Abstract
One of the lead physicians defending the “United States Public Health Service Study at Tuskegee of Untreated Syphilis in the Negro Male” was Dr. John C. Cutler. His defense of the study was (roughly) because the benefits to society in general, and the black community in particular, far outweighed any corresponding risks or harms. His moral judgment controverted the large number of thoughtful essayists decrying the Study as a straightforwardly and racist dehumanizing of men, women, and families. In this essay, I seek to show two things. First, I seek to show how an action or event done at a particular time may lack the objectivity that comes with distanciation, thus a (malicious) systemic distortion may be ambiguously reducible to a historical error, especially if there is no critical theory borne from critical reflection to hold the action or event morally accountable. Second, I show how two things should be apparent with disambiguation of the historical narrative and with critical reflection: 1) an ethic of ambiguity (and the integrity thereof) should demand that moral propositions be critically assessed at the time of an action or event from more than one angle to ensure the protection of all humans, especially historically marginalized individuals and groups; 2) an ethic of belief, given its Intentionality and intentions, should understand its inherent vulnerabilities and accentuate the import of evidence in moral epistemology.
Keywords
Ethics of Belief, Ethics of Ambiguity, Intentionality, Moral Epistemology, Syphilis Study, Tuskegee, USPHS
A young boy and his mother stood viewing a museum art piece depicting a man slaying a lion. Looking incredulous, the boy argued, “Mama, everyone knows that a man can’t beat a lion.” The mother prudentially responded, “Yes, but remember son, it was a man who painted the picture.” – anonymous source
…there can be mutual reinforcement between an explanation and what it explains. Not only does a supposed truth gain credibility if we can think of something that would explain it, but also conversely: an explanation gains credibility if it accounts for something we supposed to be true. – Quine and Ullian The Web of Belief.
Introduction
There is a uniquely discursive and unexpected feature of the notorious United States Public Health Service Study on the effect of Untreated Syphilis on the Negro Male at Tuskegee (the Study), one that points to either a weakness in the structure of ethical arguments or the propensity of agents to put forth invalid ethical arguments due to an accentuation of fallacious propositions, maniacal beliefs, or justifiable ambiguities. This paper shows that an in-principle attempt to justify the treatment (or non-treatment, as it were) of 623 Negro men (and their families) survives no credible moral epistemology or justification, cannot rely on an ethic of ambiguity to demonstrate its veracity, and cannot avoid its inherent racism. We are almost five decades since the Study, and almost nine decades since its inception. Given this near half-century of critical reflection, analysis, and moral inferences, I look at the force of predominant ethical theories to see whether an ethic of ambiguity is a sustainable defense for the Study’s protagonists.
In this essay, I use Dr. John Cutler as a symbol of the primary protagonists. Born in 1915, Dr. John Cutler, finished Western Reserve University Medical School in 1941 at the age of 26, and one year later, ten years after the Study began, started his career at the United States Public Health Service—the government organization that authorized the Study. His participation in the Study as one of the primary doctors, his furtherance of a similar study in Guatemala, and his unswerving commitment and defense of the Study decades after its public revelation, are all indicative of why he surmounts several others as the Study’s protagonist. There’s a prima facie sense in which his words can be perceived as genuine empathy: “The Tuskegee Study has been grossly misunderstood and misrepresented this way. And the fact was it was (our) concern for the black community, trying to set the stage for the best public health approach possible and the best therapy, that led to the Study being carried out” [2]. Defensive terms like “grossly misunderstood,” “misrepresented,” “concern for,” “best…approach,” and “best therapy” suggest the deep lack of empathy and care that the United States Public Health Service visited upon the families of Macon County, Alabama between 1932 and 1972 [3]. If Dr. Cutler is correct, that ambivalence surrounding the Study was only a gross “misunderstanding” and that there was nothing duplicitous about it, then the last half-century of critical analysis amounts to nothing more than the subjective misinterpretation that is (potentially) commonplace to all historical events. The “historical events” to which I refer are those events that come into being—that occur—due to actions caused by Intentional mental states (beliefs) and intentional (deliberate) actions. In this regard, I am not referring to anything environmental; [4] rather; I am referring to a particular narrative that was imposed upon one group of humans by another group of humans. Historical events of this ilk, such that they are the consequence of human actions, are themselves narratives—they occurred because of (1) particular Intentional mental states, attitudes, beliefs, etc. (2) and intentional, planned out/premeditated actions. Thus, the historical event of my present concern is the USPHS Syphilis study at Tuskegee
Undergirding many mental states (beliefs, desires, etc.) is the property of Intentionality. [5] All beliefs are mental states having certain properties: 1) beliefs (because they have Intentionality) have aboutness or directedness. “If I have a belief, it must be a belief that such and such is the case” [6]. Not all mental states have aboutness. I may have an attack of nervousness, for example, that is not about anything in particular. Beliefs, on the other hand, is not of that kind. It is a mental state that is about something. This notion that my beliefs have aboutness (or directedness), i.e., that my beliefs are always traveling towards something is philosophical jargon for inferring that my beliefs have Intentionality. Also, beliefs have 2) intentions. In this regard, I am referring to intentional in the classical, non-philosophical sense of having goals, objectives or purposes. Intentions of this sort cannot exist independent of background mental states. To speak of Intentionality, then, is to speak in a discursive and reflective way on a necessary property of belief. One can’t speak of the ethics of belief without acknowledging the belief’s Intentionality, i.e., “what is it about?” If I say I have a certain belief, the very next question would (or should) be “what is your belief about?”
The Study didn’t just happen, like say, an accident of history, void of an Intentional human narrative. The Study was a non-natural act, the result of intentional mental state, attitudes, and belief. Such states need a (mind-to-world) direction of fit. This direction of fit disqualifies interpretations that are inconsistent with an agent’s belief. On this account, there are two kinds of beliefs worthy of mention: de dicto and de re. A de dicto belief is essentially a “belief,” i.e., it is a mental state with content and Intentionality. I am not going into the richness of this discussion, which would take me too far afield of my present concern, except to say, very roughly, that a de dicto belief is an a priori belief, the kind of belief that can be had (arguably) by a brain in a vat, independent of experience. Thus, there is a redundancy in uttering a term like “de dicto belief” [6].
On the other hand, a de re belief is far more fundamental to my present concern. A de re belief is a belief that denotes something existential—or external. One can say that a de dicto and a de re belief have the same starting point. They have the same initial properties for sure. However, de re beliefs interacts with the actual, real world. Commonly, these distinctions are of no significant consequence beyond the philosophy of mind and the philosophy of language but given my showing of how contextual beliefs can function to marginalize fellow humans, this distinction helps in clarifying the ethics of belief. Thus, we will start with a clarification of belief, namely, what it means to have an ethical belief and how an unethical belief can yield ambiguous concern and render harm to others and self. Concerning the Study, unethical beliefs began as de dicto mental states and ended with the (de re) marginalization of 623 black men in Macon County, Alabama, then extended to their families.
The Ethics of Belief
Historical events, caused by intentional actions, happened because human minds made them happen. Beliefs about the historical narrative, if they are untrue, don’t count for anything ethical. If the trajectory of their beliefs is to do good, then the truth value of their beneficent proposition is ethical. If, on the other hand, the trajectory of their belief is to harm, then their actions are maleficent and unethical. I. L. Humberstone surmises, “Beliefs aim at being true, and their being true is their fitting the world; falsity is a decisive failing in a belief, and false beliefs should be discarded; beliefs should be changed to fit with the world, not vice versa” [7]. Facts about the world (e.g., the grass is green, snow is white, Nigeria is in Africa, and water is wet) should always be prioritized over individual opinions about the world, both epistemically and ethically. If the beliefs we have aren’t fortified by facts (i.e., don’t correspond to facts about the world) and good evidence (or valid arguments in defense of facts and evidence) we should set them aside. First person authority of one’s beliefs—i.e., the fact that I have access to my beliefs in a way that no one else is able—tends to render a superiority (or perhaps even an arrogance) that is not necessarily justifiable [8]. It is a special positioning, with special access, but it is not sacrosanct or devoid of error. A person, for good or for ill, may feel fully justified in believing her beliefs—and that makes perfect sense (unless one knows oneself to be delusional)—but if that belief is taken to be perfect, free from error, hubris may prevail. Donald Davidson reminds us that “Error is possible” [8]. Error, mistakes and miscalculations are always possible, “Though there is first person authority with respect to beliefs and other propositional attitudes, an error is possible; this follows from the fact that the attitudes are dispositions that manifest themselves in various ways, and over a span of time” [8]. Thus, beliefs (both de dicto and de re) are vulnerable to error and doubt, “For first-person attributions are not based on better evidence but often on no evidence at all” [8]. Fashioning one’s actions based on uncritical beliefs, therefore, is hubris. It is the beginning of personal folly, bigotry, and unethical behavior. It seems rather difficult for the protagonists in the Study to discount the word-evidence of the credible, namely, one of the primary participants in the Study and the one who brought the lawsuit, Charlie Pollard when he said, “And when this first started up, I didn’t know nothing—just a country boy, as they say. And when they got down here in Alabama, they found what they wanted—they just went to doctoring on us. And said they gon treat us. They just said, ‘bad blood’” [2]. It is clear that Pollard’s words, once juxtaposed with the goal and title of the Study, “the Effects of Syphilis in the Untreated Negro male” (italics mine), successfully refute Dr. Cutler and the other protagonists’ intentions. So long as their de dicto beliefs were only beliefs, there were no objective ethical issues. The moment their beliefs became de re (actual), i.e., the United States Public Health Service came to Macon County, Alabama and objectively fulfilling their beliefs, they were officially involved in unethical behavior. It’s time now to distinguish the two types of beliefs more clearly.
A de dicto belief is not necessarily of moral consequence. Indeed, I cannot be held morally responsible (or reprehensible) for thinking an act that I don’t commit. My subjective beliefs are of no moral consequence unless they are de re beliefs—i.e., my beliefs are of no consequence unless they are beliefs that are imposed upon real external objects. The external objects of our present concern are 623 black men and their families. If it was the case that Cutler and other protagonists of the Study opined privately—like a brain in a vat—nothing ethically hung on their beliefs (or the content thereof). But the moment their beliefs were imposed upon the men (and ostensibly, their spouses and children), causing unjustifiable harm, their beliefs in correspondence with their actions became unethical [9]. Beliefs remaining in one’s head may be metaethical moorings—analogical attempts at resolving puzzles, for instance. On a regular basis, philosophers ponder counter-intuitions, counterfactuals or expedient analogies, everything from pedophilia to murder to genocide are considered. None of these ponderings (or moorings) are considered unethical as such. They are just thoughts, even though some of these thoughts may rise to the level of beliefs. But if their beliefs move from private to public, impacting real human (or non-human) animals in the real world, their beliefs, and their corresponding actions are susceptible to (normative) moral judgement. Let’s say, for example, that a certain man (Paul) dislikes his father-in-law (Sam), which is not abnormal. Paul so dislikes Sam that he regularly ponders murdering him. He envisages a myriad of scenarios about how to kill Sam, and he even practices shooting at an effigy of Sam pinned to a tree stump in the woods. However, because Paul’s ponderings are de dicto—words and thoughts only—he committed no ethical wrong. [10] If he murders his father-in-law through premeditation, he has committed a moral and a legal de re wrong. But is there a possibility of ambiguity here? Perhaps. Imagine that Paul is so angry that with Sam that he goes to the woods and continues his vitriolic target practice with Sam’s effigy attached to a tree stump. As Paul aims at the effigy, unbeknownst to him Sam is taking a walk in the woods and crosses Paul’s line of fire precisely as Paul pulls the trigger. Sam is killed immediately. This is a homicide, but is it murder? Certainly, there is a great likelihood that Paul may be convicted, especially after the jury hears how much he despised Sam, wanted him dead, and often premeditated his murder even to the point of practicing it.
The truth of the matter is that this is a case of accidental death because there is no causal relationship between Paul’s de dicto beliefs and Sam’s death. The de re direction of fit is absent in Paul’s mind. In short, de re beliefs are subject to ethical judgement due to their interaction with the real world in ways that de dicto beliefs do not. Cutler’s (et al.) beliefs moved from de dicto to de re, and, as such, their uncritical analysis of their actions make them susceptible to the prevailing evidence against the Study and made them susceptible to moral judgement. Paul can legitimately plead ignorance of his father-in-law’s presence when the homicide/death took place. Cutler, however, fully believes that his beliefs were justified, and his actions were of no negative consequence. But he is wrong—again. He was wrong with his participation in the Study and he is wrong in the way he frames and delivers his reflections. The evidence is against him. Let me say why.
W. K. Clifford poignantly claimed in the 19th century,
He had no right to believe on such evidence as was before him. He had acquired his beliefs not by honestly earning it in patient investigation, but by stifling his doubts. And although in the end he may have felt so sure about it that he could not think otherwise, yet inasmuch as he had knowingly and willingly worked himself in that frame of mind, he must be held responsible for it [11].
The most compelling function of the ethics of belief is an epistemic one: one is never justified in making assertions in the absence of evidence. Evidence is sacrosanct. Also, justification for believing is intimately connected to evidence. Certainly “whether or to what degree a person is justified in believing something may vary with time” [12]. The protagonists, when faced with mounting evidence, over 40 years, chose to believe corrupted beliefs and false truths rather than good evidence. Once again Clifford makes excellent ethical sense, “However convinced you were of the justice of your cause and the truth of your convictions, you ought not to have made a public attack upon any man’s character until you had examined the evidence on both sides with the utmost patience and care” [12]. There was never intent to treat these men. When penicillin was discovered as a treatment for syphilis they were never administered this potentially curative antidote. And as an aside, in 1932, the same year the Study began, notorious gangster Al Capone was incarcerated in the Atlanta U.S. Penitentiary with syphilis and gonorrhea. When penicillin was found to be curative for syphilis, the ruthless, alleged murderous gangster and convicted income tax evader, was offered the medication though he refused it thinking it was poisonous [13]. Then hard-working black men in Macon County, some of whom were share-croppers, were given less consideration than an acrimonious gangster. Speaking with respect to his honest feelings about the Study, Pollard quietly said, “It did make me, you know, I might have said some curse words-when I was by myself-but they ought to have been ashamed of themselves. I wouldn’t have done them like that” [1, 46:00]. Experimenting on humans without letting them know, and without their consent, is unethical. The men thought they were patients. The protagonists knew they were objectifying these human subjects. If the Study had any integrity they would have been told them the truth; they would have asked for their consent. Whether we like it or not, beliefs, if they are to be regarded as ethical, have social constraints. Clifford offers the following refrain, “And no one man’s belief is, in any case, a private matter which concerns him alone. Our lives are guided by that general conception of the course of things which were created by society for social purposes” [11]. Social justice should never be a privilege—it is an ethical responsibility that begins with doing the good.
The Ethics of Ambiguity
Beliefs are said to be ambiguous or false if they are derived from an interpretation of a historical event in which the mind-to-world direction of fit is somehow fuzzy or unclear. Ambiguity takes place in the mind. It is a confusion of beliefs—justifiably or without justification—based upon evidence and the interpretation of evidence derived from a historical event. As a result, the ethics of ambiguity boils down to what a person believes to be ethical truths based upon his or her interpretation (assuming there are no guiding moral absolutes). If there are no moral absolutes or if there is no objective moral truth, any person seems entirely justified in his or her beliefs, even if said beliefs lead to moral relativism, moral skepticism, or even more extremely, moral nihilism—and ethical ambiguity has room to thrive. Facing this quirk in the complexity of moral philosophy, Fyodor Dostoyevsky’s (The Brothers Karamazov) way of inveighing against such views is to couch his own beliefs as a religious ethic, “Without God everything is permitted.” This relativistic view, which is also found in the Hebrew Bible, “In those days there was no king in Israel; every man did what was right in his own eyes” (Judges 17:6), was refuted by Plato in the Euthyphro over two millennia ago. On Plato’s account, the rightness or wrongness of an action is not contingent upon a Divine Commander who makes an action right because it is “loved by the Gods.” An action tends to be right or wrong for other (more human) reasons (e.g., reason, consequences, sentiments, virtues or caring relations). Nevertheless, there is something that the relativists and the Universalists have in common: they are both necessarily conjoined by the fact that there is no way to construct an argument independent of beliefs. Belief (or having a belief) is a necessary (but not sufficient) condition for having knowledge. If I say I know any particular thing I must also believe it. It makes no sense to say “I know that my mother’s name is Alice, but I don’t believe it.” With respect to moral epistemology (i.e., moral knowledge), the same rule applies. I can’t say, for example, “I know that murder is wrong, but I don’t believe it is wrong.” The challenge question in making such a moral inference, particularly with respect to analytic philosophy, is do I have a supporting argument in defense of my belief and my moral knowledge? [14] So, a legitimate question for John Cutler and others of his ilk could be, “How did you understand the nature of your beliefs and the nature of your ethics during and after the Study? Also, in the face of moral outrage, lawsuits, personal objections and a demand for social justice, why did you hold fast to your beliefs?”
Something is said to be ambiguous if its’ significance is such that more than one interpretation can be offered. Immediately it is clear that ambiguity has something to do with mind and language—mind in the sense that it is here that interpretations are done, and language in the sense that this is the medium through which interpretations are played out both in the mind and in conveyance to others. These terminologies are governed through both cognitive meanings and emotive meanings. From a logical point of view, and in order to get to the particular ends of which I see in this essay, I am more concerned with the cognitive meaning than the emotive one. Cognitive meanings demand evidence to determine the truth-value of particular statements/propositions, but emotive meanings tend to allow emotions and feelings that are vulnerable to biases in a way that facts aren’t. An act or an event is never ambiguous—They are facts. They occurred. The motivations that brought about a particular event may need unpacking, but the act or the event can be independently verified. Acts or events take place in the presence of certain irreversible contingent properties; therefore, “with regard to the past, no further action is possible” [15]. Interpretations of the actions or events are certainly all we have—interpretations. Interpretations such can be correct or incorrect, wrong or right—They can be ambiguous based upon several human factors. But the action itself, or the event, is a fact. It occurred. It represents a historical reality—it is not ambiguous—our interpretations are.
Thus, since an action or event lacks the property of ambiguity, and are, as such, factual or evidentiary, the true focus of our investigation lies in the nature of interpretation—for it is here that the ethics of ambiguity truly finds itself. The nature of interpretation must begin, in logical form, with the truth value of propositions. Such that a proposition is true, it has sustainability in valid and sound logical arguments. There is no ambiguity here. Susan Haack pointedly articulates what propositions can and can’t be if they are to have unequivocal truth-value as premises in a valid argument: “For it is valid if it couldn’t have, not just doesn’t have, true premises and false conclusions” [12]. So the proposition, “The men in the Syphilis study were inhumanely violated,” is true if and only if this proposition can be shown to be true. It is false otherwise—so says the Law of Non-Contradiction. And if this conclusion is true, and if the major and minor premises are constructed with truthful propositions, then the logical dictum—there is no conclusion that is false if all of the premises are true—remains. Every argument such is valid and sound, having true premises (none of which are false) and a true conclusion. This is quite straightforward and an irrefutable philosophical yardstick, especially in analytic philosophy, from Aristotle to today. The strength of any successful refutation would have to show a compromise (or weakness) in any of the propositions (either in the premises or the conclusion) such that either one is less formidable making the premises indeterminable, the argument (potentially) unsound, and is thus ambiguous.
Propositions, then, must be of such disambiguation that they are inaccessible to falsification or pliability. To this end, Scott Soames says the following about propositions, “The key constraint shaping the account is that real propositions are not things we, or other cognitive agents, interpret; they are not instruments we or they use to carry information; they are not entities we or they endow with Intentionality. Rather, propositions are inherently representational entities that are capable of being true or false, independent of any actual use to which we or other agents put them” [16]. The key to Soames benchmark definition is “real propositions”—i.e., as opposed to, say, unreal, artificial, fake, or illusory propositions. The latter has cognitive meaning buttressed by unequivocal evidence, the latter is suspect—suspicious even—a fantasy of sort that seems to render an historical event ambiguous, if it were able—more open to (subjective) interpretation. But again, with respect to the ethics of ambiguity, de Beauvoir says, “With respect to the past, no further action is possible. There have been war, plague, scandal, and treason, and there is no way of our preventing their having taken place; the executioner became and executioner and the victim underwent his fate as a victim without us; all that we can do is to reveal it, to integrate it in the human heritage…” [16]. The only way, it seems to me, to reveal the facts of human history, especially those facts that rise to heinous acts against others, given human tendency toward tribal revisionism, is to disambiguate the propositions of those promoting dehumanization as a matter of course,
I need to be clear: Cutler did not commence the Study, neither is he its only defender, he is more of a metaphor for its advocates. As historian Susan Reverby avers, there were some, even blacks, who saw “nothing wrong with what was done” [17]. But the preponderance of evidence suggests a malicious complicity. The researcher/playwright David Feldshuh of Miss. Ever’s Boys, the fictionalized account of the Study, usefully argues, “Here’s this reprehensible study that very caring people partook in that made me wonder what guidelines would you follow…If our intention are good, how are we to be certain that we’re not engaged in something that will in the future prove to be morally reprehensible or at least morally questionable” [17]. Ambivalence of this sort often hurries to a kind of consequentialism—a utilitarian defense that would concede moral rightness if a reprehensible (or sacrificial) act is such that it produces a greater good, yay, a greater happiness overall. On this account, there is no moral uncertainty; there is no ethical ambiguity. An action is right—not intrinsically, but consequentially—if it tends to promote a better state of affairs overall. Cutler, then, is not at all ambivalent about the Syphilis Study. He quite clearly states, “We were dealing with a very important study that was going to have the long term results of which was to actually improve the quality of care for the black community—so that these individuals were actually contributing to the work towards the improvement of health toward the black community, rather than simply serving as merely guinea pigs for the Study. And, of course, I was bitterly opposed to cutting off the Study for obvious reasons” (italics mine) [2].
The amount of rational, learned professionals, mostly employed by the Centers for Disease Control (CDC) or other parts of the USPHS, who were deeply lacking in human empathy, is so astounding that one may ask why choose Cutler as the metaphor for the Study? His words, as I’ve already shown, in the wake of an escalating moral epistemology decrying the Study, seems heartless—“It was important that they were supposedly untreated, and it would be undesirable to go ahead and use large amounts of penicillin to treat the disease, because you’d interfere with the study.” His willingness to make these claims on camera for the Nova documentary Deadly Deception is instructive, and his responses to the views of others in the USPHS is confirming. Sidney Olansky, Chief of the Division of Venereal Disease Research Laboratory, wrote to Cutler, “Dear John…We agree wholeheartedly with your premises for the validity of the study, your arguments for the importance of this follow-up, and your recommendations for the clinical examination” [17].
Cutler’s argument that it would be “undesirable” to use “large amounts of penicillin to treat the disease” is in itself a violation of the Hippocratic Oath as a physician he vowed to uphold, particularly the stanza, “I will abstain from all intentional wrong-doing and harm, especially from abusing the bodies of man or woman, bond or free.” Do no harm is the common phrasing. But in the minds of Cutler et al, were they committing harm? Not according to their interpretation of their actions or the event. On their account, “the validity of the study” (i.e., the argument that the Study should be prioritized over all other interpretations) or the economy of the Study was sacrosanct—it was an investment in something noble, regardless of other interpretations. Olansky continues in 1951, one-year shy of two decades into the Study, “We have an investment of almost 20 years of Division interest, funds and personnel; a responsibility to the survivors both their care and really to prove their willingness to serve, even at the risk of shortening life, as experimental subjects. And finally, a responsibility to add what further we can to the natural history of Syphilis” [17].
The protagonists of the Study were very clear: the Study was a noble act; there was no ambiguity with respect to their interpretation, even when it meant the direct infliction of pain for no curative end, which is entirely in view with Olansky’s words to Cutler, “Careful studies of spinal fluid and neuromuscular system are advised.” The trauma associated with this kind of invasive medical procedure was not only extremely painful, but it was also dangerous during its early 20th Century usage, which was only a few decades in use before the Study’s conception. Charlie Pollard’s testimony clearly and heroically states, even during the associated agony of the spinal tap, “It was pretty bad—that spinal tap—course, I did along pretty well with it, but uh…I stayed in the bed a week or two” [1]. These men were told that the spinal tap was a “special free treatment.” It is clear that the men saw themselves as patients receiving special care from the United States Public Health Service and the scientist who conducted Syphilis Study at Tuskegee saw the men as “experimental subjects” (and falsely) with a “willingness to serve.” Any willingness they may have had was based upon deception.
The key words in Olansky’s letter to Cutler, which served to affirm and congratulate him, were all given in the best interest, not for the men, but of the Study. Terms like “investment,” “Division interest, funds and personnel,” as well as the paternalistic ambiance of their tone, “their willingness to serve,” “at the risk of shortening [their] life,” and “experimental subjects” are omniscient language in which they offered no unadulterated evidence. Their “willingness to serve” begs the question; did they know they were serving some grand humanitarian end? And if they did know, did they know they were “experimental subjects” and that their lives (and their families’ lives) were at risk? The omniscient, omnipresent and omnipotent languages of these doctors bespeak their God-complex in the lives of an extremely vulnerable population of Negro men in Macon County, Alabama. One year after Olansky’s letter, Eleanor N. Walker, writing to Cutler, continues to encourage him to keep the course: “It seems to me that after 20 years we have too much at stake in this study to let it slide now for the sake of a few dollars.” And, as for those “lost” men who were able to slip through the idiomatic cracks, “In the case of those residing in Alabama it should be simple enough to have them located and examined.” Once again it is clear: the administrators of the Syphilis Study wanted nothing to do with its ceasing, even after two decades of watching misery and death. Their empathy for this population of black had either eroded or never existed. And their urgency didn’t recede—it abounded as we see in Walker’s search for options to ensure the Study’s continuance, “Would it be possible to think about tying in more closely with the [Tuskegee] Institute staff in some way. Certainly, something should be done right now to put the study on a firmer foundation if it is determined it should be continued.” Apparently, the firmer foundation was solidified since the Study continued for another two decades.
The Ethics of the Study
With the help of Simone de Bouveur et al., I have tried to show how that the Syphilis Study wasn’t at all ambiguous—it was a straightforward historical event. Any potential ambiguity would have to hang on a misinterpretation of the Study—a misinterpretation that I take to be wholly unjustified given the level of deception and harm. If the doctors in the Study desired moral salvation, it would have had to be because they thought they weren’t doing something morally prohibited. In their minds, their interpretation of the Study was the correct one. There was no moral or ethical ambiguity in their imagination. I believe that Cutler’s beliefs were morally groundless and unjustifiable, but what of his/their actions? Cutler says, “The fact was it was a concern for the black community.” The morality of the Study rests on the truth-value of this proposition. I think I’ve shown this proposition to be false. And I’ve also showed how Clifford’s scourge against false beliefs, especially when used as propositions in the construction of an argument, is also embraced by Bertrand Russell, “It is undesirable to believe a proposition when there is no ground whatever for supposing it true.”
The USPHS Syphilis Study at Tuskegee was an experiment with (objectified) human subjects, but for these black men in rural Alabama it was an unconscionable disrespect of their freedom and bodies by none other than their government—the United States of America, the “land of the free.” Their basic human liberty was denied and for four decades empathy was an irrelevance. This “study” was anti-black racism. There can be no gainsaying the fact that the USPHS Study on Untreated Syphilis in the Negro Male at Tuskegee was an intentionally racist study; it wasn’t simply a human rights violation. It was an antiblack racist act. None of the men in the Study were white. It was titled as a study on Negro males. An argument could be made that the Study would not have been done with black slave men, because during slavery commodified black bodies had value. But free black men of the Deep South were disposable (this is clear from the post-slavery lynchings), thus the nomenclature of “anti-black racism” of which I give Lewis Gordon’s reflection a generous quote.
In this explicit foregrounding of the self, Gordon’s focus is on the ontology (not the psychology) of everyday black and white egos, the interactive dynamics between these ontologies, and their relations to the origins and maintenance of antiblack racism. The interactive dynamics between these ontologies have trapped black and white ego formation in classic imperial battles for ontological space. By ontological space, I mean space to be, to posit oneself and realize that self-positing. The imperial nature of this battle derives from the fact that Europeans and Euro-Americans have defined the ontological space of white ego genesis in a way that requires the evading of the humanity of Africans. This evasion is effected through the racial redefining of Africans as blacks, Negroes, or more pejoratively as “niggers.” The result is an imperial ontology that restricts the space of black ego genesis and appropriates its ego-formative resources in the interest of white self-formation. (italics mine) [18].
Black men in 1932 Alabama lacked the power and the resources to defend themselves against the imperial threat of a United States government sanctioned, white supremacist ideology. They had nothing with which they could resist the invasion of whiteness—they knew that many of their family members were sick with “bad blood” so they trusted their bodies (and their ontology) to those whose interest was self-centered. The men deserved an ethic of empathy and care. Instead, they were the recipient of ethical egoism—the USPHS did what was right in their own rational self-interest, regardless of the collateral damage in the form of devalued black bodies (and later, Guatemalan brown bodies).
The underlying conceptual scheme facilitating the Study was a white supremacist, anti-black racism that envisioned black lives and black bodies as non-free property, void of any significance or import that whites were duty-bound to respect. Truly antiblack racism envisaged black bodies as non-free regardless of time or space. Consider for a moment the case of Dred Scott, the black slave who accompanied his master, Army officer Dr. John Emerson, to various northern Free states, where it was decided in 1852 by Chief Justice Roger Taney that
…a negro, whose ancestors were imported into the [United States of America], and sold as slaves…had for more than a century before been regarded as beings of an inferior order, and altogether unfit to associate with the white race, either in social or political relations; and so far inferior, that they had no rights which the white man was bound to respect; and that the negro might justly and lawfully be reduced to slavery for his benefit. He was bought and sold, and treated as an ordinary article of merchandise and traffic, whenever a profit could be made by it. This opinion was at that time fixed and universal in the civilized portion of the white race. It was regarded as an axiom in morals as well as in politics, which no one thought of disputing, or supposed to be open to dispute; and men in every grade and position in society daily and habitually acted upon it in their private pursuits, as well as in matters of public concern, without doubting for a moment the correctness of this opinion [19].
The Dred Scott decision, among other things, set the stage for the white supremacist arrogance that would eventually enable hideous actions like the Syphilis Study. Chief Justice Taney’s conceptual scheme was not based upon a parochial decision—it was the overarching decision with only two members of the Court dissenting. The Civil War may have put an end to physical (body) enslavement, but the white supremacist conceptual scheme promoting black inferiority through a pervasive anti-black racism was institutionalized in many white minds through their beliefs, creating the kind of patriarchal white supremacist culture that would make the Syphilis Study a possibility among enlightened, rational people who lived in the United States. The correlation of Scott and the men of the Study accentuates the absence of two values in the overarching conceptual scheme: freedom and empathy.
Conclusion
In conclusion, de Beauvoir, writing on what it means to be free, says, “But if man is free to define for himself the conditions of a life which is valid in his own eyes, can he not choose whatever he likes and act however he likes?” [15]. I am not binding myself to the French existentialism Beauvoir is defending here, but as a definition of freedom, I find much purchase. In other words, 1932 Macon County, Alabama had an unusually high rate of syphilis, roughly one-third of the men tested had the sexually transmitted disease. This “fact” caught the attention of the USPHS, whereupon they commenced a study—and experiment—of what would happen if these black men were untreated. To our present knowledge, the USPHS didn’t give the men the syphilis virus, neither through injection nor any other form (though we can’t discount this possibility that they may have, given the nefarious action was done a few years later in Guatemala by some of the same scientists, including Dr. Cutler), but what they did was of such deceitfulness that it interrupted history. The force of history is such that, in the words of theologian David Tracy, [20] “it is not only contingent; history is interruptive” [19]. The historical interruption seems clear enough:
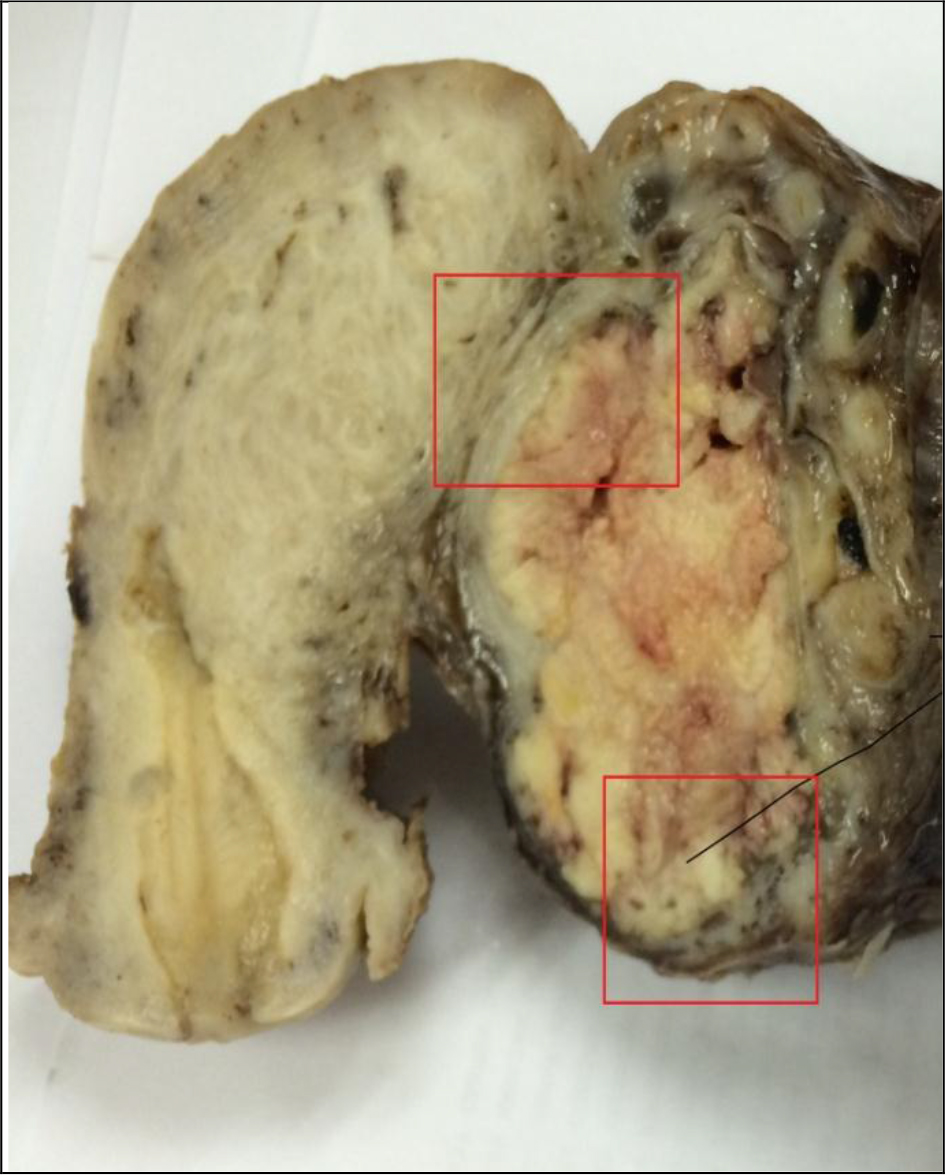
The men thought that they were patients of a joint federal and local medical and nursing program at the Tuskegee Institute and the Macon County health department for their “bad blood,” a local idiom that encompassed syphilis as well as anemias. They did not consider themselves subjects since they did not know the study existed. The PHS followed the men for forty years (from 1932 to 1972), actively keeping them from many forms of treatment (including penicillin when it became available in the 1940s), never giving them a clear diagnosis, but providing them with the watchful eyes of a nurse as well as exams (including a diagnostic spinal tap), placebos, tonics, aspirins and free lunches. Burial insurance became an additional inducement for their participation. In exchange, the men or their families agreed to allow for autopsies without knowing that the researchers needed to confirm the ravages of syphilis on the men’s organs and tissues. [17].
Among the many pieces of evidence of what seems somewhat sadistic, or apathetic is the organizational structure derived from the conceptual scheme. There is no happenstance in this socio-scientific-medical construction. Instead, we see the properties of what injustice demands: an abuse of power by those who were in structurally powerful positions to halt the freedom of the powerless. The ethical violations, the human rights violations and the racism that hovered over this successful effort to constrain the vulnerable is clarified further by Tracy’s critique, “To be an American is to live with pride by participating in a noble experiment of freedom and plurality. But to be a white American is also to belong to a history that encompasses the near destruction of one people (the North American Indian, the true native Americans) and the enslavement of another people (the blacks)” [19].
In contrast to Dred Scott, a slave, the syphilitic (as well as the controlled group) men of Macon County were not slaves, but they were deceived just the same. They thought the actions of the doctors were noble. Herman Shaw, one of the men in the Study, said, “The way I heard about it was through a rumor that the people, and this came out of Macon County, said that you can get free medicine for yourself, and things of that kind. And therefore, I went. On that Saturday afternoon when we went over there, they said we would get free medicine, that wouldn’t cost us anything and the doctor… We will get free doctoring” [2]. They went to become patients of medical doctors. They were made interruptions of history as objectified experimental subjects. There is no way that deception of this kind can be morally prudential.
References
- A non-digitalized version of this article was previously printed without open access as a commentary in Journal of Healthcare, Science and Humanities. Vol. VIII, Number 1, Spring 2018.
- Deadly Deception: https://www.youtube.com/watch?v=qNa8CnC4sSU Deadly Deception 3:31
- Guatemala Syphilis Experiment https://www.britannica.com/event/Guatemala-syphilis-experiment; Recent questions regarding the existence of the specimens gives good reason to doubt the Study’s 1972 termination. See,
- Roy, Benjamin (1987) The Tuskegee Syphilis Experiment: Biotechnology and the Administrative State. Journal of the National Medical Association 87: 1;
- Spector-Bagdady, Kayte and Paul A. Lombrardo (2018) From in vivo to in vitro: How the Guatemala STD Experiments Transformed Bodies into Biopecimens” The Milbank Quarterly 00:1–28.
- Such as hurricanes. In 2017 Hurricane Irma and Maria devastated the Caribbean, but there were no underlying mental states. Though we tend to use generic language like “acts of God” to contextualize a certain kind of phenomenon, hurricanes and other kinds of environmental events are natural historical events having no import for my present concerns.
- The “I” is capitalized to differentiate between “Intentionality” as a function of mind in which mental states are very often about something and “intentions” or to “intend.”
- Searle, John. R. (1983). Intentionality: An Essay in the Philosophy of Mind. Cambridge, New York, Oakleigh, Melbourne: Cambridge University Press.
- Humberstone L (1992) Mind, New Series. Cambridge University Press 101: 59–83..
- Davidson, Donald (2001). New York: Oxford Press.
- Slote, Michael (2001) Morals from Motives. New York: Oxford University Press, Inc.
- There are some ethical theories, like Christian ethics, for example, “For as he thinks in his heart, so is he” (Proverbs 23:7) and other words spoken by Jesus on his Sermon on the Mount, that take motives and other de dicto beliefs to be on the same level of committing the action. But this doesn’t work rationally. It is hard to envision an argument that would put thinking about pedophilia as being equivalent to actual pedophilia. Doing an act requires far more commitment than thinking an act. Either way, Christian ethics would also decry the Study even to a greater extent than other non-cognitivist and cognitivist approaches.
- Clifford, William Kingdon (2008) The Ethics of Belief, A. J. Burger.
- Haack, Susan (1995). Evidence and Inquiry Malden: 1995.
- Al Capone dies in Florida villa”. Chicago Sunday Tribune. Associated Press. January 26, 1947.
- As well as, to what degree am I justified in believing my beliefs? It does make good sense to believe my beliefs—even if they are ambiguous, but I am justified to a lesser degree—because if I don’t believe my beliefs, I would believe nothing at all, unless I find that my beliefs are delusional or fail to correspond to the “experts” or facts about the real world.
- de Beauvoir, Simone. (1948). The Ethics of Ambiguity. New York: Philsophical Library.
- Soames, Scott. (2015). Rethinking Language, Mind, and Meaning. Princeton, Oxford: Princeton University Press.
- Reverby, Susan M (2000) Tuskegee’s Truths: Rethinking the Tuskegee Syphilis Study.Chapel Hill, London: University of North Carolina Press.
- Gordon, Lewis R. (1995). Bad Faith and Antiblack Racism. Amherst: Humanuty Books.
- Scott v. Sanford, 60 U.S. (19 How.) 393 (1857).
- Tracy, David (1987) Plurality and Ambiguity. Chicago: University of Chicago Press.