Abstract
The Pregnancy Ecological Assessment (PregEMA) Pilot Study was designed to apply EMA approaches (i.e., capturing experiences in real time in the natural environment) among a population of pregnant women. A total of 28 women completed EMA surveys on their smartphone over a 4 week period during their second and third trimester. We assessed mood, eating, physical activity, stress, location and context at the beginning of the day, end of day, and randomly throughout the day and week. The majority of participants completed EMA surveys (average 76% completion rate) with limited missing surveys. Key findings from the EMA data were that on average, women indicated having trouble sleep 71% of the time, were taking prenatal vitamins 73% of the time, were physically active 55% of the time, and spent 5.7 hours per day sitting. The innovative approaches employed in PregEMA allowed us to understand women’s experiences in real-time and in women’s natural environments. Future work could consider how these methods may be integrated into larger population studies, trials and clinical or community-based interventions.
Keywords
Pregnancy; Ecological Momentary Assessment (EMA); mobile technology
Background
Ecological momentary assessment (EMA), the repeat assessment of experiences, behaviors, and mood in real time within one’s own environment has been applied in multiple studies, particularly in areas related to health [1]. EMA has been applied in numerous contexts including but not limited to studies related smoking cessation[2, 3], eating patterns[4], and cardiovascular activity[5]. EMA has been useful in addressing limitations in data collection methods that rely on recalling previous experiences over long periods of time as well as capturing dynamic processes that may fluctuate or change over short periods of time. EMA has rarely been applied in studies of pregnant populations; however some prior examples include the use of technologies such as personal digital assistants (PDA) to assess the psychological state of pregnant women to predict the length of human gestation [6, 7] and repeat collection of saliva samples and psychological distress questionnaires administered at short intervals to assess psychological distress and pregnancy outcomes [8].
Previous studies have used mHealth (mobile health) approaches among pregnant populations. However, there are no known published studies to date that specifically use mobile technology or smartphones coupled with EMA data collection to assess the health and experiences of pregnant women in real time. The application of EMA through current technologies such as smartphones can be useful for data collection among pregnant women given the dynamic, complex nature of pregnancy [9].
As a result, we developed the Pregnancy Ecological Momentary Assessment (EMA) Pilot Study (PregEMA), which was designed to examine the central question of whether EMA data collection through smartphone technology could be applied among a pregnant population to understand their contexts, behaviors/lifestyle factors, and psychosocial well-being. As a secondary aim, we explored the possibility of collecting location data in real-time, an extension of EMA known as geographical momentary assessment (GMA), in order to assess context/environments [10]. Assessment of location and environment in real time provides an avenue to capture women’s multiple environmental exposures outside of their residential neighborhood as typically measured in prior studies. Today, the smartphone allows for instant access to participants for real time data collection and transfer of information, and the GPS built into smart phones permits collection of information on subject location. Data from Pew show that smartphone use is common enough to support applications and are feasible among the proposed study population with a high percent of smartphone ownership[11]. These approaches can remotely capture women’s daily experiences and provide insight into effective strategies and interventions for addressing health during pregnancy. This paper presents the methods and design of PregEMA and some descriptive data of the study population.
Methods
Recruitment and Sample
PregEMA is a pilot ancillary study to the GDM2 Trial, a randomized controlled trial designed to assess two screening approaches for diabetes in pregnant women (i.e., gestational diabetes)[12, 13]. Participants recruited for GDM2 are a diverse sample of pregnant woman between the ages of 18–45 with singleton pregnancies between 18–24 weeks of gestation. Exclusion criteria are preexisting type 1 or 2 diabetes, hypertension requiring medication, inability to complete or already completed glucose testing, advanced HIV or liver disease, and recent steroid use. The study takes place at a hospital in Pittsburgh, PA. Women are recruited directly through the hospital clinic, flyers, electronic announcements, social media advertisements, and through other physicians’ offices. Study recruitment for GDM2 began in July 2015. Recruitment for PregEMA began October 2015 and ended in Jan 2016. Women from GDM2 were approached during their first or second study visit (between 24 and 28 weeks gestation) to gauge their interest in participating in PregEMA. After their GDM2 visit, in which they were either completing their initial glucose tolerance test (visit 1) or randomized to take the follow-up glucose tolerance test (visit 2), women were asked if they were interested in hearing about PregEMA; and if so, the research coordinator would describe the study, review the eligibility criteria, and review informed consent. Women also received the study coordinator’s contact information if any technical issues or other problems were to arise. Eligibility criteria for PregEMA included having a smartphone and willingness to use their own smartphone for completing EMA surveys. We approached 37 women from GDM2, and 3 did not have a smart phone and 2 were not interested. A total of 32 women completed consent forms while 31 initiated the web-based application. Our final analytic sample included 28 women who completed at least 16 surveys over the 4-week study period. The Institutional Review Board for the University of Pittsburgh approved this research study.
Study Design and EMA Data Collection
PregEMA is a prospective study where women were followed over a 4-week period. Over the 4-week period, women received prompts through the smart phone via text, linking them to time-specific surveys through an online system. Participants would receive prompts to complete surveys at the beginning of the day (BOD), the end of day (EOD), and at a random day and time. Participants received prompts to complete the BOD and EOD surveys 3 times a week (various days) as well as a random prompt twice per week. Participants set the times for which they would like to receive their BOD and EOD, with the times being at least twelve hours apart. Participants are given 30 minutes to complete the BOD and EOD surveys with reminder text messages sent every 10 minutes. They were given 60 minutes for the random survey with reminder text messages sent every 20 minutes. After that time period, the survey would cancel and would be considered missing. Figure 1 includes example screen shot of the EMA prompts as they appear on the smartphone.
After the initial protocol was set up on the participant’s phone through the online system, their information was stored in their browser’s cookies. The cookies were then sent to a secondary server, which was separate from the primary server used for the back-end program designed to send the survey prompts. Information was communicated back to this secondary server, which included a program designed to check when surveys were available. Once the participant completed and submitted their survey, that information was also sent back to the secondary server, where the data was loaded into a database. Each time the participant completed a survey, their GPS coordinates (longitude and latitude) were also recorded. Participants had the option of turning on/off their location services. After the 4-week period, women were invited to complete a 20–30 minute exit interview over the phone for feedback about the protocol and overall study. Women were compensated $35 if they completed 3 surveys per week over the 4-week study period and an exit interview. Women did not receive direct payment for their phone or data charges.
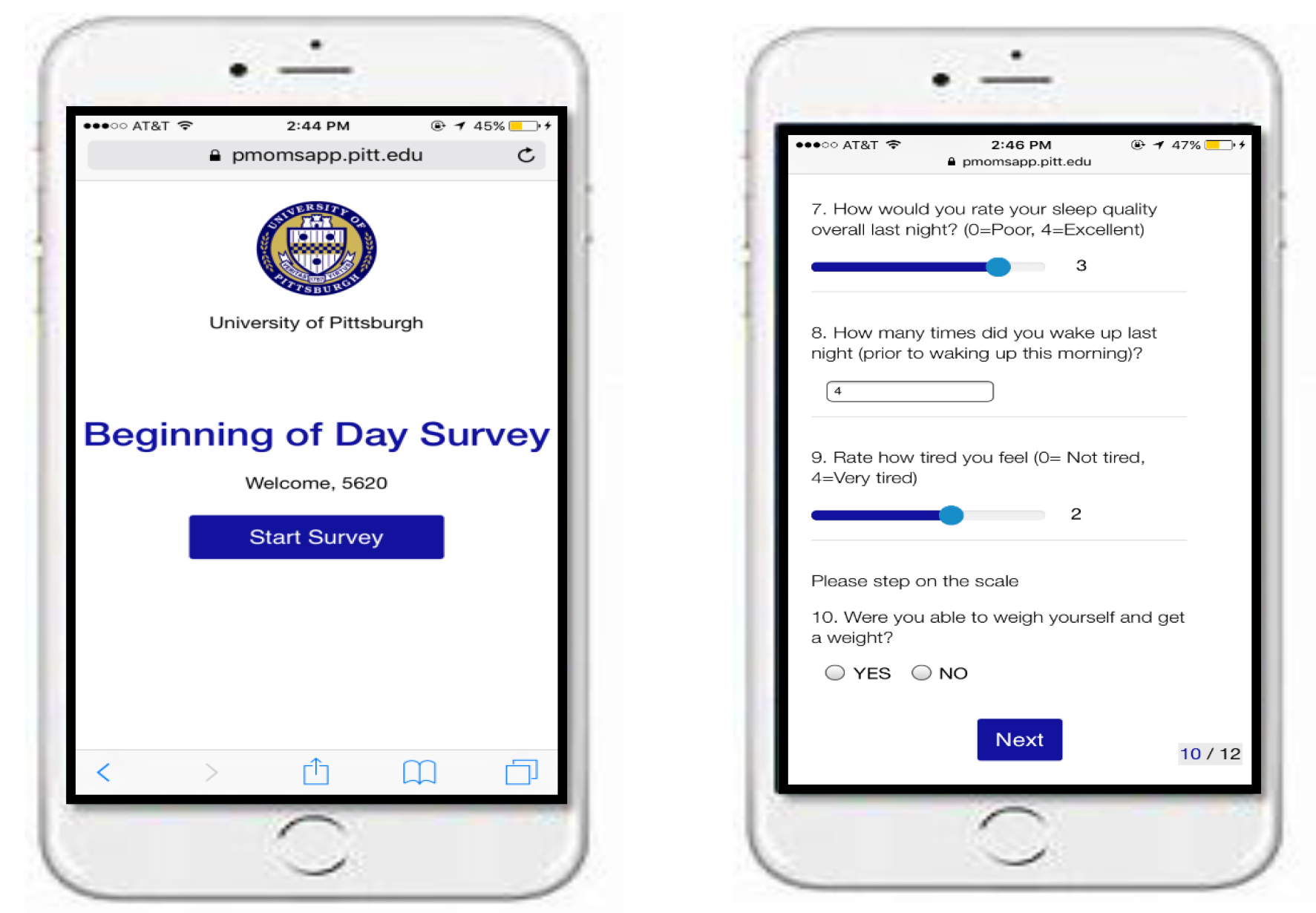
Figure 1. Screenshot of EMA Prompts on Smartphone
Measures
PregEMA included a variety of measures for the BOD, EOD, and random surveys. Many of the measures had parallel items from existing tools and scales. For example, the Cohen Perceived Stress Scale is a validated scale with multiple measures [14]. Although not developed for the EMA context, we adapted measures from this scale and others for this study. Some other measures were derived from other EMA studies [15].
BOD Survey. The BOD survey was designed to assess women’s mood and experiences in the morning and what may have occurred overnight. We collected measures on sleep, eating patterns, and mood. Example questions were “Did you have trouble falling asleep” with a yes or no response; “Rate how well you slept last night” with a response of 0 = poor to 4 = excellent; and “How are you feeling” with various options that they could check all that apply such as Happy, Angry, Stressed and Content.
EOD Survey. The EOD survey was designed to assess women’s experiences during the day and was only collected once per day, not throughout the day. Once again, we asked questions about rest, sleeping patterns, physical activity, and eating patterns. Exampled questions included “Were you able to eat today” with the option of yes or no. There were several follow up questions such as “How many meals and snacks did you eat today?”; “Did you eat anything before 12 noon”; “Did you change what you ate today because of weight gain?” Additionally, we asked that if participants purchased foods for the day, that they take a picture of the receipt. They had an opportunity during the EOD day prompt to upload pictures of receipts of foods they purchased. This could have been food purchased at any convenience or grocery store, including anything eaten a restaurant.
Random Survey. The random survey questions were sent at a random time during the waking hours (between times of the BOD and EOD alarm prompts) and any day of the week. They received a maximum of two random surveys per week. The random survey included items of discrimination, stress, and experiences in healthcare settings [16]. Example questions were “In the past week, have you seen a doctor, nurse or other healthcare worker for this pregnancy?” with follow-up questions such as “How satisfied were you with the care you received” on a scale of 1–5; “In the past week, were you treated unfairly because of your race or ethnic group?” If they answered yes, the follow-up question was “Where?” with options such as at the doctor/healthcare clinic, at a restaurant, at work.
Direct questions about context were sent with each EMA prompt: “Where are you?” (e.g., home, work, outside). “Who are you with?” (e.g., alone, with partner/spouse, other family member, other). GPS (longitude, latitude) capabilities are embedded in the current technology for smartphones allowing us to collect location as participants complete the various EMA prompts.
Analyses
The primary analyses are descriptive and show trends and prevalence of the core survey questions as well as location. Location information (longitude/latitude) were mapped using ArcGIS version 10.5 (ESRI; Redlands, CA). Since participants were completing the same survey questions multiple times over the 4 week period, univariate analyses were conducted by taking an unweighted average within subject and then averaging responses across subjects. Descriptive analyses were completed using SAS version 9.4 (Cary, NC).
Results
Table 1 includes characteristics of the population of women who completed a minimum number of EMA surveys. The characteristics of women in the pilot PregEMA were similar to the overall characteristics of the source population from the GDM2 Study.
A total of 880 surveys were sent to the 28 participants. In total, 665 surveys were attempted/completed (BOD=278 out of 388, EOD=292 out of 372, RAND=95 out of 120) for completion rates of 72%, 78%, and 79%, respectively, and an overall completion rate of 76%. The total number of responses varied from a low of 12 to a high of 28 with a mean of 23 and a median of 25 data collection points.On average participants completed 9.7 BOD and 10.4 EOD surveys over the month period. Subjects had good compliance with random surveys. Only two participants completed 1 or 2 random surveys while the remainder completed 3 or 4. Within each time point, participant’s tended to have answered all the survey questions. An examination of the main questions of each time point (excluding the food receipt upload option) shows high response rates within each BOD, RAND, and EOD time point with the average number of answered questions as follows: BOD 8 + 0.8 (out of 9 questions), RAND 8 + 0.5 (out of 9 questions), and EOD 9 + 0.9 (out of 11 questions). The most commonly missed BOD question was BOD6 which asks subjects to rate their level of hunger. The most commonly missed RAND question was RAND3 which asks subjects about unfair treated today because of her race or ethnic group. In part this was driven by one subject who never answered this question. There was not a pattern of missing questions within the EOD surveys. Table 2 includes each type of survey completed per participant.
Table 1. Characteristics of the Population (N = 28)a
|
Estimate |
|
|
Age, M (Range) |
26 [19–37] |
|
Pre-Pregnancy BMI, M (Range) |
29 [22–41] |
|
Weeks Gestation, M (Range) |
27 [20–34] |
|
Race, % |
|
|
Non-Hispanic Black |
48% |
|
Non-Hispanic White |
43% |
|
Mixed Race |
9% |
|
Income (yearly), % |
|
|
<$20K |
57% |
|
$80K+ |
13% |
|
Education, % |
|
|
HS/GED |
35% |
|
Some college |
22% |
|
College degree |
22% |
a. Height and weight (to calculate BMI) were all taken at participant’s 1st visit, while gestation was collected at the start of the surveys. There were several income and education categories, but only a few are presented. Yearly income was not adjusted for family size.
Table 2. Surveys Completed Per Participant (N = 28)
|
Time Category |
Minimum count per person |
Maximum count per person |
M (SD) |
|
Across all time categories |
12 |
30 |
23 (3.9) |
|
BOD |
4 |
16 |
9 (2.5) |
|
EOD |
5 |
13 |
10 (0.6) |
|
R |
1 |
4 |
3 (0.7) |
Participants in the study had the option to allow location data to be included with their survey responses. The majority of surveys included location data (80.3%). Missing location data were subject dependent rather than time point dependent. Missing location information for the three time periods (BOD, RAND, and EOD) occurred on 20.7%, 20%, and 18.6% of surveys respectively. However, 65.1% of the missing location data occurred in just 4 participants. No information is known about device or cellphone provider so it could not be determined if one of these factors contributed to missing location data. Participants were not restricted to any particular area during study participation, but the subject’s location data was predominantly within Allegheny County with a few locations outside of Allegheny County in PA, OH, and FL. The location data revealed that very low location variability was collected, both overall and between time points (BOD, RAND, and EOD). Three extreme location outliners, 2 in Florida and 1 in Ohio, were removed before examining the data. Minus these locations that were far out of the subject’s normal pattern, the maximum range between survey points within subject was between 0.0171 and 96.7 km with an average (standard deviation) of 24.0 ± 24.7 km. A given subject’s location data is predominantly found within 10 km of other location data from that same subject.
Tables 3–5 include descriptive analyses of the overall population by taking the within person unweighted average and then averaging across all participants for the study time frame (i.e., 4 weeks). In table 3, the beginning of day responses indicate that a majority of participants had trouble falling asleep but on average slept 7 hours each night. The rating of their sleep quality was average although a majority indicated being tired when asked about mood/feelings. In table 4 at the end of the day, on average, women at almost 4 meals or snacks per day, with a majority eating a meal/snack prior to noon. Not many participants indicated changing what they ate due to concerns with weight gain. About half of the participants indicated being physically active on average while 65% of the population spent 5 hours or more sitting in a given day. As indicated in Table 5, which were random prompts, women were around 28 weeks pregnant when they participated in the study. About 41% saw a healthcare provider within the past week; and out of those, a great majority were satisfied with their care. No one in the population indicated being treated unfairly due to their race (racial discrimination). Two core question related to perceived stress were queried and indicated that women have a sense of control over important aspects of their life and the ability to handle important life issues.
Table 3. Beginning of Day Responses
|
Survey Question |
Estimate |
|
Did you have trouble falling asleep last night? (yes) |
71.9% |
|
How many hours of sleep did you get? |
7.0 |
|
Rate how well you slept last night (0=poor, 4=excellent) |
|
|
0 |
7% |
|
1 |
19% |
|
2 |
34% |
|
3 |
31% |
|
4 |
9% |
|
Do you feel nauseous or ill? (yes) |
16% |
|
Please rate your level of hunger (0=not hungry, 4=very hungry) |
|
|
0 |
16% |
|
1 |
30% |
|
2 |
27% |
|
3 |
15% |
|
4 |
12% |
|
Have you had anything to eat or drink this morning? (yes) |
62% |
|
Did you eat overnight or late at night after dinner? (yes) |
31% |
|
How are you feeling? (check any that apply) |
Selected items Tired: 88% Happy: 29% Content: 40% |
Table 4. End of Day Responses
|
Survey Question |
Estimate |
|
Were you able to eat today? (yes) a |
99% |
|
(if yes) How many meals and snacks did you eat today? |
3.8 |
|
(if yes) Did you eat anything before 12 noon? (yes) |
62% |
|
(if yes) Did any pain, fatigue, or other symptoms of pregnancy affect how you ate today? |
16 |
|
(if yes) Did you change what you ate today because of concern about weight gain? b |
7% |
|
Did you take a pre-natal vitamin today? (yes) |
73% |
|
Were you physically active today? (yes) |
55% |
|
How many hours did you spend sitting today? c |
5.7 |
|
Did you sleep or rest during the day today? (yes) |
32% |
|
(if yes) How many hours? |
2.6 |
a. Only two records where a subject reported not eating for the day
b. Only 4 participants changed eating due to concerns about weight gain
c. 65% spent 5 or more hours sitting
Table 5. Random Survey Responses
|
Survey Question |
Estimate |
|
How many weeks pregnant are you? |
28.1 |
|
In the past week, have you seen a doctor, nurse or other healthcare worker for this pregnancy? (yes) |
41% |
|
(If yes) How satisfied were you with the care you received (on a scale of 1–5, with 5 being most satisfied and 1 being least satisfied)? |
|
|
1 |
3% |
|
2 |
11% |
|
3 |
13% |
|
4 |
15% |
|
5 |
58% |
|
(If yes) Please select the topics you discussed (check all that apply) |
Top topics: Weight gain: 73% Gestational diabetes: 37% Medicines: 37% Preterm labor signs: 34% Breastfeeding: 24% |
|
In the past week, how often have you felt like you were unable to control the important things in your life? 0=never; 1=almost never; 2=sometimes; 3=fairly often; 4=very often |
|
|
0 |
41% |
|
1 |
27% |
|
2 |
18% |
|
3 |
12% |
|
4 |
2% |
|
In the past week, how often have you felt confident about your ability to handle your personal problems? 0=never; 1=almost never; 2=sometimes; 3=fairly often; 4=very often |
|
|
0 |
9% |
|
1 |
3% |
|
2 |
20% |
|
3 |
27% |
|
4 |
41% |
Based on some results from the exit interview, we identified several ways in which we could tailor a future protocol and learned of participants’ perceptions of using mobile technology in order to assess pregnancy health and well-being in real time. A few key themes emerged: participants discussed dividing questions about food intake by meals and snacks rather than one question on meals; tailoring questions related to physical activity and amount of sitting each day; eliminating the feature to upload pictures of participants food and restaurant receipts as many participants did not collect paper receipts. We also asked women during the exit interview about the potential burden of receiving EMA prompts at least 4 times per week, and no participant cited this as a major burden or deterrent from participating. The majority of participants also said they would have been willing to completed surveys for longer than four weeks. Further analyses from these exit interviews will be useful in continuing to tailor protocols for EMA data collection among pregnant women.
Discussion
PreEMA is an approach to advancing EMA data collection during pregnancy with the goal of understanding some of the dynamic processes women undergo extending beyond the physiological changes typically assessed in biomedical research. The innovative approaches employed in PregEMA allows us to understand women’s pregnancies in real-time and in women’s natural environments. This is the first study of our knowledge that incorporates real-time measurements of behavioral, psychosocial, and environmental factors and processes during pregnancy and over a 4-week period.
The measures collected in this study allows us to apply multi-level frameworks to complex processes by integrating individual and environmental level data. The psychosocial measures of mood, stress, and discrimination have been collected in previous EMA studies, including assessment of diurnal patterns of salivary alpha amylase in pregnant women via PDA prompts for women to collect their own saliva samples while also completing mood assessments using paper and pencil methods [17]. However, no studies of our knowledge collect EMA data of stress as well as mood and experiences of discrimination via mobile technology and beyond the short 1 week intervals that are typical of EMA studies. Additionally, the collection of women’s location via the GPS capabilities embedded in the smartphone allowed for the implementation of geographical momentary assessment to understand location in tandem with participants’ reports of their environments. These location measurements present an opportunity to uncover patterns of mobility among pregnant women over an extended period of time and implementation of geospatial analyses that can aid in identifying clustering and patterning of health risks and behaviors in space and time.
There are some limitations in EMA data collection that are not characteristic just to this study. Although EMA methods allow for data collection in real time, repeat, intensive measurement can be burdensome over long periods of time. EMA helps to minimize recall bias, particularly among items that are dynamic and change within shorter intervals. However, the items from longer, validated scales have not been necessarily validated for EMA data collection nor designed to capture micro-processes. The technology developed for this pilot study is similar to other applications outside of EMA data collection. However, there is a challenge of developing an application that may not be transferable across operating systems. In order to address this, our pilot included a web-based application that required the participant to be connected to Wi-Fi either directly or through their data plan. This sometimes posed as a challenge for participants who did not always have a data plan or who could not connect to Wi-Fi. A future protocol should include a phone-based and web-based component that allows the participant to complete EMA prompts when they are not connected to Wi-Fi or a data plan but then automatically uploads data whenever connected.
This pilot has also informed future research for a larger EMA cohort as well as continuation of EMA data collection to understand real-time micro-processes during the postpartum period, a time when mothers are going through tremendous changes, including taking on new maternal roles. The results of this pilot will aid in providing new research questions and hypotheses related to the multiple pathways between context and health among childbearing women to develop future interventions, programs and policies. Furthermore, the use of mobile technology to assess women’s health in real-time during pregnancy can directly inform a future intervention designed to address the multiple demands and challenges women face during pregnancy and beyond. Future work using mobile technology should apply person-centered design coupled with supportive services in real time and when necessary (just-in-time interventions) as well as support current modes of clinical and social service care for women and their children.
Acknowledgement
We would like to thank the women who agreed to participate in the pilot study. We would also like to thank the staff and co-investigators of the GDM2 Trial, including Dr. Esa Davis (PI). We would like to thank the PregEMA pilot study staff and students; including the recruitment and retention team, Jessica Duell and Rashaa Brown; and the technology team Er Wang and Dr. Hassan Karimi. We would also like to thank Dr. Lora Burke for her guidance in developing the protocols for the EMA mobile application and using her EMPOWER study as a prototype. Finally, this pilot study was made possible in part from funding from the Academy Health/Aetna Foundation Scholars-in-Residence Fellowship. The PI, Dr. Dara Mendez was funded by a Diversity Supplement NIH/NHLBI R01HL107370-S1 (Mendez/Burke) while she was conducting this pilot study. This pilot study led to the development of the NIH/NHLBI funded Postpartum Mobile Mothers Study (PMOMS).
References
- Shiffman S, Stone AA, Hufford MR (2008) Ecological momentary assessment. Annu Rev Clin Psychol 4: 1–32. [crossref]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, et al. (2002) Immediate antecedents of cigarette smoking: an analysis from ecological momentary assessment. J Abnorm Psychol 111: 531–545. [crossref]
- Hufford MR, Shields AL, Shiffman S, Paty J, Balabanis M (2002) Reactivity to ecological momentary assessment: an example using undergraduate problem drinkers. Psychol Addict Behav 16: 205–211. [crossref]
- Engel SG, Kahler KA, Lystad CM, Crosby RD, Simonich HK, et al. (2009) Eating behavior in obese BED, obese non-BED, and non-obese control participants: a naturalistic study. Behav Res Ther 47: 897–900. [crossref]
- Kamarck TW, Shiffman SM, Smithline L, Goodie JL, Paty JA, et al. (1998) Effects of task strain, social conflict, and emotional activation on ambulatory cardiovascular activity: daily life consequences of recurring stress in a multiethnic adult sample. Health Psychol 17: 17–29. [crossref]
- Spicer J, Werner E, Zhao Y, Choi CW, Lopez-Pintado S, et al. (2013) Ambulatory assessments of psychological and peripheral stress-markers predict birth outcomes in teen pregnancy. J Psychosom Res 75: 305–313. [crossref]
- Entringer, S, Buss C, Andersen J, Chicz-DeMet A, Wadhwa PD (2011) Ecological Momentary Assessment of Maternal Cortisol Profiles Over a Multiple-Day Period Predicts the Length of Human Gestation. Psychosomatic Medicine 73: 469–474. [crossref]
- Giesbrecht GF, Poole JC, Letourneau N, Campbell T, Kaplan BJ, et al. (2013) The Buffering Effect of Social Support on Hypothalamic-Pituitary-Adrenal Axis Function During Pregnancy. Psychosomatic Medicine 75: 856–862. [crossref]
- Newham JJ, Martin CR (2013) Measuring fluctuations in maternal well-being and mood across pregnancy. Journal of Reproductive and Infant Psychology 31: 531–540.
- Epstein DH, Tyburski M, Craig IM, Phillips KA, Jobes ML, et al., (2014) Real-time tracking of neighborhood surroundings and mood in urban drug misusers: application of a new method to study behavior in its geographical context. Drug Alcohol Depend 134: 22–29. [crossref]
- Pew (2013) Internet and American Life Project.
- Abebe KZ, Scifres C, Simhan HN, Day N, Catalano P, et al. (2017) Comparison of Two Screening Strategies for Gestational Diabetes (GDM(2)) Trial: Design and rationale. Contemp Clin Trials 62: 43–49. [crossref]
- Scifres, C.M., et al., (2015) Gestational diabetes diagnostic methods (GD2M) pilot randomized trial. Matern Child Health J 19: 1472–1480. [crossref]
- Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24: 385–396. [crossref]
- Burke LE, Shiffman S, Music E, Styn MA, Kriska A, et al. (2017) Ecological Momentary Assessment in Behavioral Research: Addressing Technological and Human Participant Challenges. J Med Internet Res 19: 77. [crossref]
- Williams DR, Yan Yu, Jackson JS, Anderson NB (1997) Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination. J Health Psychol 2: 335–351. [crossref]
- Giesbrecht GF, Campbell T, Letourneau N, Kooistra L, Kaplan B, et al. (2012) Psychological distress and salivary cortisol covary within persons during pregnancy. Psychoneuroendocrinology 37: 270–279. [crossref]