this as a reason for faking orgasm in order to have the sexual encounter stop. Few of the previous study [15] discussed that women fake orgasm because of physical discomfort.
In addition, many of the previous studies found that a common reason why women fake was to keep the relationship intact [10, 12, 17, 20]. In the current study, not one of the college women talked about this as a reason for faking an orgasm, which raises questions about today’s college women and their focus on long-term commitments.
Another unique theme noted by college women in this study to explain their reason for faking was because their partner did not know what he was doing. The women who discussed this felt as though they would never experience an orgasm with their partner and therefore faked orgasm. These women were faking orgasm in order to end the encounter, and this is where there are similarities to the other studies [10,11,13,15,18]. These previous studies found that women would fake orgasm to end the sexual encounter, however it was for a variety of other reasons such as being tired, bored, or uncomfortable, not that the male partner didn’t know what he was doing. This reason for faking could be explained in large part because of the young age of the female respondents, who in turn may have young, sexually inexperienced partners who do not know what is involved in pleasing their partner.
Feelings about faking. Several studies have investigated how women feel about faking orgasm and women have suggested their male partner would be hurt to know [10, 11, 18], but asking about how their friends feel about their faking behavior has not been a focus of past studies. In this study, the college women were divided in their own feelings about having faked orgasm. On the one hand, many of the women felt as though their behavior was normal and nothing they were concerned about; on the other hand, many women felt guilty about faking orgasm, but they also justified their actions as necessary. These women knew that faking may not have been the right thing to do, but they could justify why it was done. In addition, most of the college women mentioned that they didn’t tell their partner about faking orgasm because they did not want him to have a negative response.
A unique finding in the study was the reaction of her friends. The college women interviewed for this study all described their female friends as having a supportive view of faking orgasm. Many of their college girlfriends shared that they do the same thing, and that they also believe faking orgasm is a very normal behavior.
Sexual scripts. The finding that many college women discussed the role of the media in defining what “normal sex” is and what female orgasm is supposed to look like was unique. Few of the previous studies [11] examined women’s sexual scripts or the variety of societal pressures that are placed on women. All the women in this study described the important role of the media in shaping their understanding of sex and orgasm. The college women participating in this study mentioned either learning about orgasms or faking orgasms through some sort of media such as pornography, movies, or television. These women mentioned having a fantasy version or unrealistic idea of what “normal sex” is “supposed” to look like due to the media influence in their younger years.
The second script that arose from the interviews with college women is the notion that her orgasm serves as a reflection of her partner. Previous studies have also described this need for women to assure her partner of his competency. [26, 27] discuss how it becomes obligatory for women to have an orgasm. A large goal of her orgasm is not about her pleasure; rather it is about making sure her male partner is happy and confident about his own sexual abilities. This belief system further ingrains the sexual double standard that the male orgasm is for pleasure while the female orgasm is for performance. Other studies [11, 15] found that many women faked because they felt that they needed to show their partner that he is doing a good job and give him the impression that they are enjoying sex as much as he is.
Finally, the third script to emerge from the interviews was the notion that female orgasm signals that sex is complete. Many of the women discussed faking orgasm in order to end the sexual experience. This is similar to other studies such as [26] in which they noted that the woman’s orgasm is the “goal of sex.” Similar to the current study, the female orgasm is seen as what needs to happen for the sex to be complete.
Limitations
As with all qualitative studies, the findings of this study cannot be generalized. There were several limitations to this study beginning with a small sample size and being limited by participants who were willing to be interviewed for the study. In-depth interviews were completed with college women who volunteered and therefore may be more open and comfortable with talking about faking orgasm. The interviews relied on the participants’ ability to recall as well as their perceptions of events, which could not be verified. This study was also limited to students who attended one public university in the northeastern U.S. and all shared the same race. A more diverse group of participants may impact the findings. Factors such as women’s race, socioeconomic status, culture, or religious orientation could all play into women’s propensity towards faking orgasm, along with their willingness to discuss such matters.
Future Research
The prevalence of faking orgasm and the reasons why women fake have been the focus of many studies, however, as noted earlier, it is one of the “least well-studied human sexual behaviors” [7]. In relation to the current study, it would be beneficial for future studies to conduct more in-depth investigations focusing on specific aspects of the current study. Future studies could focus solely on the context of faking, reasons for faking, or feelings a woman or her friends might have about faking orgasm. It would also be beneficial to look at the deeper meaning of faking orgasm in terms of the sexual scripts.
It is important to note that all of the participants in this study ranged in age from 19 to 22 years old. This sample was chosen because of the interest in examining young women’s experiences. Recognizing that faking orgasm is increasing among this age group, it is important to understand why. It is useful to examine this age group to understand how society, media, self-image, and male partners all affect their faking behavior. Other studies could compare how younger women differ from older women in their attitudes, beliefs, and influences. Future research could also compare women based on other factors such as ethnicity, race, religion, socioeconomic factors, and sexual orientation. The participants for this study were all women who shared their experiences of faking orgasm with male partners. Further research could examine how women in same sex relationships experience faking orgasm.
Suggestions and Recommendations
The frequency with which women fake orgasm, and the pressure women feel from their partners to reach orgasm provides several suggestions and recommendations for sexuality education. First and foremost, there is greater need for education of basic anatomy, as well as opportunities for discussion of what students see as the purpose of sex. It appears that for many of the women interviewed in this study, sex involves feelings of pressure, and involves an act or performance in order to prove (mostly to the male partner) that the sexual encounter was a success and that she is normal and okay. Better sexuality education is needed for both men and women in order to have a more realistic understanding of sexual function and the role of pleasure.
Second, there is a need for media literacy and a discussion of the role of pornography specifically in shaping ideas about sex. Many of the women felt their faking behavior was influenced by what has been portrayed in pornography, as well as in television shows and in movies. An opportunity to discuss the reality of sexual encounters versus the image portrayed in the media would be useful.
Third, there is a need for greater permission for couples to talk about their sexual response, their desires, motives, what feels good, and what they need. The college women interviewed for this study made it clear that sex is not something you can or should talk about with even your most intimate partner. Better role models for communicating and greater emphasis in sexuality education classes on how to approach topics of sexual pleasure are needed to give both women and men permission to talk with their partner.
Conclusion
This research looked at an understudied aspect of women’s sexuality – faking orgasm – from a qualitative perspective. It focused on young women who fake in order to understand the reasons, context, and influences for such behavior. Among these women’s circles of friends, faking orgasm is considered commonplace and normal. Faking orgasm is not new; however, it appears that more women are faking than in prior generations. For college women, faking behavior has increased dramatically over the past 30 years – from less than half to over three-quarters of college women today saying they have faked an orgasm [8]. This increase in faking seems counter-intuitive as the emergence of the third wave of feminism has worked to empower women, and women are becoming much more aware of their own pleasure and their own bodily autonomy. There are a wide variety of reasons women give for faking, and by delving into these reasons, the sexual scripts that women are raised to believe can be better understood. By deciphering these scripts that lead to faking orgasm, researchers can further understand societal pressure, self-pressure, and partner pressure, and work to change that.
This study was unique in that it used a qualitative methodology to investigate the experiences of college women who had faked orgasm in the context of heterosexual relationships. Women faking orgasm appears to be normalized amongst their peer group. Interviews with these 12 college women revealed many themes and suggested that women have similar experiences when it comes to faking orgasm and their sexual scripts. By understanding the scripts that young women who fake orgasm hold onto, along with the context and reasons for faking orgasm, we can further deconstruct the societal implications tied to what “normal sex” is “supposed” to look like and help them have a more honest and pleasurable sexual experience.
References
- Reiner R (1989) When Harry met Sally. MGM Home Entertainment.
- David L, Seinfeld J (1993) Seinfeld/The Mango [Episode 65]. In Seinfeld. NBC.
- Daniels G, Poehler A, Schur M, Wittles H (2011) Parks and Recreation/Ron and Tammy: Part II [Episode 34]. In Parks and Recreation. NBC.
- TMZ (2016) Caitlyn Jenner: Watch me fake an orgasm. I am Cait. TMZ: Los Angeles, California.
- Breslaw A (2017, October 11). 7 Sad but true reasons women fake orgasms. Cosmopolitan.
- Azodi M (2010, October 26). The crazy way I faked it. Cosmopolitan.
- Cooper EB, Fenigstein A, Fauber RL (2014) The Faking Orgasm Scale for Women: Psychometric properties. Archives of Sexual Behavior 43: 423-435. [crossref]
- Caron SL (2021) The sex lives of college students: Three decades of attitudes and behaviors. Orono, ME: Maine College Press.
- Darling CA, Davidson JK (1986) Enhancing relationships: Understanding the feminine mystique of pretending orgasm. Journal of Sex & Marital Therapy 12: 182-196. [crossref]
- Ellison C (2000) Women’s sexualities: Generations of women share intimate secrets of sexual self-acceptance. Publisher’s Group West.
- Fahs B (2014) Coming to power: Women’s fake orgasms and best orgasm experiences illuminate the failures of (hetero) sex and the pleasures of connection. Culture, Health & Sexuality 16: 974-988. [crossref]
- Hite S (1976) The Hite report: A nationwide study of female sexuality. New York: Seven Stories.
- Muehlenhard C, Shippee S (2010) Men’s and women’s reports of pretending orgasm. The Journal of Sex Research 47: 552-567. [crossref]
- Wiederman MW (1997) Pretending orgasm during sexual intercourse: Correlates in a sample of young adult women. Journal of Sex & Marital Therapy 23: 131-139. [crossref]
- Bryan TS (2001) Pretending to experience orgasm as a communicative act: How, when, and why some sexually experienced college women pretend to experience orgasm during various sexual behaviors (Unpublished doctoral thesis). University of Kansas.
- Braun V, Clarke VE, Rogers C (2014) “It feels so good it almost hurts”: Young adults’ experiences of orgasm and sexual pleasure. Journal of Sex Research 51: 503-515. [crossref]
- Kaighobadi F, Shackelford TK, Weekes-Shackelford VA (2011) Do women pretend orgasm to retain a mate? Archives of Sexual Behavior 41: 1121-1125. [crossref]
- Lafrance MN, Stelzl M, Thomas EJ (2016) Faking to finish: Women’s accounts of feigning sexual pleasure to end unwanted sex. Sexualities 20: 281-301.
- Mialon HM (2012) The economics of faking ecstasy. SSRN Electronic Journal 50: 277-285. [crossref]
- Roberts C, Kippax S, Waldby C, Crawford J (1995) Faking it: The story of “ohh!” Women’s Studies International Forum 18: 523-532.
- Fahs B (2011) Performing sex: The making and unmaking of women’s erotic lives. Albany, NY: SUNY Press.
- Harris EA, Hornsey MJ, Larsen HF, Barlow FK (2019) Beliefs about gender predict faking orgasm in heterosexual women. Archives of Sexual Behavior 48: 2419-2433. [crossref]
- Potts A (2000) Coming, coming, gone: A feminist deconstruction of heterosexual orgasm. Sexualities 3: 55-76.
- Future of Sex Education Initiative (2012) National sexuality education standards: Core content and skills K-12. Special issue of the Journal of School Health 1-42.
- Casey E, Masters NT, Morrison DM, Wells EA (2013) Sexual scripts among young heterosexually active men and women: Continuity and change. Journal of Sex Research 50: 409-420. [crossref]
- Lavie-Ajayi M, Joffe H (2009) Social representations of female orgasm. Journal of Health Psychology 14: 98-107. [crossref]
- Weiss S (2017) 4 super real reasons women fake orgasms.
- Maxwell JA (2005) Qualitative research design: An interactive approach (2nd Edition). Thousand Oaks, CA: Sage Publications.