Abstract
Objective: To assess preinjury frailty in elderly hip fracture patients as a predictor for postsurgical morbidity and mortality, prompting early referral to palliative care services in patients deemed high-risk for postoperative complications. Including palliative care in the multidisciplinary care of the high-risk patient has been shown to improve quality of life (QOL), increase patient and caregiver satisfaction, and reduce healthcare costs.
Design: The design is a quality improvement initiative.
Setting: The setting is an academic medical center, serving as the region’s Level 1 Trauma Center. There is no current process for measuring frailty as a predictor of postsurgical morbidity and mortality.
Participants: The project’s participants are elderly adults aged 65 and older presenting to the emergency room for treatment following a hip fracture.
Interventions/Measurements: A frailty measurement tool using PDSA (plan-do-study-act) cycles was selected. Next, a clinical decision-making algorithm for risk assessment and palliative care referral was designed and implemented for the project participants. Pre- and post-implementation referral rates and post-implementation risk identification and compliance with the utilization of the risk assessment tool were measured. This initiative aimed to begin preoperative frailty assessment with 50% compliance in the target population, with palliative care referral occurring per recommendations based on an algorithm.
Results: Patients in the post-implementation group were more likely to have their frailty risk evaluated and to receive a palliative care referral than the pre-implementation group. Rates of risk identification and palliative care referral increased by 68% and 85%, respectively, which surpassed the goals of this initiative.
Conclusion: Identifying patients with higher preinjury frailty can predict those at risk for mortality and morbidity, thus indicating those patients for whom palliative care referral may be beneficial. Using a standardized process for preinjury frailty screening and referral increased risk assessment and palliative care referral for elderly hip fracture patients.
Keywords
Hip fracture, Frailty, Frailty screening, Elderly, Palliative care
Introduction
In the United States, there are an estimated two million bone fractures annually [1]. These fractures account for over 432,000 hospital admissions and around 180,000 nursing home admissions [1]. Hip fractures account for 14% of these bone fractures [2], accounting for over 300,000 hospital admissions annually in the United States [3]. Hip fractures represent 72% of fracture-related medical expenses [2], with the estimated cost of hip fracture in the United States being $12-15 billion annually [4]. A low-impact trauma, such as a fall from standing, can result in a fragility fracture, with one of the most common fracture sites being the hip [5]. Fragility fractures result from a force that would not ordinarily result in a fracture [6]. In elderly patients aged 65 and older, a hip fracture is associated with high mortality [7]. Approximately 8-10% of elderly hip fracture patients die within 30 days of surgery [8]. About 20% of older women and 37% of older men die in the year following injury [9]. Hip fracture in this elderly population also increases morbidity [7]. According to Johnston et al. [9], approximately 42% of elderly hip fracture patients will fail to return to their pre-fracture mobility, and 35% will become dependent on personal assistance or an assistive device for ambulation. These patients are four times more likely to need long-term care [9]. This population is more likely to suffer complications such as deep venous thrombosis (DVT), pulmonary embolism (PE), pneumonia (PNA), infection, bleeding, nonunion/malunion, and anesthesia-related complications [10]. Hip fractures are associated with high healthcare costs, with the total annual cost estimated at $50,508 per patient in the United States [2]. Pre-fracture comorbidities are associated with even higher costs [11]. These estimates correspond to $5.96 billion yearly in healthcare spending [2].
According to Alexiou et al. [8], a hip fracture in the elderly can severely impact physical, mental, and psychological health and diminish quality of life (QOL). Due to the high morbidity and mortality associated with a hip fracture in the elderly patient, as well as the economic and caregiver burdens of the injury, early referral to palliative care should be considered to meet the holistic needs of the patient, families and the healthcare system [7]. According to Archibald et al. [12], early palliative care referral is not routinely occurring, thus missing an opportunity to improve the quality of care. Frailty is a state of increased vulnerability to illnesses or health conditions following a stressor event such as a hip fracture, thus increasing the incidence of disability, hospitalization, long-term care, and premature mortality [12]. Frailty is characterized by increased deficits and decreased strength, endurance, and physiological function [13]. These frail, elderly patients are at increased risk of adverse events such as infection, anemia, delirium, and falls [5,10]. Frailty is associated with a 29% increase in hospital costs [3]. Frailty is also associated with increased postoperative mortality [14]. Frail patients who undergo an emergent surgical procedure are 23 times more likely than robust patients to expire on postoperative day one [14]. In the elderly hip fracture population, there is a positive correlation between frailty score and incidence of 1-year mortality [15].
Problem
Many elderly hip fracture patients experience a downward health trajectory despite being without a life-threatening diagnosis [13]. Others have multiple medical diagnoses and comorbidities [13]. A severe illness or injury, such as a hip fracture, can negatively affect QOL due to the burden of symptoms, treatment, or caregiver stress [16]. “Clinical vulnerability of older adults after hip fracture is a consequence of pre-existing frailty that is worsened as a consequence of fracture-fragility, exacerbating disability and driving poorer clinical outcomes over time” [17]. According to Archibald et al. [12], a higher level of frailty in the elderly patient is associated with increased intra-operative resource and postoperative care requirements, thus increasing the length of stay (LOS) and the likelihood of being institutionalized in a long-term care facility following discharge. Even in low-risk procedures, frail patients have a greater than three times incidence of serious complications, including sepsis, pneumonia, and delirium [14,18]. The American College of Surgeons and the American Geriatrics Society recommend that frailty screening be performed as a routine preoperative assessment on patients ≥65 years of age [12]. “The ability of acute care providers to adequately prepare for, recognize and respond to the needs of frail older adults is paramount to aiding prognosis and care plan optimization” [12]. In elective surgery, frailty evaluation can be utilized to optimize preoperative function in the individual [19,20]. Conversely, for emergency or non-elective surgery, such as hip fracture repair, frailty evaluation can trigger early discussion regarding “ceilings of care…and the futility of escalating interventions after complications…” [19]. Preoperative frailty assessment can also ensure appropriate resources are available pending surgical or postsurgical complications [20]. Despite these recommendations, providers often overlook this screening [12].
Clinical Significance
The organization participating in the project is a Magnet-recognized hospital and Level 1 Trauma Center serving as the area’s academic medical center. In the project’s setting, the hospitalist group routinely admits patients who experience a hip fracture with orthopedic consultation. These patients, specifically those 65 years and older, are not routinely screened for frailty by the hospitalist or the orthopedic group. The hospitalist or orthopedic provider can assess a patient’s perioperative risk and individualized needs by incorporating routine frailty screening [14]. The Clinical Frailty Scale (CFS) is a risk stratification tool that evaluates frailty based on comorbidity, function, and cognition to assess a numerical frailty score ranging from very fit to terminally ill [21]. By incorporating a routine frailty screening, the provider can identify patients who would benefit from early palliative care consultation.
Including palliative care in the multidisciplinary care of frail, elderly hip fracture patients is appropriate as these injuries can pose a risk to QOL [22]. Palliative care providers assist with symptom management, QOL, and advanced care planning [23,24]. The palliative care team helps patients determine the best management or treatment options considering the patient’s prognosis and can assist in providing safe and effective pain management to elderly patients [23,24]. “Recent models of optimal palliative care integration emphasize referral at diagnosis, increasing presence as time progresses, and a shift in focus toward rehabilitation and survivorship care if a patient’s illness trajectory improves or toward end-of-life care and hospice referral if their trajectory declines” [24]. Palliative care is associated with lower healthcare utilization and cost savings by honoring patients’ wishes and decreasing the number of medical procedures performed [25]. Palliative care-associated savings average $2,642 per admission for patients discharged alive and $6,896 for patients who pass away during their hospitalization [26]. Despite the benefits of palliative care, this service is often underutilized in this patient population [26]. Patients not diagnosed with cancer are less likely to receive a timely referral [24]. Barriers to the utilization of palliative care occur due to a knowledge deficit on the purpose and benefits of these services [27]. Many patients and providers are uncomfortable discussing advanced directives, leaving patients open to potentially unwanted invasive procedures in an emergency [7]. Providers may be reluctant to consult palliative care to prevent loss of hope or increased fear [27]. Additionally, palliative care is frequently mistaken for end-of-life care. According to the World Health Organization (WHO), palliative care is an approach that seeks to improve the QOL of patients and their families facing life-threatening illnesses “through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual” [16]. Radbrudh et al. [16] state that palliative care is not intended to expedite or postpone death but rather to manage symptoms. Palliative care has been shown to reduce pain symptoms and psycho-emotional stress, which correlates to higher patient satisfaction [28]. Palliative care assessment of every hip fracture patient is unrealistic due to limited resources; however, palliative care evaluation for those elderly hip fracture patients who score higher on the risk stratification scale, such as the CFS, is a practical approach [27].
Materials and Methods
This quality improvement (QI) project focuses on the principles of patient-centered care, which includes “respect for patient values, preferences, and expressed needs, coordination and integration of care, and providing emotional support alongside the alleviation of fear and anxiety associated with clinical care” [29]. Therefore, this project aims to enhance QOL by incorporating palliative care into holistic care through symptom management and patient and caregiver satisfaction [30]. These aims are accomplished by promoting open discussions regarding the goals of care and patient preferences [7].
Development of PICOT (Patient, Intervention, Comparison, Outcomes, Time) Question
The population of interest included patients aged 65 and older who had sustained a hip fracture. The primary intervention of interest was utilizing the CFS screening tool on each of these patients on admission, with a goal of at least 50% compliance with this risk assessment by the admitting provider. This intervention was compared to the current practice of not evaluating preoperative frailty in the target population, thus missing identifying those at increased risk for poor outcomes. The desired outcome included considering palliative care referrals for those who scored moderately frail and above. This project aimed to improve QOL and patient satisfaction in the target population. The project was implemented from November to December 2022, and the results were compared to the same period in 2021.
PICOT Question
In the elderly (≥years/age) hospitalized patient who experiences an acute fragility hip fracture (P), how does the implementation of the Clinical Frailty Scale (CFS) tool on hospital admission (I) compared to no frailty screening (C), increase the incidence of palliative care referral in the target population (O)?
Evidence: Review of Literature/Literature Search
A literature search was conducted with the previously mentioned PICOT question as the focus. The databases searched included PubMed and CINAHL; the search engine Google Scholar was also utilized. A PRISMA diagram (Figure 1) is included to describe the literature search. Two studies were excluded from the databases and three from the search engine due to duplication. PubMed was searched using the keywords (hip fracture AND frailty scale) and (hip fracture AND frailty). MeSH terms included the following: aged, conservative treatment, femoral fractures/therapy, femoral fractures/psychology, femoral fractures/rehabilitation, frailty/diagnosis, frailty/psychology, life expectancy, quality of life, activities of daily living, comorbidity, mobility limitation, recovery of function, walking, hip fractures/therapy, frail elderly, hip fractures/mortality, long-term care, frail elderly/statistics and numerical data, frail elderly/statistics and numerical data, decision making, hip fractures/complications, multimorbidity, and patient acceptance of health care. Boolean connectors included “Hip fracture AND frail AND mortality” and “hip fracture AND frail AND palliative care.” When limiting to publications over the past five years, PubMed revealed thirty-four studies with abstracts reviewed. Thirty-two articles were eliminated based on abstract evaluation lacking either hip fracture diagnosis or utilization of frailty scale. Two studies were retained for appraisal after being found to meet topic relevance.
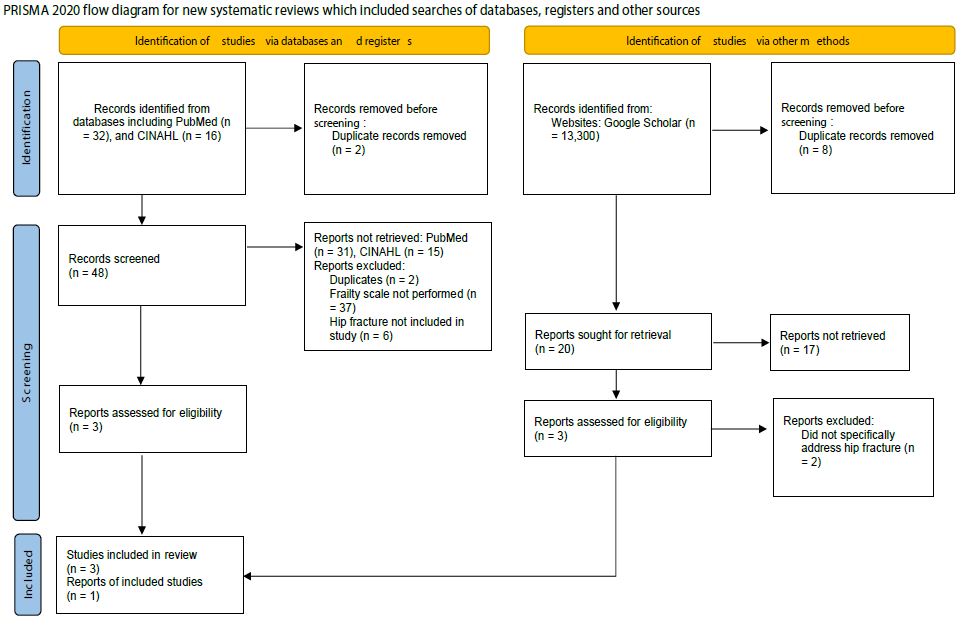
Figure 1: 1A PRISMA diagram
From : Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372:n71.
doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
CINAHL search was performed using the keywords (hip fract* AND frailty scale), (femoral neck fract* AND frailty scale), and (femoral neck fract* AND frail*). Limitations included studies from the last five years and the English language. The search revealed sixteen studies with all abstracts reviewed. Fifteen articles were eliminated, not meeting topic relevance; one was retained for appraisal. A search was conducted utilizing the Google Scholar database with the keywords “hip fracture” AND “palliative care” AND “elderly” AND “frail” AND “frailty scale.” Narrowing the studies to include the last five years and review articles revealed 23 results. Three of the studies were duplicates of a previous search. Ten articles were retained for review, and four were eliminated based on a review of the abstract; five did not contain information regarding hip fracture. One study was included for appraisal.
Evidence Synthesis
The four articles were appraised using the John Hopkins Evidenced-Based Practice Model for Nursing and Healthcare Professionals. The Research Evidence Appraisal Tool, Appendix E, was utilized for article evaluation. Each article was assigned a level and grade of evaluation, as seen in the Evaluation Table (Table 1) and Study Level and Quality Table (Table 2).
Table 1: Grade of evaluation
|
Article Citation |
Conceptual Framework and Purpose |
Design/Method |
Sample/Setting |
Major Variables Studied (and Their Definitions) |
Measurement |
Data Analysis |
Findings |
Appraisal: Worth to Practice |
| Braude, P., Carter, B., Parry, F., Ibitoye, S., Rickard, F., Walton, B., Short, R., Thompson, J., & Shipway, D. (2021). Predicting 1-year mortality after traumatic injury using the clinical frailty scale. Journal of the American Geriatrics Society, 70(1), 158-167. https://doi.org/10.1111/jgs.17472 | No conceptual framework described
Aim: to determine the effect of frailty on 1-year mortality in older adults admitted following trauma |
Observational study Level 1 Evidence Quality Grade A High Quality | Severn Major Trauma Net-work’s major trauma center based in South West England
Patients ≥ 65 years/age admitted between Nov. 2018 and Sept. 2019 with traumatic injuries (N = 585) |
DV: Mortality at 1 yearIV: Level of frailty as measured by CFS | Frailty was measured by the CFS included age, sex, comorbidities, injury type and injury severity score | CFSNumber deceased at 1-year f/u | Median age: 81 years/old55.7% female 44.3% male 50.8% living with frailty (CFS ≥ 5) At 1-year f/u 29.6% had deceased | Strengths: large sample size, easily replicated Limitations: did not include hip fracture patients, CFS scores prior to March 2019 were retro-spectively assessed.
Conclusion: Association between increasing severity of frailty and 1- year mortality (the chance of dying increased with a higher frailty score) |
Note: DV: Dependent Variable, IV: Independent Variable, CFS: Clinical Frailty Scale, f/u: Follow-Up
|
Article Citation |
Conceptual Framework and Purpose |
Design/Method |
Sample/Setting |
Major Variables Studied (and Their Definitions) |
Measurement |
Data Analysis |
Findings |
Appraisal: Worth to Practice |
| Chan, S., Wong, E. K., Ward, S. E., Kuan, D., & Wong, C. L. (2019). The predictive value of the clinical frailty scale on discharge destination and complications in older hip fracture patients. Journal of Orthopaedic Trauma, 33(10), 497- 502. https://doi.org/10.1097 /bot.000000000000 1518 | No conceptual framework described
Aim: to determine if the CFS is associated with discharge destination, in-hospital complica- tions, and length of stay following hip fracture |
Retrospective cohort study
Level 1 Evidence Quality Grade A High Quality |
Setting: Un-named academic level 1 trauma center in Canada Sample: all patients age ≥ 65 years admitted with an isolated hip fracture (N = 423) | DV1: Discharge destinationDV2: in- hospital complications
DV3: Length of stay IV: Level of frailty as measured by CFS |
Frailty was measured by the CFS
DV1 measured as either death or discharge to long-term care facility DV2 measured as presence or absence of the hospital complications DV3 measured in days of hospital admission |
Data was evaluated by comparing DVs to frailty score | Median age: 82.5 years/old
63.3% female 36.7% male
15.9% died or were d/c’d to long term facility 81.8% De-veloped at least 1 compli- cation Median LOS was 7 days |
Strengths: first study to examine the use of CFS to predict adverse outcomes
Limitations: small percentage of CFS scores determined in retrospect; universal health care which may affect discharge destinationConclusion: frailty is associated with adverse d/c destination, in-hospital complications and increased LOS |
Note: DV: Dependent Variable, IV: Independent Variable, CFS: Clinical Frailty Scale, d/c’d: Discharged
|
Article Citation |
Conceptual Framework and Purpose |
Design/Method |
Sample/Setting |
Major Variables Studied (and Their Definitions) |
Measurement |
Data Analysis |
Findings |
Appraisal: Worth to Practice |
| Chen, C., Chen, C., Wang, C., Ko, P., Chen, C., Hsieh, C., & Chiu, H. (2019). Frailty is associated with an increased risk of major adverse outcomes in elderly patients following surgical treatment of hip fracture. Scientific Reports, 9(1), 1 – 9. https://doi.org/10.1038/s41598-019-55459-2 | No conceptual framework described
Aim: to determine the effect of the level of frailty on post-operative emergency room visits, readmission, and mortality |
Observational cohort study
Level 1 Evidence Quality Grade A High Quality |
Setting: an orthopedic ward in a medical center and a district hospital in Changhua County, Taiwan Sample: Patients ≥ 50 years treated for a hip fracture (N=245) | DV1: 1-, 3-, and 6- month emergency department visits
DV2: readmission rates DV3: mortality ratesIV: level of frailty on CFS |
Frailty was measured by the CFS
DV1 measured number of emergency department visits to participating hospitals DV2 measured as readmissions to participating hospitals due to postoperative complications DV3 measured in number of all cause mortalities |
Data was evaluated by comparing DVs to frailty score at 3 points in time of the study | Prevalence of pre-frailty and frailty were markedly higher in womenFrail patients were typically older, had lower BMI, and worse cognitive function | Strengths: study examined relationships adjusted for covariates
Limitations: based on subjective data, may not represent all geographical areas
Conclusion: frailty is associated with more short-term mortality; pre-frailty was more strongly associated with early ED visits and hospital readmissions |
Note: DV: Dependent Variable, IV: Independent Variable, CFS: Clinical Frailty Scale, BMI: Body Mass Index
|
Article Citation |
Conceptual Framework and Purpose |
Design/Method |
Sample/Setting |
Major Variables Studied (and Their Definitions) |
Measurement |
Data Analysis |
Findings |
Appraisal: Worth to Practice |
| Thorne, G. & Hodgson, L. (2021). Performance of the Nottingham hip fracture score and clinical frailty scale as predictors of short and long-term outcomes: A dual-centre 3-year observational study of hip fracture patients. Journal of Bone and Mineral Metabolism, 39(3), 494-500. | No conceptual framework described
Aim: to report outcomes for patients with a hip fracture and compare the performance of the NHFS with the CFS |
Observational cohort study
Level 1 Evidence Quality Grade A
High Quality |
Setting: two non- specialist hospitals on the South Coast of England over a 3- year period from Jan. 2016 to Dec. 2018
Sample: Any patient admitted during this time frame who suffered a hip fracture (N=2,422) |
DV1: Inpatient mortality
DV2: 30-day mortality DV3: LOS IV1: NHFS score IV2: CFS score |
30-day mortality prediction after hip fracture with NHFS
Frailty measured by CFS Inpatient mortality and 30-day mortality were measured as a percentage LOS measured in days |
Data was evaluated by comparing inpatient mortality, 30-day mortality, and LOS based on CFS scoring and NHFS | Median age: 85 years 70.6% female 29.4% male
30-day mortality: 5.8%
1-year mortality: 23.5%
Average LOS: 18.0 days |
Strengths: large sample population, only study to compare NHFS and CFS in predicting mortality and \ hospital stayLimitations: 28% of patients did not have NHFS; 42% did not have CFSzConclusions:
Both CFS and NHFS are useful to predict survival rates for 1 year following injury; neither score predicted LOS |
Note: DV: Dependent Variable, IV: Independent Variable, LOS: Length of Stay, NHFS: Nottingham Hip Fracture Score, CFS: Clinical Frailty Scale.
Table 2: Study Level and Quality
|
Article 1 |
Article 2 |
Article 3 |
Article 4 |
|
| Level I
· Experimental study (RCT) · Systematic Review of RCT’s · Explanatory mixed method design that includes level I quant study |
Xa
|
Xa
|
Xa
|
Xa
|
| Level II
· Quasi-experimental study · System Review w/combination of RCTs, Quasi-exp, or quasi-exp. Only · Explanatory mixed method design that includes only Level II quant study |
||||
| Level III
· Non-experimental · Systematic Review w/combination of exp./non-exp studies · Qualitative study or meta-synthesis · Exploratory, convergent or multiphasic mixed methods · Explanatory mixed method design that includes only a level III quant study |
||||
| Level IV
Opinion of respected authorities/expert committees, or consensus panels · Clinical practice guidelines · Consensus panels · Position statements |
||||
| Level V
· Integrative/Scoping/Literature Review · QI, program, financial evaluation · Case Reports · Expert opinion |
Note: a: High Quality; b: Good Quality; c: Low Quality or Major Flaws; Article 1: Braude et al., (2021); Article 2: Chan et al., (2019); Article 3: Chen et al., (2019); Article 4: Thorne and Hodgkin, (2021).
Table 3 includes the Synthesis Table Outcomes for each study appraised. The synthesis reveals the relationship between frailty and 1-year mortality, short-term mortality, and adverse discharge destinations, including long-term institutionalization and death, in-hospital complications, LOS, early emergency department visits, and hospital readmissions following initial injury/hospitalization. Recommendations for practice change include evaluating acute hip fracture patients ≥65 years of age on a frailty scale as a predictor tool (Table 4), thus assisting the provider in identifying patients who may benefit from palliative care consultation.
Table 3: Table of Recommendation(s) for Practice Change
|
Recommendation |
References in Support of Recommendation |
Rationale |
Level of Evidence |
Quality Rating |
| 1. Patients ≥ 65
years of age experiencing an acute hip fracture should be screened on a CFS as a predictor for mortality. |
Braude et al., (2021)
Chen et al., (2019)
Thorne & Hodgson (2021) |
To identify those at risk
for 1-year or early mortality following a hip fracture as there is a positive correlation between severity of frailty and mortality. |
I |
A |
| 2. Patients ≥ 65 years of age experiencing an acute hip fracture should be screened on a frailty scale as a predictor for adverse discharge destinations, in-hospital complications, and increased LOS | Chan et al., (2019) | To identify those at risk
for adverse discharge destinations such as death or long-term institutionalization, in- hospital complications and prolonged LOS. |
I |
A |
Note: CFS: Clinical Frailty Scale, LOS: Length of Stay
Table 4: Table of Strength of Recommendation(s)
|
Recommendation |
Strength of Evidence for Recommendation |
References in Support of Recommendation |
| 1. Patients ≥ 65 years of age experiencing an acute hip fracture should be screened on a CFS as a predictor for mortality.
*Strong evidence = Strongly recommend |
Based on the JHEBP level of evidence and
quality ratings, strong & compelling evidence with consistent results was found to support organizational translation (Dang et al., 2022).
|
Braude et al., (2021)
Chen et al., (2019)
Thorne & Hodgson (2021) |
| 2. Patients ≥ 65 years of age experiencing an acute hip fracture should be screened on a frailty scale as a predictor for adverse discharge destinations, in-hospital complications, and increased LOS
*Strong evidence = Strongly recommend
|
Based on the JHEBP level of evidence and
quality ratings, strong & compelling evidence with consistent results was found to support organizational translation (Dang et al., 2022).
|
Chan et al., (2019)
|
Note: CFS: Clinical Frailty Scale, LOS: Length of Stay
Theoretical/Project Framework
The Model for Improvement guides this QI project using PDSA (Plan-Do-Study-Act) cycles. Initially, project planning included researching the evidence to determine the effectiveness of the proposed intervention. The literature demonstrates that frailty screening is recommended preoperatively for patients aged 65 and older [12]. The benefits of palliative care in frail, elderly patients, regardless of diagnosis, have been established, with improved QOL, patient and family satisfaction, and healthcare costs. Secondly, the plan was formulated. The instructions regarding implementation were widely disseminated among the hospitalist APRNs. This information detailed the scope of the project and project goals, the CFS, and the benefits of including palliative care in the multidisciplinary team caring for the frail, elderly hip fracture patient. SMART (specific, measurable, achievable, relevant, and time-bound) goals describe the project’s aim. The project took place at a university teaching hospital and included the hospitalist APRNs responsible for evaluating frailty in each elderly hip fracture patient utilizing the CFS. The APRNs were then prompted to consider palliative care consultation for patients identified as moderately frail or above. The initial goal for this project was 50% or greater compliance with the use of a CFS and palliative care consultation in the specified population. Measuring progress included evaluating the electronic health record (EHR) of those patients in the target population by measuring the use of a CFS followed by suggested recommendations for palliative care consultation when appropriate. Results were assessed throughout the project implementation to guide further education and project revisions to promote compliance.
Project Design
The project was initiated on a small scale with the hospitalist APRNs performing the CFS, with tentative plans to include all hospitalist providers pending project results. Data was collected and documented. The daily hospitalist patient logs were checked for the inclusion criteria. Once these patients were identified, EHRs were reviewed for the utilization of a CFS by the hospitalist APRNs and the subsequent palliative care referral in those deemed moderately frail and above. The data results were then compared to the same patient population and time frame from one year prior. Data were evaluated to determine the effectiveness of the project.
Implementation
The patients participating in the described project were identified by age and diagnosis, including those aged 65 years and older who sustained an acute hip or femoral neck fracture and who were admitted to the medical center by a hospitalist APRN. On admission, these patients were evaluated for frailty utilizing the CFS. Palliative care consultation was recommended for those scoring moderately frail (6) or above. SWOT (strengths, weaknesses, opportunities, and threats) analysis was conducted on the projected project. Strengths identified included the support of the palliative care team and the hospitalist group. An additional strength was the recommendation of the American College of Surgeons and the American Geriatrics Society to perform frailty screening routinely preoperatively on patients ≥ 65 years [12]. A project weakness included resistance to change by providers within the hospitalist group and misconceptions regarding palliative care. There was concern among providers that frailty screening would be time-consuming and burdensome. Additionally, providers often deferred/refrained from initiating palliative care referrals for fear that their patients would give up hope in their recovery [27]. Some providers misconstrued palliative care as end-of-life care [16]. These weaknesses were mitigated by incorporating education regarding the benefits of palliative care and frailty screening.
By including palliative care providers in the care planning of these patients within the target population, this project provided opportunities for improvement in the patient’s QOL, patient and caregiver satisfaction [31], and healthcare costs [25]. The interdisciplinary care promoted by this project encouraged patient-centered care through the holistic shared management of healthcare challenges [32]. The concern about eliminating potential operative cases from the orthopedic service was a potential threat. This threat was reduced by communicating with the orthopedic team the goals of care, including promoting patient-centered care with optimal surgical recovery based on the patient’s and family’s personal preferences. Barriers identified included increased time and workload, negative attitudes towards change, and the potential for ineffective communication regarding project goals and implementation. Mitigating actions included acknowledging concerns and reinforcing project goals, benefits, patient-centeredness, and cost-effectiveness. The project’s facilitators included multidisciplinary collaborations, communication, and teamwork. The project’s hospitalist group is a large medical group within a university medical center with various expert specialties and consultants. There is excellent teamwork between the hospitalist group and consulting services, such as orthopedics and palliative care, with open communication. Team leaders from the hospitalist service supported the project.
Stakeholders and Project Team
The project team included the Doctoral of Nursing Practice (DNP) student, hospitalist APRNs, palliative care providers, the medical center’s nursing and ancillary staff, the DNP project chair, the DNP project committee member, and the statistician. This multidisciplinary team worked together to provide patient-centered and cost-effective quality care. The CFS was disseminated among the hospitalist APRNs. Instructions regarding implementation were distributed via email and in person to all hospitalist APRNs detailing the project’s scope, project goals, and the benefits of including palliative care in the multidisciplinary team caring for the frail, elderly hip fracture patient. Implementation of the project began in November 2022, with data collection and evaluation from November 1, 2022 – December 31, 2022. Pre-implementation data was also obtained from November 1, 2021 – December 31, 2021. Pre- and post-implementation data included age in years, gender, race, and time of visit. Additional post-implementation data included utilization of CFS, ranking on CFS, risk identified, and referral to palliative care if appropriate. Data was collected via the hospitalist’s daily census reports and EHR chart review. No patient identifiers were required, collected, or saved; therefore, Institutional Review Board (IRB) approval was unnecessary.
Results and Discussion
The frailty assessment was evaluated on the CFS, with frailty measured numerically from 1 (very fit) to 9 (terminally ill) [21]. A study by Rockwood et al. [33] shows a high correlation between the judgment-based CFS and the mathematically based Frailty Index (FI), with a Pearson coefficient of 0.80 and p < 0.01. There is an excellent consistency of the CFS with an experienced geriatric medicine specialist’s opinion (Cohen’s K: 0.80, p < 0.0001) [34]. There is a strong inter-rater reliability (Cohen’s K: 0.811, p < 0.001) and a strong test-retest reliability utilizing the CFS (Cohen’s K: 1.0, p < 0.001) [34]. Data collected for this project included the patient’s age, gender, race, CFS score, month of admission, eligibility, CFS used (yes/no), risk identified (yes/no), and palliative care referral (yes/no) based on findings. The total palliative care referral numbers were compared to the same data from one year prior during the same period. The goal outcome was palliative care referral for those elderly frail hip fracture patients who score moderately frail or above (CFS ≥ 6). Meeting this goal outcome represents QI, with the expected results being improved patient and family satisfaction and reduced healthcare costs.
Findings
During the pre-implementation period from November – December 2021, 24 patients met the criteria with admission by the hospitalist APRNs. Of those 24 patients, only one received a palliative care referral during their hospitalization. In comparison, during project implementation from November – December 2022, 19 patients met the same specified criteria. The CFS risk assessment was performed on 13 of these 19 patients. This number equates to 68.4% compliance with the utilization of the risk assessment tool, surpassing the goal of 50%. Seven of these 13 assessed patients were deemed less than moderately frail, scoring ≤ 5 on the CFS assessment performed by the admitting APRN. Therefore, palliative care referral was not recommended for these seven low-frailty patients. Six of these 13 patients were moderately frail or above (CSF ≥ 6). Four of these six patients with a CFS score of ≥ 6 received the recommended palliative care referral. Based on this data, there was 84.6% compliance with appropriately placed palliative care referrals. Of the 13 patients assessed for frailty, the APRNs performing the assessment appropriately followed the referral recommendations for 11 patients (Table 5).
Table 5: Results
|
Year |
Number in specified population admitted by hospitalist APRN |
Number in specified population in which CFS was utilized |
Number of those assessed scoring ≥ 6 (moderately frail or above) on CFS |
Number in target population receiving palliative care referral |
| 2021 |
24 |
N/A |
N/A |
1 |
| 2022 |
19 |
13 |
6 |
4 |
Note: APRN: Advanced Practice Registered Nurse, CFS: Clinical Frailty Scale
Implications for Practice/Policy
The goal of this project is to identify those patients who are considered frail by utilizing a CFS on all hip fracture patients within the target population who are admitted to the medical center by the hospitalist service as recommended by the American College of Surgeons and the American Geriatrics Society [12]. These frail patients are considered at high-risk for complications and mortality [5,7], which may affect the patient or caregiver’s QOL due to symptom burden, caregiver stress, and complex treatment options [16]. Palliative care referral is recommended for those patients in the target population who score moderately frail and above (CFS ≥ 6). This QI project is intended to improve patient and caregiver QOL and reduce healthcare costs. Palliative care assists with symptom management and advanced care planning, promoting QOL by identifying and respecting the patient’s personal goals of care [23]. Palliative care is also associated with lowered healthcare utilization and costs, saving an average of $2,642 – $6,896 per patient by respecting the individual’s wishes regarding the plan of care [26]. The study’s strengths included the excellent collaboration between the hospitalist group and the palliative care team. Numerous studies also show the superiority of the CFS over other frailty assessments and a positive correlation between a higher frailty score and morbidity and mortality. Limitations include the small sample size and provider subjectivity of the CFS scoring. Additionally, the study only evaluated elderly patients who had sustained an acute hip fracture and did not address additional types of injuries or surgical procedures. Another limitation includes a lack of evaluation of long-term outcomes, including the patient’s perceived QOL or patient and caregiver satisfaction following palliative care consultation.
References
- Lewiecki ME, Wright NC, Curtis JR, Siris E, Gagel RF, et al. (2017). Hip fracture trends in the United States, 2002 to 2015. Osteoporos Int 29: 717-722.
- Adeyemi A, Delhougne G (2019) Incidence and economic burden of intertrochanteric fracture. JBJS Open Access 4: 1-6. [crossref]
- Kwak M, Digbeu B, Des Bordes J, Rianon N (2022) The association of frailty with clinical and economic outcomes among hospitalized older adults with hip fracture surgery. Osteoporos Int 33: 1477-1484. [crossref]
- Arshi A, Rezzadeh K, Stavrakis AI, Bukata SV, Zeegen EN (2019) Standardized hospital-based care programs improve geriatric hip fracture outcomes: An analysis of the ACS NSQIP targeted hip fracture series. J Orthop Trauma 33: e223-e228. [crossref]
- Pioli G, Bendini C, Pignedoli P, Giusti A, Marsh D (2018). Orthogeriatric Co-management – managing frailty as well as fragility. Inj 49: 1398-1402.
- Kani KK, Porrino JA, Mulcahy H, Chew FS (2018). Fragility fractures of the proximal femur: Review and update for radiologists. Skeletal Radiol 48: 29-45. [crossref]
- Koso RE, Sheets C, Richardson WJ, & Galanos AN (2018). Hip fracture in the elderly patients: A Sentinel event. Am J Hosp Palliat Care 35: 612-619. [crossref]
- Alexiou K, Roushias A, Varitimidis S, Malizos, K (2018). Quality of life and psychological consequences in elderly patients after a hip fracture: A review. Clin Interv Aging 13: 143-150. [crossref]
- Johnston CB, Holleran A, Ong T, McVeigh U, Ames E (2018). Hip fracture in the setting of limited life expectancy: The importance of considering goals of care and prognosis. J Palliat Med 21: 1069-1073. [crossref]
- Cannada LK, Mears SC, Quatman C (2020). Clinical Faceoff: When should patients 65 years of age and older have surgery for hip fractures, and when is it a bad idea?. Clin Orthop Relat Res 479: 24-27. [crossref]
- Allsop S, Morphet J, Lee S, Cook O (2020). Exploring the roles of advanced practice nurses in the care of patients following fragility hip fracture: A systematic review. J Adv Nurs 77: 2166-2184. [crossref]
- Archibald MM, Lawless M, Gill TK, Chehade MJ (2020). Orthopaedic [sic] surgeons’ perceptions of frailty and frailty screening. BMC Geriatr 20: 1-11. [crossref]
- Stow D, Spiers G, Matthews FE, Hanratty B (2019). What is the evidence that people with frailty have needs for palliative care at the end of life? A systematic review and narrative synthesis. Palliat Med 33: 399-414. [crossref]
- Nidadavolu LS, Ehrlich AL, Sieber FE, Oh ES (2020). Preoperative evaluation of the frail patient. Anesth Analg 130: 1493-1503. [crossref]
- Traven SA, Reeves RA, Althoff AD, Slone HS, Walton ZJ (2019). New five-factor modified frailty index predicts morbidity and mortality in geriatric hip fractures. J Orthop Trauma 33(7): 319-323. [crossref]
- Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, et al. (2020). Redefining palliative care – A new consensus-based definition. J Pain and Symptom Manage 60: 754-764. [crossref]
- Pizzonia M, Giannotti C, Carmisciano L, Signori A, Rosa G, Santolini F, et al. (2020). Frailty assessment, hip fracture and long‐term clinical outcomes in older adults. Eur J Clin Invest 51: 1-9. [crossref]
- Zhang X, Jiao J, Xie X, Wu X (2021). The association between frailty and delirium among hospitalized patients: An updated meta-analysis. J Am Med Dir Assoc 22: 527-534. [crossref]
- Dhesi JK, Lees NP, Partridge JS (2019). Frailty in the perioperative setting. Clin Med 19: 485-489. [crossref]
- Lee S, Nam J, Kim Y, Kim M, Choi J, et al. (2021). Predictive model for the assessment of preoperative frailty risk in the elderly. J Clin Med 10: 4612. [crossref]
- Church S, Rogers E, Rockwood K, Theou O (2020). A scoping review of the clinical frailty scale. BMC Geriatr 20: 1-18. [crossref]
- Sullivan NM, Blake LE, George M, Mears SC (2019). Palliative care in the hip fracture patient. Geriatr Orthop Surg & Rehabil 10: 1-7. [crossref]
- Harries L, Moore A, Kendall C, Stanger S, Stringfellow TD, et al. (2020). Attitudes to palliative care in patients with neck-of-femur fracture—A multicenter survey. Geriatr Orthop Surg Rehabil 11: 1-7. [crossref]
- Santivasi WL, Partain DK, Whitford KJ (2019). The role of geriatric palliative care in hospitalized older adults. Hosp Pract 48: 37-47. [crossref]
- Sampaio SG, Motta LB, Caldas CP (2019). Value-based medicine and palliative care: How do they converge?. Expert Rev Pharmacoecon Outcomes Res 19: 509-515. [crossref]
- Konda SR, Lott A, Egol KA (2020). Development of a value-based algorithm for inpatient triage of elderly hip fracture patients. J Am Acad Orthop Surg 28: e566-e572. [crossref]
- Davies A, Tilston T, Walsh K, Kelly, M (2018). Is there a role for early palliative intervention in frail older patients with a neck of femur fracture?. Geriatr Orthop Surg Rehabil 9: 1-6. [crossref]
- Flöther L, Pötzsch B, Jung M, Jung R, Bucher M, et al. (2021). Treatment effects of palliative care consultation and patient contentment. Med 100: 1-6. [crossref]
- Finkelman A (2022) Quality improvement: A guide for integration in nursing (2nd ed.), Jones & Bartlett Learning, Burlington, MA Chan S, Wong EK, Ward SE, Kuan D, Wong CL (2019). The predictive value of the clinical frailty scale on discharge destination and complications in older hip fracture patients. J Orthop Trauma 33: 497-502.
- Porter AS, Harman S, Lakin JR (2020). Power and perils of prediction in palliative care. Lancet 395: 680-681. [crossref]
- Flaherty C, Fox K, McDonah D, Murphy J (2018). Palliative care screening: Appraisal of a tool to identify patients’ symptom management and advance care planning needs. Palliat Care 22: E92-E96. [crossref]
- Poitras M, Maltais M, Bestard-Denommé L, Stewart M, Fortin M (2018). What are the effective elements in patient-centered and multimorbidity care? A scoping review. BMC Health Serv Res 18: 1-9. [crossref]
- Rockwood K, Song X, MacKnight C, Bergman H, Hogan D, et al. (2005). A global clinical measure of fitness and frailty in elderly people. CMAJ 173: 489-495. [crossref]
- Özsürekci C, Balcı C, Kızılarslanoğlu MC, Çalışkan H, Tuna Doğrul R, et al. (2019). An important problem in an aging country: Identifying the frailty via 9-point clinical frailty scale. Acta Clinica Belgica 75: 200-204. [crossref]