DOI: 10.31038/CST.2017245
Proposal Description
Abstract
Objectives and task definition, based on the state of the art in terms of technology and knowledge. Detailed description of the problem which shall be solved, description of the beneficiary and user of the project results.
Study of the prognostic marker microRNA-Mir-216a/217 in hepatocellular carcinoma patients and development of an autologous vaccine with tumorlysate pulsed dendritic cells, genetically modified for the expression of the Mir-216a/217 and HAb18G/CD147 antigen.
Aim
The aim of the present protocol is the development of the techniques for the detection and quantification of the prognostic marker microRNA-Mir- 216a/217 in serum and liver tissue from hepatocellular carcinoma patients submitted to hepatectomy. Based on the above, an experimental (in vitro) protocol will be developed for the production and differentiation of dendritic cells derived from the peripheral blood of mononuclear cells, genetically modified for the expression of the microRNA-Mir-216a/217 and HAb18G/CD147 antigen and their maturation by the cell lysate from tumor resections of hepatocellular carcinoma patients. The ultimate goals of the present study are the early diagnosis of recurrence of hepatocellular carcinoma and the development of an autologous dendritic cell vaccine for additional immunotherapy of these patients.
Introduction
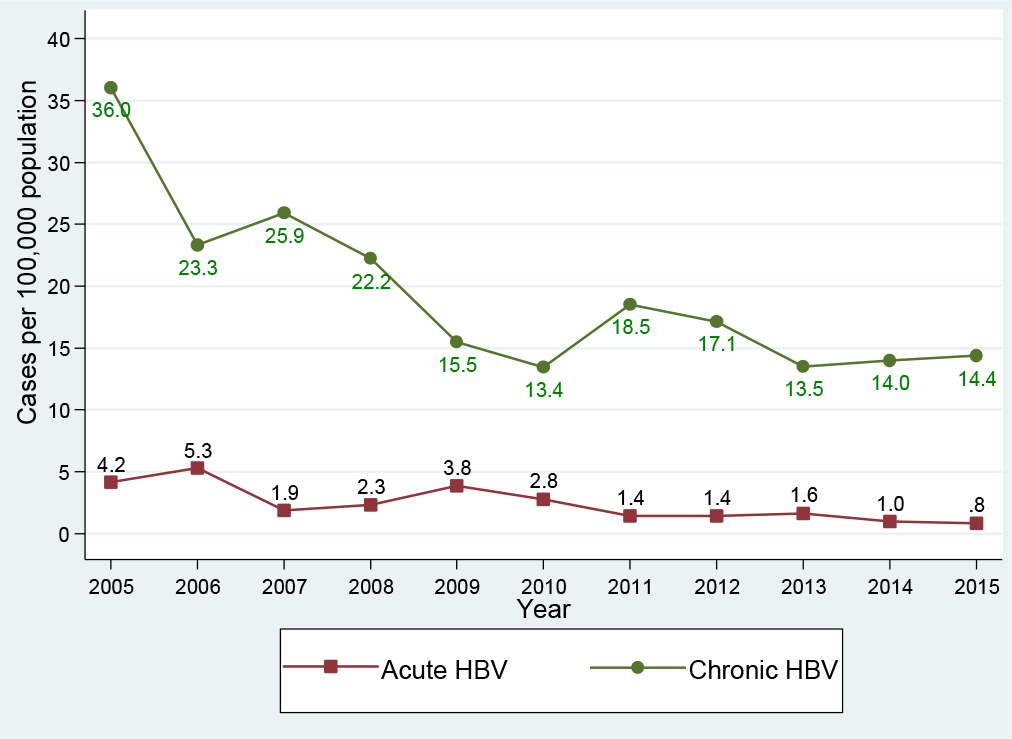
Hepatocellular carcinoma (HCC) is the third leading cause of cancer deaths worldwide with over 600,000 patients dying from this disease annually [1]. The age standardized incidence rates (ASR) of HCC in men in Europe, adjusted to the European Standard Population, is about 8 per 100,000, with a peak in Southern Europe of 10.5 per 100,000 (http://globocan.iarc.fr/). Liver transplantation and tumor resection have proven to be the most effective standard therapies and provide 5-year survival rates of 70% for patients within the Milan criteria, i.e., single tumour < 5 cm in size or up to three tumors < 3 cm in size [2]. These rates reach 50% with radiofrequency ablation and transarterial chemoembolization, which are the next preferred lines of therapy. However, these therapeutic procedures most often do not provide a complete cure, as half of the treated patients experience tumor recurrence within 3 years. A further major problem is that only 30–40% of patients are eligible for the above-described treatments due to the fact that HCC frequently remains undiagnosed until an advanced stage has been reached and occurs in the setting of advanced liver disease due to cirrhosis. These patients have a median survival time ranging from 3 to 16 months [3]. Thus, there is currently ongoing development and testing of alternative drug-based therapies for HCC that target tumor signalling pathways and vasculature. However, so far, the only drug that significantly prolonged survival (by nearly 3 months) in patients with advanced HCC is sorafenib, a multi-targeted tyrosine kinase inhibitor [4]. In view of these facts, new strategies are required. In this study we focus on the identification of predictive molecular factors for HCC recurrence and the development of immunotherapy methods for these patients.
Early Diagnosis of HCC Recurrence with Micro-RNA Techniques
MicroRNAs (miRNAs) are a class of small endogenously expressed non-coding RNAs. The miRNAs in blood, called circulating miRs (cmiRNAs) are potential biomarkers for detecting and monitoring cancer progression [5]. The ability of some miRNAs to function as tumor promoters (miR-30d, miR-151 and miR-210) or suppressors (miR-122, let-7g, miR-29b, miR-193b, miR-194, miR-139 and miR-124) in hepatocarcinogenesis have led to new insights into the molecular pathways involved in HCC [6]. Recently, upregulation of the miR-216a/217 cluster identified to be associated with the early HCC recurrent disease, by comparing the miRNA expression profiles of HCC liver tissue from patients with early-recurrent and non-recurrent disease [7]. In this protocol we intend to develop a technique for the detection and quantification of miR-216a/217 in the blood of HCC patients submitted to liver resection in order to identify recurrence of the disease.
Specific Description of the Proposed Solution
A sensitive and predictable method for the detection and identification of the microRNA216a/217 as the ideal biomarker for prognosis of Hepatocellular Carcinoma
Paraffin-embedded tissue analysis
Paraffin-embedded Hepatocellular Carcinoma (PE-HCC) Tissue samples of the primary tumor are obtained from HCC patients who underwent surgical treatment or biopsy at our centers.
RNA Extraction from serum samples
Total RNA was extracted from 500 μL of serum by using TRI reagent BD (Molecular Research Center). Ten sections, each 10- μm thick, were cut from each PE-HCC block. Deparaffinized tissue sections were digested by using proteinase K, and RNA was extracted by using a modified protocol of the RNAWiz Isolation kit (Applied Biosystems). The RNA was quantified and assessed for purity by using ultraviolet spectrophotometry and the Quant-iT RiboGreen RNA assay kit (Invitrogen) [8,9].
RT-qPCR assay with extracted RNA
10 ng of total RNA extracted from Hepatocellular tumor tissue, normal tissue, or serum are dissolved in 5 μL H2O (2 ng/μL) for reverse transcription with the addition of 5 μL of a reaction mixture containing 5Χ first strand buffer, 10 mmol/L deoxynucleoside-5’- triphosphate, RNasin, reverse transcriptase, and miR-specific RT primers (Exiqon). After the mixture was incubated in 37°C for 2 h, the transcribed specific cDNA was diluted 10-fold with molecular grade H2O before use as a qPCR template. Each qPCR contained 2.5 μL of diluted cDNA, 5 μL of 2ΧPerfeCTa SYBR Green FastMix for iQ (Quanta Bioscience), miR-specific, locked nucleic-acid– based forward primer targeting the specific microRNA216a/217 and universal reverse primer (Exiqon).
RT-qPCR directly in serum
This assay requireσ only a small aliquot of serum. To deactivate or solubilize proteins that might inhibit the RT-qPCR, 2.5_L of each serum sample are mixed with 2.5 μL of a preparation buffer that contained 2.5% Tween 20 (EMD Chemicals), 50 mmol/L Tris (Sigma- Aldrich), and 1 mmol/L EDTA (Sigma-Aldrich). 5 μL ofRT reagent mixture are added which contain the same RT reagents used for RT-qPCR with extracted RNA RNA, directly to 5 μL of serum in preparation buffer; a 2-h incubation at 37°C is followed by a 5-min enzyme inactivation at 95°C. The transcribed cDNA is diluted 10- fold by H2O and then centrifuged at 9000 g for 5 min to eliminate the protein precipitant. A 2.5-μL volume of the supernatant cDNA solution is used as the template for qPCR. qPCR conditions, primers and reagents, and data analysis were duplicated for those described in RT-qPCR with extracted RNA section.
Real time quantitative PCR (qPCR)
Real-time qPCRs were performed using SYBR Green PCR Master Mix and 7300 Realtime PCR System (Applied Biosystems, Foster City, CA USA). Real-time qPCRs were also used to detect miRs, as reported [10]. Sequences of miR-specific primers for cDNA synthesis and reverse primers for miR-216a were: 5′-CATGATCAGCTGGGCCAAGACACAGTTGCCAGCTG-3′ and 5′-TAATCTCAGCTGGCAA-3′. Primers for miR-217 were: 5′ CATGATCAGCTGGGCCAAGAATCCAGTCAGTT-3′ (cDNA synthesis) and 5′-TACTGCATCAGGAACT-3′ (reverse primer). miR expression levels were also confirmed by poly-adenylation of mature miR and cDNA synthesis primed by oligo-dT primer tagged with universal primer sequence (miScript System, Qiagen). cDNA was amplified using miR specific and universal primers. For miR-216a and miR-217 PCRs, the same reverse primers mentioned above and the primers provided by Qiagen were used as miR-specific primers. 5S RNA or 18S RNA served as internal control (Ambion) [7]. Genetically modified dendritic cells.
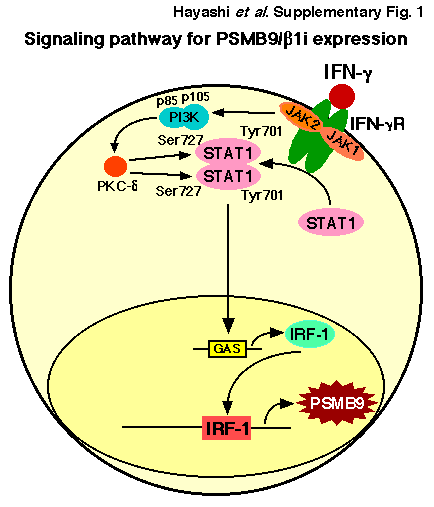
The limited improvements in clinical outcomes with dendritic cells loaded with tumor associated antigens (TAAs) led to trials with genetically modified DCs to further enhance antigen presentation and immunostimulation N. Recent studies have shown that the miR- 216A/217 cluster is consistently and significantly up-regulated in HCC tissue samples and in cell lines associated with early tumor recurrence, poor disease free survival and an epithelial mesenchymal transition (EMT) phenotype [7-31]. Stable over-expression of miR-216a/217- induced EMT, increased the stem like cell population, migration and metastatic ability of epithelial HCC cells. PTEN and SMAD7 are subsequently identified as two functional targets of miR-216a/217, and both PTEN and SMAD7 are down regulated in HCC. Ectopic Expression of PTEN or SMAD7 partially rescued miR216a/217 mediated EMT phenotype, cell migration and stem-like properties in HCC cells. Previously was shown that SMAD7 is a TGF-β1 antagonist. Recently, it has been also shown that Epithelial–mesenchymal transition (EMT) induced by transforming growth factor-β (TGF-β) is implicated in hepatocarcinogenesis and hepatocellular carcinoma (HCC) metastasis [32]. On the other hand, HAb18G/CD147, which belongs to the CD147 family, is an HCC-associated antigen that has a crucial role in tumor invasion and metastasis. Upregulation of HAb18G/CD147 is induced by TGF-β coupled promoting the idea that CD147 may be a potential target for the treatment and prevention of HCC. Other studies have also shown that overexpression of miR216a/217 act a positive feedback regulator for the TGF-b pathway and the canonical way involved in the activation of the PI3K/Akt/ Mtor in HCC cells [33,34].
These facts led us to the second proposal of our protocol:
Experimental (in vitro) protocol for the production and differentiation of dendritic cells derived from the peripheral blood fraction of mononuclear cells, genetically modified for the expression of the microRNA-Mir-216a/217 and HAb18G/CD147 antigen and their maturation by the cell lysate from tumor resections of hepatocellular carcinoma patients
1. MS2 VLP-based delivery of microRNA-216a/217 as a potential delivery approach for the production of clinical grade genetically modified monocyte derived dendritic cells for the immunization of patients suffered from Hepatocellular Carcinoma
Recent studies suggest that microRNA-216a/217 microRNA (miR-216a/217) plays an essential role in immunoregulation and may be involved in the pathogenesis of Hepatocellular Carcinoma. Therefore, it is of interest to investigate the potential therapeutic application of miR-216a/217-induced dendritic cells in Hepatocellular Carcinoma, a concept that has not been thoroughly investigated thus far. Virus-like particles (VLPs) are a type of recombinant nanoparticle enveloped by certain proteins derived from the outer coat of a virus. Herein, we describe a novel miRNA-delivery approach via bacteriophage MS2 VLPs and investigate the therapeutic effects of miR–216a/217-induced dendritic cells against patients suffering from Hepatocellular Carcinoma.
2. An Innovative Methodology for the miR216a/217 MicroRNA Delivery in peripheral blood monocyte derived antigen presenting dendritic cells via magnetic nanoparticles
Peripheral Blood Monocyte derived dendritic cells show promising potential in the vaccination of HCC patients. Recently, gene silencing strategies using microRNAs (miR) emerged with the aim to expand the therapeutic potential of genetically modified dendritic cells. However, researchers are still searching for effective miR delivery methods for clinical applications. Therefore, we aimed to develop a technique to efficiently deliver miR216a/217 microRNA into patient’s dendritic cells with the help of a magnetic non-viral vector based on cationic polymer polyethylenimine (PEI) bound to iron oxide magnetic nanoparticles (MNP), whose uptake efficiency and cytotoxicity will be determined by flow cytometry. The Present Proposal is directed in different magnetic complex compositions and determined. Additionally, the present proposal is focusing on the monitoring of the release, processing and functionality of delivered miR216a/217 microRNA with confocal laser scanning microscopy, real-time PCR and live cell imaging, respectively. On this basis, we will focus on the established parameters for construction of magnetic non-viral vectors with optimized uptake efficiency (~75%) and moderate cytotoxicity in patients peripheral blood monocyte derived dendritic cells. Furthermore, we aim to introduce the magnetic non-viral vector based on cationic polymer polyethylenimine (PEI) transfection as a long term beneficial strategy for the successful genetic modification of the HCC-TAAs presenting dendritic cells against Hepatocellular Carcerous cells for future in vivo applications.
Generation of peripheral blood monocyte-derived miR-216a/217 induced DCs
Monocyte-derived DCs from Hepatocellular Carcinoma Patients (obtained with following informed consent and approved by our institutional review board) are generated. In brief, peripheral blood mononuclear cells (PBMCs) are prepared from whole blood by Ficoll density-gradient centrifugation. The PBMCs are suspended in tissue culture flask in RPMI 1640 supplemented with 1% heat inactivated autologous serum for 60 minutes at 37°C to allow for adherence. The nonadherent cells are removed and the adherent cells are cultured overnight. To generate immature miR-216a/217 induced DCs (DCs), the nonadherent and loosely adherent cells are collected the following day and placed in RPMI 1640 medium containing 1% heat-inactivated autologous serum, 1000 U/ml recombinant human GM-CSF (Becton Dickinson, Bedford, MA, USA), and 500 U/ml recombinant human IL-4 (Becton Dickinson) for 6 days. In order to assess the effects of HCCsp on miR-216a/217 induced DCs generation, we are focusing on the creation of four types of miR-216a/217 induced preparation: 1) miR-216a/217 induced DCs; 2) miR-216a/217 induced s generated in the presence of HCCsp during the entire culture period (DCs/sp); 3) miR-216a/217 induced DCs exposed to 0.1 KE/ml (0.1 KE equals of 0.01 mg of dried streptococci) penicillin-inactivated Streptococcus pyogenes (OK-432) (Chugai Pharmaceutical) for 3 days (OK- miR- 216a/217 induced DCs) as described previously; 4) OK- miR-216a/217 induced s generated in the presence of HCCsp during the entire culture period (OK-DCs/sp). Four types of miR-216a/217 induced are generated in the presence of equal amounts of GM-CSF and IL-4 during the entire culture.
To generate monocyte-derived miR-216a/217 induced DCs for vaccination, PBMCs derived from the HCC patient are freshly isolated (obtained with following informed consent and approved by our institutional review board). Autologous miR-216a/217 induced s are generated in RPMI 1640 medium containing 1% heat-inactivated autologous serum, 1000 U/ml recombinant human GM-CSF, 500 U/ml recombinant human IL-4, and 10 ng/ml recombinant TNF-α (Becton Dickinson) [30]. On day 6 of culture, DCs harvested from the nonadherent and loosely adherent cells are used for fusion. The firmly adherent monocytes are harvested and used as an autologous target for the CTL assays.
HCC Patient selection
The clinical trial protocol will be approved by the Institutional Review Boards of our University Hospitals. Patients will be informed of the investigative nature of this study, and written consent in accordance with institutional regulations is obtained prior to study entry. Eligibility criteria included HCC patients submitted to liver resection or biopsy and transarterial chemoembolization (TACE) with radiological diagnosis of primary HCC by computed tomography (CT), classified in stage II and III according to the tumor-node-metastasis (TNM) classification; age over 20 years/both male and female; Eastern Cooperative Oncology Group scale 0–1; and indicators of acceptable hematological (hemoglobin ≥8.5 g/dl, white blood cells ≥2,000/mm3, platelet ≥50,000/mm3), hepatic (Child Pugh score ≤7, alanine aminotransferase, aspartate aminotransferase ≤5x upper normal limit) and renal (creatinine ≤1.5 mg/dl) function. Important exclusion criteria consisted of organ transplantation; a medical history of autoimmune disease, immunodeficiency, or autoimmune disease that might be aggravated by immunotherapy; not exceeding 2 weeks after antibiotic treatment needed due to a serious infectious disease; seropositivity for human immunodeficiency virus antigen; use of immunosuppressive drug such as cyclosporin A and azathioprine; any cardiopulmonary disability judged by the investigator; a medical history of psychological disease or epilepsy; and evidence of another active malignant neoplasm.
Autologous DC generation
DCs are generated from blood monocytes, as reported previously, with modifications. White blood cells obtained from the HCC patients through leukapheresis. DCs are prepared in a GMP-compliant facility at our hospitals. Peripheral blood mononuclear cells (PBMCs) are separated from WBC by Ficoll-Paque™ PLUS (Amersham Biosciences, Uppsala, Sweden) density gradient centrifugation. PBMCs are stored in a liquid nitrogen tank until necessary for DC generation. PBMCs thawed, ished with Hanks’ Balanced Salt Solutions, resuspended in RPMI-1640 medium (Lonza, Basel, Switzerland) supplemented with autologous heat-inactivated plasma, and then incubated in CellSTACK Culture Chambers (Corning, Corning, NY, USA). After 0.5–1 h incubation at 37°C in a 5% CO2 incubator, non-adherent cells are removed by gentle ishes.
The adherent monocytes are cultured in X-VIVO15 (Cambrex, East Rutherford, NJ, USA) supplemented with 100 ng/ml of granulocyte macrophage-colony stimulating factor (GMP grade: LG Life Science, Seoul, Korea) and 300 ng/ml of interleukin (IL)-4 (JW CreaGene Inc., Seongnam, Korea) for 5 days. On day 5, nonattached immature DCs are harvested and pulsed with CTP-fused human AFP, MAGE-1 and GPC-3 recombinant proteins at a final concentration of 5 μg/ml each. Antigen-pulsed dendritic cells are matured in the presence of cytokine cocktail, IL-6 (Peprotech, Rocky Hill, NJ, USA), IL-1β (Peprotech), tumor necrosis factor (TNF)-α (Peprotech), prostaglandin E2 (PGE2) (Sigma Chemical Co., St. Louis, MO, USA), interferon (IFN)-γ (LG Life Science), OK432 (Chugai Pharmaceutical Co., Tokyo, Japan), and poly I: C (Sigma) for 1 or 2 days depending on surface phenotypes and cell population. On day 6–7, the DCs are harvested, ished, and resuspended in 1.2 ml of cryopreserving solution containing 5% dimethyl sulfoxide (Bioniche Pharma USA, Lake Forest, IL, USA). Finally fully equipped DCs are packed into a sterile glass vial (4×107 cells/vial), sealed with a snap-cap, and stored at an ultralow freezer for >12 h.
Quality control of dendritic cell vaccine
Safety test
For safety, endotoxin, germ-free and mycoplasma-free tests are performed according to the KFDA-approved JW CreaGene standard and test guidelines. Endotoxin is evaluated using gel-clot techniques. The endotoxin of the product should be less than 10 EU/ml per 1.2- ml vial. Mycoplasma test is performed by both direct culture and PCR methods using e-Myco™ Mycoplasma PCR detection kit (Intron Biotechnology, Seongnam, Korea), which contains primer sets specifically designed to detect major contaminants of Mycoplasma in cell cultures such as M. arginini, M. faucium, M. fermentans,M. hyorhinis, M. orale, and A. laidlawii as well as other broad spectrum of mycoplasma.
Cell size and granularity
During the differentiation from monocytes to miR-216a/217 induced dendritic cells, cell size and granularity increase. Based on these principles, the cell size and granularity of each miR-216a/217 induced DC vaccine are assessed by flow cytometric analysis. PBMCs are used for gating control.
Phenotypic analysis
The phenotype of miR-216a/217 induced DC vaccine is determined by flow cytometry using a FACSCalibur™ flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA). The following monoclonal antibodies are used: i) fluorescein isothiocyanate-conjugated mouse antihuman IgG2a isotype control; ii) phycoerythrin-conjugated mouse antihuman IgG1 isotype control; iii) anti-CD14, anti-CD19, anti-CD40, anti-CD80, anti-D86, anti-HLA-ABC, and anti-HLA-DR (BD Pharmingen, San Diego, CA, USA).
Viability
The viability of miR-216a/217 induced DC vaccine is assessed by propidium iodide (PI) staining. PI (BD Pharmingen) is added to a sample and kept in the dark at room temperature for 20 min. Cell viability is examined by flow cytometry using a FACSCalibur™ (Becton Dickinson). Viability is represented as 100-[(PI+ of sample)−(PI+ of control)] (%).
Lymphocyte proliferation assay
One vial from each miR-216a/217 induced DC vaccine lot is used to test of T cell stimulation capacity according to the standard lymphocyte proliferation assay. T cells are isolated from cryopreserved PBMC using nylon wool column (Polysciences, Warrington, PA, USA). Purified T cells (1×105) are cultured with serially diluted DC vaccine (starting from 1×104 cells to 0.33×103 cells) at 37°C for 5 days. T cell proliferation is assessed by 3-(4,5-di-methylthiazol-2-yl)-2,5- diphenyltetrazolium bromide, yellow tetrazole: MTT) assay following manufacturer’s protocol (CellTiter 96 Non-Radioactive proliferation assay kit; Promega, Madison, WI, USA). R2 represent the standard curve of MTT assay for the validation of a data set.
Cytokine production assay
Either culture supernatant of each antigen-pulsed miR-216a/217 induced DC or co-cultured medium of T cells/ miR-216a/217 induced DC at the ratio of 10: 1 is collected and stored at −80°C until this assay. The concentration of IL-12p70, IL-10, IFN-γ, and IL-4 is measured with corresponding human immunoassay kits (BD OptEIA™ kit, BD Pharmingen) based on the manufacturer’s instruction. Each experiment is performed 3 times and the result is described as the mean ± standard deviation.
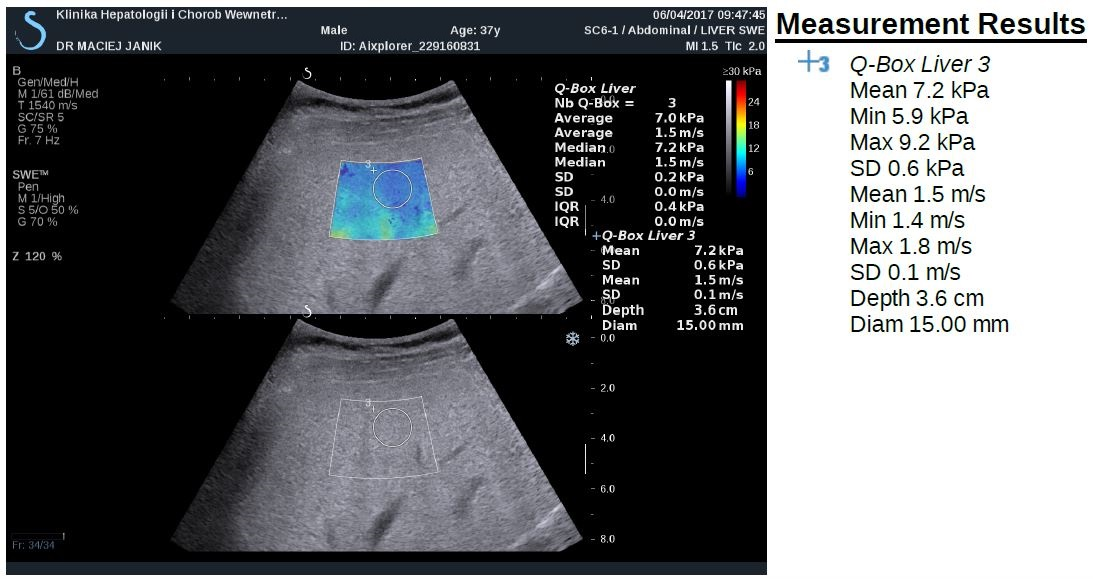
Treatment protocol of Hepatocellular Carcinoma Patients
The screening evaluation shall be performed in 3 weeks before the start of dendritic cell-based immunotherapy and consisted of the following: complete history, thorough physical examination, chest X-ray, electrocardiogram, urine analysis, hematological and immunological parameters, serum chemistry, tumor markers [AFP and protein induced by vitamin K absence or antagonists-II (PIVKA-II)], ultrasonography and abdominal CT scan. Eligible HCC patients underwent liver resection or TACE and biopsy, 2 weeks before the start of the vaccination. PBMC collection by leukapheresis is performed 1 week before the first planned vaccination. Tumor antigen-pulsed miR-216A/217 Professional Antigen Presenting DCs are injected intravenously in 20 mL of phosphate-buffered saline over 10 minutes on day 12. Patients were observed for 2 hours after each vaccination to assess any immediate complications. During the first cycle, 6 vaccinations are administered at biweekly intervals. Medical history and standard blood tests and urine analysis are performed at each vaccination. Vital signs are monitored during and after each injection. Response evaluation is performed 4 weeks after fourth vaccination (10 weeks after first vaccination). Two further vaccinations are administered at biweekly intervals, and final response evaluation is performed at 18 weeks after first vaccination. Tumor markers, including qRT-PCR miR-216A/217, and serological tests for autoantibodies, including anti-nuclear antibody, are evaluated every 4 weeks.
Clinical response and toxicity assessment
Clinical responses to vaccination are evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST) criteria. Complete response is defined as disappearance of all target lesions. Partial response is defined as 30% decrease in the sum of the longest diameter of target lesions. Progressive disease is 20% increase in the sum of the longest diameter of target lesions. Stable disease is defined as small changes that do not meet above criteria. Toxities are classified according to the National Cancer Institute Common Toxicity Criteria.
Description of the German and Greek partners from higher education institutions, research establishments and commercial companies who are involved in the project (key competencies, capabilities, infrastructure, etc).
The Division of Transplantation, Department of Surgery, Aristotle University of Thessaloniki Medical School is the leading center in Greece, performing liver transplantation and liver surgery in patients with hepatocellular carcinoma and has the ability to perform clinical studies on the prognosis and therapy on this subject.
The Department of Surgery, Essen University Hospital, is a leading center worldwide in liver transplantation and liver surgery in patients with hepatocellular carcinoma and has performed many multi institutional clinical studies on the prognosis and therapy on this subject.
Justify the scope of the collaboration between the partners of both countries and the mutual benefit provided through this collaboration. Overview of previous contacts in and collaborations with the partner country.
Immunotherapy of HCC
Immunotherapy aims to provide a more efficient and selective targeting of tumor cells by inducing or boosting the existing tumor-specific immune response. The rationale for immunotherapy for HCC is based on several lines of evidence of a protective role the immune system, e.g., by controlling tumor growth. First, HCC patients with an intratumoral accumulation of lymphocytes had a superior 5-year survival rate and a prolonged recurrence-free survival after liver transplantation or resection [11,12]. A certain level of protection was especially conferred by cytotoxic CD8+ T cells [11]. Of note, these tumor infiltrating lymphocytes (TILs) were associated with an inflammatory microenvironment that was a predictor of overall patient survival, indicating a protective role of TILs in HCC [13,14]. Furthermore, a strong CD8+ T cell response against several tumor-associated antigens (TAAs) was found to coincide with improved recurrence-free survival after liver resection [15]. The important role of CD8+ T cells in HCC control is further supported by a study in mice. It was shown that interferon γ (IFNγ) produced by CD8+ TILs could be one effector mechanism for apoptosis of hepatoma cells [16]. These data imply a central role of T cells in modulating tumor progression and provide strong justification for T cell immunotherapy.
Immunotherapy approaches for HCC
A limited number of immunotherapy trials for HCC have been conducted based on several strategies, with yet modest results. Cytokines have been used to activate subsets of immune cells and/or increase the tumor immunogenicity [17,18]. Further strategies have been based on infusion of tumor infiltrating lymphocytes or activated peripheral blood lymphocytes [19-21]. Alternatively, direct delivery of genetically modified or designer T cells (dTc) into the hepatic artery has been recently proposed as a promising novel strategy and is currently evaluated in a phase I human clinical trial (ClinicalTrials. gov Identifier: NCT01373047). Indeed, the latter strategy has recently been successfully used for treatment of different cancers and several human clinical trials are currently ongoing [22].
Alternatively, considering active immunotherapy strategies (i.e. therapeutic vaccination), the number of human clinical trials published to date is extremely small. The first HCC vaccine clinical trial was conducted by Butterfield et al. based on CD8+ T cell epitopes specific for alpha fetoprotein (AFP), showing the generation of AFP-specific T cell responses in vaccinated subjects [23]. To improve the immune response, the same authors performed a subsequent phase I/II trial administering AFP epitopes presented by autologous DCs loaded ex vivo. This treatment, however, resulted only in transient CD8+ T cell responses, possibly caused by the lack of CD4+ help [24,25]. To overcome this limitation and to increase the number of tumor associated antigens (TAAs) targeted by the immune response elicited by the vaccine, few vaccine approaches based on autologous DCs pulsed ex vivo with a lysate of the autologous tumor [26] or of hepatoblastoma cell line HepG2 [27,28] have been evaluated in human clinical trials, showing limited improvements in clinical outcomes . The last clinical trial in the literature is based on a combination of low dose cyclophosphamide treatment followed by a telomerase peptide (GV1001) vaccination which did not show antitumor efficacy [29].
Prospects for the success of the proposed measures and implementation concepts describing how the project outcomes can be utilized after the funding period (utilization plan)
Dendrigenea: A manufacturing patient-specific cell therapy product
Overview and case study of dendrigenea’s cell therapy technology: Our Dendrigenea cellular therapy product is currently progressing through clinical development with the potential to address unmet medical needs affecting millions of patients suffered from cancer –tumor related diseases. Dendrigenea is an autologous cell-based therapeutic product which has already received regulatory approval and reach the market. Our primary challenge is to quickly become a Leader dendritic cell manufacturing facility of such products in sufficient volume to meet patients demand.
Biogenea Pharmaceuticals Ltd has developed a cancer-specific dendritic cell therapy technology for use in an autologous patient-specific vaccine therapy and is conducting late-stage clinical trials both in Greece and other Countries from Southeaster Europe. Dendritic cells are derived from a patient’s own peripheral blood and processed through a short four-week isolation, maturation, culture and fusion procedure under media perfusion conditions that lend potent functional anti-cancer vaccination properties to the final vaccine-cell product.
Development and clinical use of a Peripheral Monocyte Derived Cell Therapy Product (PMDCTP) such as Dendrigenea has raised unique manufacturing challenges that we have addressed through a series of patented innovative solutions, many of which could have broad application in the field of cancer immunotherapy for the production of commercial-scale dendritic cell based manufacturing Vaccines.
Peripheral Blood as a source of dendritic vaccines has key advantages for patients. In particular, autologous (PMDCTP) (treatments derived from a patient’s own monocytes) has a favorable safety and risk profile not available from allogeneic (universal donor) therapies.
Concerns over immune rejection and disease transmission are minimal. In addition, short-term culture and monocyte maturation procedures reduce the risk of tumorgenic transformation, which is possible in universal donor cell products typically generated from longer-term serially passaged cultures. Dendrigenea has demonstrated a high level of safety in more than 250 patients treated successfully for a variety of tumor-cancer related medical indications, with both local and systemic administration, showing no sign of cell-related adverse events.
Our dendritic cells are expanded from cell populations existing within patient’s own peripheral blood that are associated with natural cell immune response and tissue homeostasis as well as healing. Local transplantation of these expanded, patient-specific peripheral blood derived dendritic cells are expected to immunize patients suffering from Tumor related diseases. They are currently under clinical evaluation for a range of cancer cell treatments including Melanoma, Leiomyosarcoma, Glioma, Glioblastoma, Neuroblastoma and Ovarian, Breast Cancer.
Dendrigenea goes through of an ex-vivo, culture, maturation and cell fusion process have been developed to expand specific subpopulations of primary monocyte derived dendritic cells found within patient’s own peripheral blood, including early stem and progenitor cells, without triggering cell differentiation to other malignant tissue specific cell-lines . The result is a mixed population of dendritic cells genetic or not modified targeted directly to patient’s own cancer cells.
References
- Schütte K, Bornschein J, Malfertheiner P (2009) Hepatocellular carcinoma–epidemiological trends and risk factors. Dig Dis 27: 80-92. [crossref]
- Llovet JM, Bruix J (2008) Molecular targeted therapies in hepatocellular carcinoma. Hepatology 48: 1312-1327. [crossref]
- Llovet JM, Burroughs A, Bruix J (2003) Hepatocellular carcinoma. Lancet 362: 1907-1917.
- [crossref]
- Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, et al. (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359: 378-390. [crossref]
- Asaga S, Hoon DS (2013) Direct serum assay for microRNA in cancer patients. Methods Mol Biol 1024: 147-155. [crossref]
- Giordano S, Columbano A (2013) MicroRNAs: new tools for diagnosis, prognosis, and therapy in hepatocellular carcinoma? Hepatology 57: 840-847. [crossref]
- Xia H, Ooi LL, Hui KM (2013) MicroRNA-216a/217-induced epithelial-mesenchymal transition targets PTEN and SMAD7 to promote drug resistance and recurrence of liver cancer. Hepatology 58: 629-641. [crossref]
- Asaga S, Kuo C, Nguyen T, Terpenning M, Giuliano AE, et al. (2011) Direct serum assay for microRNA-21 concentrations in early and advanced breast cancer. Clin Chem 57: 84-91. [crossref]
- Takeuchi H, Morton DL, Kuo C, Turner RR, Elashoff D, et al. (2004) Prognostic significance of molecular upstaging of paraffin-embedded sentinel lymph nodes in melanoma patients. J Clin Oncol 22: 2671-2680. [crossref]
- Xia H, Cheung WK, Sze J, Lu G, Jiang S, et al. (2010) miR-200a regulates epithelial-mesenchymal to stem-like transition via ZEB2 and beta-catenin signaling. J Biol Chem 285: 36995-37004. [crossref]
- Unitt E, Marshall A, Gelson W, Rushbrook SM, Davies S, et al. (2006) Tumour lymphocytic infiltrate and recurrence of hepatocellular carcinoma following liver transplantation. J Hepatol 45: 246-253. [crossref]
- Gao Q, Qiu SJ, Fan J, Zhou J, Wang XY, et al. (2007) Intratumoral balance of regulatory and cytotoxic T cells is associated with prognosis of hepatocellular carcinoma after resection. J Clin Oncol 25: 2586-2593. [crossref]
- Hirano S, Iwashita Y, Sasaki A, Kai S, Ohta M, et al. (2007) Increased mRNA expression of chemokines in hepatocellular carcinoma with tumor-infiltrating lymphocytes. J Gastroenterol Hepatol 22: 690-696. [crossref]
- Chew V, Tow C, Teo M, Wong HL, Chan J, et al. (2010) Inflammatory tumour microenvironment is associated with superior survival in hepatocellular carcinoma patients. J Hepatol 52: 370-379. [crossref]
- Hiroishi K, Eguchi J, Baba T, Shimazaki T, Ishii S, et al. (2010) Strong CD8 (+) T-cell responses against tumor-associated antigens prolong the recurrence-free interval after tumor treatment in patients with hepatocellular carcinoma. J Gastroenterol 45: 451-458. [crossref]
- Komita H, Homma S, Saotome H, Zeniya M, Ohno T, et al. (2006) Interferon-gamma produced by interleukin-12-activated tumor infiltrating CD8+T cells directly induces apoptosis of mouse hepatocellular carcinoma. J Hepatol 45: 662-672. [crossref]
- Reinisch W, Holub M, Katz A, Herneth A, Lichtenberger C, et al. (2002) Prospective pilot study of recombinant granulocyte-macrophage colony-stimulating factor and interferon-gamma in patients with inoperable hepatocellular carcinoma. J Immunother 25: 489-499. [crossref]
- Sangro B, Mazzolini G, Ruiz J, Herraiz M, Quiroga J, et al. (2004) Phase I trial of intratumoral injection of an adenovirus encoding interleukin-12 for advanced digestive tumors. J Clin Oncol 22: 1389-1397. [crossref]
- Shi M, Zhang B, Tang ZR, Lei ZY, Wang HF, et al. (2004) Autologous cytokine-induced killer cell therapy in clinical trial phase I is safe in patients with primary hepatocellular carcinoma. World J Gastroenterol 10: 1146-1151. [crossref]
- Takayama T, Makuuchi M, Sekine T, Terui S, Shiraiwa H, et al. (1991) Distribution and therapeutic effect of intraarterially transferred tumor-infiltrating lymphocytes in hepatic malignancies. A preliminary report. Cancer 68: 2391-2396. [crossref]
- Takayama T, Sekine T, Makuuchi M, Yamasaki S, Kosuge T, et al. (2017) Adoptive immunotherapy to lower postsurgical recurrence rates of hepatocellular carcinoma: a randomised trial. Lancet 356:802-7.
- Essand M, Loskog AS (2013) Genetically engineered T cells for the treatment of cancer. J Intern Med 273: 166-181. [crossref]
- Butterfield LH, Ribas A, Meng WS, Dissette VB, Amarnani S, et al. (2003) T-cell responses to HLA-A*0201 immunodominant peptides derived from alpha-fetoprotein in patients with hepatocellular cancer. Clin Cancer Res 9: 5902-5908. [crossref]
- Butterfield LH, Ribas A, Dissette VB, Lee Y, Yang JQ, et al. (2006) A phase I/II trial testing immunization of hepatocellular carcinoma patients with dendritic cells pulsed with four alpha-fetoprotein peptides. Clin Cancer Res 12:2817-25.
- Bray SM, Vujanovic L, Butter field LH (2011) Dendritic cell-based vaccines positively impact natural killer and regulatory T cells in hepatocellular carcinoma patients. Clin Dev Immunol 2011: 249281. [crossref]
- Lee WC, Wang HC, Hung CF, Huang PF, Lia CR, et al. (2005) Vaccination of advanced hepatocellular carcinoma patients with tumor lysate-pulsed dendritic cells: a clinical trial. J Immunother 28: 496-504. [crossref]
- Palmer DH, Midgley RS, Mirza N, Torr EE, Ahmed F, et al. (2009) A phase II study of adoptive immunotherapy using dendritic cells pulsed with tumor lysate in patients with hepatocellular carcinoma. Hepatology 49: 124-132. [crossref]
- El Ansary M, Mogawer S, Elhamid SA, Alwakil S, Aboelkasem F, et al. (2013) Immunotherapy by autologous dendritic cell vaccine in patients with advanced HCC. J Cancer Res Clin Oncol 139: 39-48. [crossref]
- Greten TF, Forner A, Korangy F, N’Kontchou G, Barget N, et al. (2010) A phase II open label trial evaluating safety and efficacy of a telomerase peptide vaccination in patients with advanced hepatocellular carcinoma. BMC Cancer 10: 209. [crossref]
- Morrison BJ, Steel JC, Gregory M, Morris JC (2009) Genetically Modified Dendritic Cells in Cancer Immunotherapy. In Shurin MR, Salter RD, “Dendritic Cells in Cancer”, Springer 23: 347-363.
- Blechacz B, Mishra L (2013) Hepatocellular carcinoma biology. Recent Results Cancer Res 190: 1-20. [crossref]
- Wu J, Ru NY, Zhang Y, Li Y, Wei D, et al. (2011) HAb18G/CD147 promotes epithelial-mesenchymal transition through TGF-β signaling and is transcriptionally regulated by Slug. Oncogene 30: 4410-4427. [crossref]
- Shen J, Stass SA, Jiang F (2013) MicroRNAs as potential biomarkers in human solid tumors. Cancer Lett 329: 125-136. [crossref]
- Gao Q, Shi Y, Wang X, Zhou J, Qiu S, et al. (2012) Translational medicine in hepatocellular carcinoma. Front Med 6: 122-133. [crossref]