DOI: 10.31038/IJNM.2025613
Abstract
Introduction: Rapid changes in health care, innovative technologies and the emergence of new knowledge have led to the need for nurses to continue to learn and develop throughout their careers to keep their knowledge, skills, and competencies up to date. However, nurses are confronted by various barriers to continuing their professional education. There is limited research about these barriers in the Eswatini context. Therefore, this study explored the barriers to continuing nursing education among nurses in one hospital in the Lubombo region of Eswatini.
Methods: A descriptive qualitative design was employed. Ten purposively selected nurses participated in the study. Face-to-face, in-depth, semi- structured interviews were used to collect data. The audio-recorded interviews were transcribed verbatim. Thematic analysis guided by Braun and Clarke’s method was applied.
Findings: Participants understood the value of continuing nursing education. However, participants encountered barriers which included lack of time, staff shortages, poor remuneration, lack of distance learning options, and absence of training leave. Lack of job security was also a barrier reported by participants. Participants suggested that employing more nurses, job security assurance, and financial support could motivate nurses to further their studies.
Conclusions: There is a need for the Ministry of Health to collaborate with healthcare facilities and nursing education institutions to create an enabling environment for continuing professional education for nurses. Further research needs to investigate factors that hinder employers from allowing nurses to further their education.
Keywords
Barriers, Competencies, Continuing nursing education, Employer, Nurses
Introduction
In the rapidly changing healthcare context, continuing professional education (CPE) is essential for healthcare professionals to provide person-centered, safe, and effective care. King et al. (2021) [1]. Continuing professional education is a life-long learning approach whereby healthcare professionals acquire knowledge and skills to maintain competency in their field of practice [2]. The goal of CPE is to contribute to healthcare professionals’ career advancement, improved financial income, professional networks, and personal skills [3]. Continuing professional education is central to nurses’ lifelong learning and is vital for keeping their knowledge and skills up-to-date [4]. In nursing practice, CPE is essential to improve quality of care, promote nurses’ resilience and increase readiness to face emerging and re-emerging healthcare challenges [5].
Studies show that knowledge gained through basic professional education has a half-life of 2.5 years and needs to be updated at the end of this period. Moreover, such training will expire five years after graduation; hence, deprivation of CPE can lead to poor quality patient care and death [6]. Identifying continuing professional development needs is the nurse’s responsibility, and interpreting those needs is the nurse manager’s responsibility [5]. Self-motivation, relevance to practice, preference for workplace learning, strong enabling leadership, and a positive workplace culture are key factors that positively influence CPE for nurses. Moreover, nurses embark on continuing education when they have a reason to do so [7]. For nurses, engaging in CPE can be mandatory or voluntary. Mandatory CPE occurs when regulatory organizations set compulsory conditions for nurses to transition from their initial to higher qualifications [4]. CPE promotes motivation, commitment, and nurses’ retention and performance [7]. Evidence has shown that nurses do not always engage in continuing education and that CPE does not always address nurses’ real needs (Vázquez-Calatayud et al., 2021). Reasons for not engaging in nursing CPE include time limitations, fatigue, lack of motivation, and poor working conditions. Additional reasons include an organizational culture characterized by a lack of leadership and collegial support, an inability to apply new knowledge in practice, distant learning sessions from the workplace, and educational programs not adapted to nurses’ needs [8]. Barriers to continued nursing education have several negative consequences for the nursing profession. Limited access to ongoing education can hinder career advancement opportunities for nurses, leading to decreased job satisfaction and lower professional retention rates [4]. The lack of updated knowledge and skills may result in suboptimal patient care outcomes, affecting patient safety and the quality of healthcare delivery [9]. Additionally, the profession’s overall growth and development may be stunted when nurses cannot contribute to research, innovation, and the adoption of new evidence-based practices [7]. To fulfil the primary goal of enhancing quality care, international organisations recommend strengthening the human capital by engaging in professional development initiatives for nurses. Basic nursing training alone is insufficient, especially because nurses are occasionally confronted with unpredictable care situations in highly complex patient-care environments. Thus, there is an unequivocal global consensus regarding nurses’ need for continuing education [9]. Continuing nursing education will protect the public and improve the quality of care and services. Lack of nursing CPE negatively influences quality of patient care, job satisfaction, recruitment, and retention [10]. Although continuing nursing education is beneficial [4], there is a paucity of research on the barriers to CPE in Eswatini. Therefore, the study explored barriers to continuing nursing education in Eswatini. Exploring barriers to CNE in a resource-limited country provides insight into the socio-politico-economic climate that influences professional development for nurses.
Methods
Research Question
The central question in this study was: “What are the barriers to continuing nursing education in one hospital in Eswatini?”
Study Design
This was a descriptive qualitative study. This design was chosen to paint a clear picture of a little-known phenomenon. The descriptive qualitative design recognizes the phenomenon’s subjective nature and helps researchers contribute to change and quality improvement in clinical settings [11]. The Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines were used to report this qualitative study [12].
Research Setting
The study was conducted in a public regional referral hospital in the Kingdom of Eswatini. The hospital has 400 beds and approximately 500 outpatients seen by healthcare professionals daily. The following services are provided in the hospital: psychiatric and mental healthcare, outpatient care, maternal and child healthcare, surgery, oncology, general medicine, HIV testing, and treatment. The hospital also provides palliative care, dental, audiology, physiotherapy, and occupational therapy services. The setting was conveniently selected because it is the lead author’s clinical placement hospital. Different nursing cadres, which include nursing assistants, general nurses, and specialist nurses, are employed in the hospital.
Sampling Method and Procedure
The participants included nurses who were full-time employees at the hospital, working at least 40 hours per week, and had been working for more than six months. Participants were purposively sampled to select participants in the best position to answer the research question [13]. Following permission from the hospital to conduct the study, the lead author recruited the participants by visiting the different hospital units to explain the purpose and value of the study. Nurses willing to participate were given an information leaflet, and dates and times were scheduled to answer questions related to the study, sign informed consent, and plan a venue and time for the interviews.
Data Collection and Management
The lead author, a male university lecturer with a postgraduate qualification and clinical experience in critical care nursing, visited the participants who volunteered in their units. This visit aimed to explain the value of the study and answer participants’ questions before signing the informed consent form. Before primary data collection, the second author conducted two pilot face-to-face interviews with participants in the same research setting using a semi-structured interview guide developed by the research team. The flexible nature of face-to-face interviews allows researchers to explore in-depth information from participants [14]. Pilot interviews help identify and rectify poorly structured or offensive questions that reveal researcher biases [15]. The interview guide contained questions that explored the barriers to continuing nursing education. No questions were changed after the pilot interviews; therefore, the data were included in the data analysis. The questions were: 1) What is the value of continuing nursing education? 2) What are the barriers to continuing nursing education in your view?. The interviews were conducted at times that the participants selected to avoid disrupting patient care. Data saturation was attained after the ninth interview, and an additional interview was conducted to verify the saturation. After data collection, all the interviews were transcribed verbatim and sent to the lead author for review. The second author has clinical experience in community and mental health nursing. The second author was not a supervisor to the participants; hence, the participants did not feel coerced to participate in the study. Following data collection, the interview transcripts and audio recordings were encrypted and stored in a password-protected computer accessible only to the research team.
Data Analysis
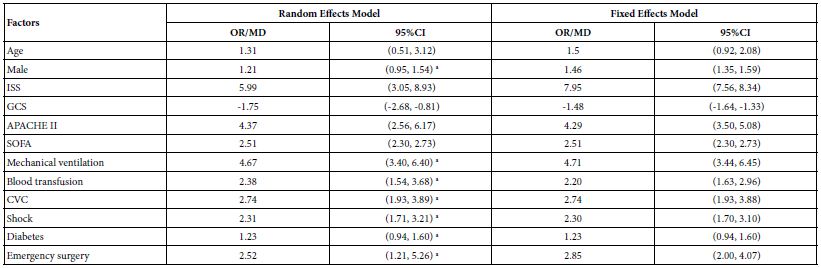
The interviews were transcribed verbatim using Microsoft Office Word 365. Thematic analysis guided by the Braun and Clarke (2006) [16] method was applied (Table 1).
Table 1: Application of Braun and Clarke’s data analysis method.
|
Braun and Clarke’s steps
|
Application in the present study
|
| Step 1: Familiarizing oneself with the data |
The co-authors read and reread the transcripts, listened to the interview recordings, and wrote down word-for-word what was captured in the audio recordings. |
| Step 2: Generating initial codes |
The co-authors used short phrases to code the data. Similar codes were then sorted into categories. |
| Step 3: Searching for themes |
The co-authors searched for themes by identifying shared categories in participants’ responses. |
| Step 4: Reviewing themes |
The co-authors reviewed the themes to refine and discard unnecessary themes. |
| Step 5: Defining and naming themes |
The co-authors defined and assigned names to themes to clarify emerging findings. |
| Step 6: Writing a descriptive research report |
The second author wrote the research report, which the lead author reviewed. |
Trustworthiness
Trustworthiness was maintained using Lincoln and Guba’s (1985) credibility, dependability, confirmability, and transferability strategies. Credibility was maintained through prolonged engagement, whereby the researcher met with nurses before data collection and during the interviews. Member checking was performed when the interview transcripts were verified with the participants, who confirmed that the findings reflected their perceptions and experiences. Transferability was enhanced through purposive sampling and by describing the participants’ demographic profile and the research setting. Additionally, the research methodology was described in detail. An audit trail that comprehensively described steps for collecting, organizing, and analyzing the data was provided to enhance dependability. Confirmability was maintained by providing adequate and relevant direct verbal quotations from the participants to support the findings.
Ethical Considerations
Ethical approval was granted by the Eswatini Health and Human Research Review Board (FWA00026661/IRB00011253/SHR004/2024). The hospital’s administration also granted permission to conduct the study, and participants received oral and written information concerning the study. Participants further signed consent forms indicating their willingness to participate. The participants were informed that participation was completely voluntary and that they could withdraw their informed consent at any time when they desired to do so. To maintain anonymity and confidentiality, participants were assured that pseudonyms would be used in the research report. Furthermore, the lead author did not ask questions that caused emotional or psychological harm to participants.
Findings
Participants’ Characteristics
Ten face-to-face interviews were conducted with diverse nursing cadres from January 2024 to June 2024, each lasting approximately 30 to 45 minutes. Table 2 shows the participants’ demographic characteristics.
Table 2: Summary of participants’ demographic characteristics.
|
Participant
|
Age (in years) |
Sex |
Highest qualification |
Work Experience
|
|
1
|
34
|
Female |
Diploma in General Nursing |
10 years
|
|
2
|
29
|
Male |
Diploma in General Nursing |
3 years
|
|
3
|
27
|
Female |
Certificate in Nursing Assistance |
3 years
|
|
4
|
29
|
Male |
Certificate in Nursing Assistance |
1 year
|
|
5
|
26
|
Male |
Diploma in General Nursing |
3 years
|
|
6
|
27
|
Female |
Certificate in Nursing Assistance |
4 years
|
|
7
|
32
|
Female |
Diploma in General Nursing |
6 years
|
|
8
|
34
|
Female |
Diploma in General Nursing |
7 years
|
|
9
|
25
|
Female |
Certificate in Nursing Assistance |
3 years
|
|
10
|
34
|
Male |
Diploma in General Nursing |
10 years
|
Themes and Subthemes
The data analysis revealed three themes and 10 associated subthemes (Table 3).
Table 3: The data analysis revealed three themes and 10 associated subthemes.
|
Themes
|
Subthemes
|
| Understanding the value of continuing nursing education |
Updating professional knowledge |
| Improving clinical skills |
| Perceived barriers to continuing education |
Staff shortage and lack of time |
| Remuneration mismatch |
| Financial difficulties |
| Lack of training leave and open distance learning opportunities |
| Uncertain job security |
| Suggestions for recognition of nurses’ continuing education |
Ensuring adequate nursing staff |
| Provision of study leave and job security |
| Financial support |
Theme 1: Understanding the Value of Continuing Nursing Education
This theme describes the participants’ understanding of the value of continuing nursing education. Participants revealed that continuing education improved their professional competencies and skills in providing patient care. Two subthemes were developed, namely 1) updating professional knowledge and 2) improving clinical skills.
Subtheme 1: Updating Professional Knowledge. Participants verbalised that continuing nursing education is meant to enhance their professional knowledge in patient care. This view by participants reflects the recognition of using up-to-date and evidence-based knowledge to provide patient care:
“…. nursing is dynamic and one needs to equip him or herself with the current knowledge, current guidelines and the technology, new drugs that are introduced, and new procedures” [Participant 8].
“Basically, since nursing is a dynamic sector… and evolving, so as a healthcare practitioner you have to be up to date and be updated on the current standards of the profession for you to be able to continue providing quality care” [Participant 5].
The participants responses demonstrate an understanding of the ever-evolving nature of healthcare that requires up-to-date knowledge to improve patient outcomes.
Subtheme 2: Improving Clinical Skills. The participants verbalised that continuing nursing education contributes to improvement of clinical skills. The participants’ reports highlight the significance of updating nursing skills to enhance patient assessment, diagnosis, and treatment of diverse diseases:
“…I’ll make an example with us nursing assistants it happens that there are procedures that we want to do but our scope restricts us …so by furthering our studies we will be more qualified to do those procedures which we are currently restricted from doing… we will be able to learn new things that are occurring in health… indeed it is important” [Participant 6].
“…to get updated skills and be competent so that they [nurses] can be able to render nursing care to save patients’ lives” [Participant 8].
These collective responses by participants demonstrate the nature of continuing education in enhancing performance of nursing skills that match their current qualifications to enhance holistic patient care.
Theme 2: Perceived Barriers to Continuing Education
This theme related to participants’ perceived barriers to continuing their education. The perceived barriers hinder their attempts to improve competencies in providing quality patient care. Five subthemes emerged: 1) staff shortage and lack of time, 2) remuneration mismatch, 3) financial difficulties, 4) lack of training leave and open distance learning opportunities, and 5) uncertain job security.
Subtheme 1: Staff Shortage and Lack of Time. Participants voiced that staff shortages in the hospital resulted in a lack of time and opportunities to further their education. The insights highlight that a shortage of staff leads to tight work schedules that hinder professional development:
“… currently in our facility, we have shortage with the staff which makes it difficult for one to pursue their studies because of the shortage” [Participant 2].
“…it can be the issue of staffing ratio…you find that there are these nurses who want to further their studies in the facility, but they can’t leave the work and continue with their education … and the schedule is not friendly” [Participant 4].
Collectively, the participant’s responses reflect the role played by staff shortages and tight work schedules in inhibiting professional development opportunities.
Subtheme 2: Remuneration Mismatch. The participants expressed the mismatch between the upgraded qualifications and salary hindered their professional development. According to the participants, this situation discouraged them from continuing their education. These perceptions reflect poor recognition of upgraded education by the employer:
“…another thing it’s the lack of motivation, since people who go and further their studies are doing the very same job…and getting the same salary” [Participant 1].
“Like I said in the beginning, the first barrier is that you will go to further your education and come back here to earn a lower salary… let me make an example, they will hire you as a degree nurse and you will do that degree job yet you get paid for a diploma qualification” [Participant 3].
The responses by participants jointly indicate that poor remuneration demotivates nurses from engaging in professional development trainings.
Subtheme 3: Financial Difficulties. Shortage of finances was reported by participants as a barrier to their professional development. Hence, participants would not be able to keep up with higher education costs as there were no scholarships to assist them:
“I think it’s…our government and the ministry of health…they do not [financially] support part-time education…whereby you are still working and still studying” [Participant 5].
“Another barrier could be finances…most of us nurses want to enrol for education and continue to learn but we are breadwinners… then it becomes difficult for one to continue [with their education] because you have to provide for your family, and you have to pay for your school fees at the same time” [Participant 9].
These participant responses reflect that higher education fees and increased family responsibilities do not favour continuing education endeavours among nurses.
Subtheme 4: Lack of Training Leave and Open Distance Learning Opportunities. The participants verbalised that lack of open distance learning opportunities hindered their continuing education endeavours. These views demonstrate that the nature of nursing programmes offered by higher education institutions was instrumental in enhancing professional development among nurses:
“…my only barrier is that for nursing assistants, you need to resign completely and then you go back to school because there is no study leave for us…and the nursing degree is offered full-time [Participant 4].
“…when you want to continue with nursing education you need to resign first and there is no study leave or distance learning for nurses, so it becomes difficult…” [Participant 10].
These responses jointly reflect that study leave is essential for all nursing cadres in hospitals to enable them to engage in their professional development initiatives.
Subtheme 5: Uncertain Job Security. Participants reported that uncertain job security hindered them from continuing their education. According to the participants, there was no assurance that they would still return to their jobs after upgrading their education. These insights highlight lack of support from employers concerning nurses’ professional development:
“… also, there is no job security…so you ask yourself so many times that should I resign and go to study…and then when I come back who is going to employ me, where and when, who is going to take care of my kids, who is going to take care of my family whilst I am looking for a [new] job?” [Participant 2]
“…and the job security – you can’t just leave your post and go to further your studies because you might not know whether you will be employed or not when you come back, so for me it’s that.” [Participant 5].
These participant responses jointly demonstrate that employers are not visionary regarding nurses’ professional development. Job insecurity reflects an unsupportive working environment in the hospital.
Theme 3: Suggestions for Recognition of Nurses’ Continuing Education
This theme describes suggestions from participants concerning the recognition of nurses’ continuing education by employers and the Ministry of Health. An environment that supports professional development recognises the need to implement interventions to improve patient outcomes. Three subthemes were developed: 1) ensuring adequate nursing staff, 2) providing study leave and job security, and 3) financial support.
Subtheme 1: Ensuring Adequate Nursing Staff. Participants verbalised that employers need to hire more nursing staff. According to the participants, this would create room for other nurses to continue their education while others fill their spaces in the working area:
“…it lies with the employer to try as much as possible to…to employ more nurses in order to cover up the shortage” [Participant 8].
“I think…this facility…with the nursing management board has to consider the issue of the staffing ratio so that nurses can have some spare time and continue with their education…” [Participant 4].
These responses jointly highlight that adequate nursing staff is important as nurses are able to take turns and partake in continuing education.
Subtheme 2: Provision of Study Leave and Job Security. Participants verbalised that employers’ assurance of job security can promote continuing education among nurses. According to the participants, they would be motivated to learn because they would still return to their jobs immediately after completing their studies:
“…they have to allow the nurse to go study, maybe they pay like 75% of the salary while the nurse is studying and then when he or she comes back he will be able to get his job back with an agreement which says maybe you can work for 4 years before you look for greener pastures” [Participant 2].
“…let them (nurses) go and study then hire them when they return and deduct funds from their salaries [while they are studying] – yes, I think that can work out” [Participant 3].
The collective participants’ insights reflect that motivation to engage in continuing education relies on efforts by employers who need to provide job security for nurses.
Subtheme 3: Financial Support. The participants expressed the need for financial support from the government and the Ministry of Health to assist in their professional development. These views indicate that governments need to support nurses in continuing education to improve the citizens’ quality of care:
“… government can provide the finances for the nurses for their extra educational courses… I think in that way we can bridge the current problem within nursing education my sister…” [Participant 4].
“…they [health institutions and government] should fund nurses, especially nursing assistants – let them go and study” [Participant 3].
Collectively, the participants’ responses show the role that the government can play in meeting the need for nurses to engage in continuing education.
Discussion
The study has provided insight into barriers to continuing nursing education in a developing country. Despite the obstacles to continuing education, participants clearly understood its value. The findings of this study support those of research conducted by Tachtsoglou et al. (2020) [17] among Greek nurses, which reported that the main reason for continuing education was acquiring new professional knowledge. Additionally, the findings of this study support those of another study conducted in two hospitals in southeast Morocco, which revealed that participants’ motivation for continuing education was mainly intrinsic factors, which included improving professional competence and knowledge [9]. These findings highlight the dynamic nature of healthcare and nursing practice, which always places a need upon nurses to upgrade their knowledge to keep up with developments in healthcare. Additionally, nurses’ desire for continuing professional education needs to be met with appropriate in-service education programs and workshops and a supportive environment to enable their professional development. Continuing nursing education is necessary in the face of scientific and technological advancements, which require the acquisition of new knowledge, improved skills, and the renewal of clinical practices [6]. In their examination of nurses’ motivation to continue their education, [18] found that the most crucial reason was improving professional competence, skills, and patient care. This finding suggests that nurses value enhancing their knowledge and skills to provide patients with the best care.
In line with the findings of this study, [18] found that the high workload resulting from staff shortages in nursing care units was one of the main reasons for nurses not to further their studies, resulting in exhaustion and lack of time to focus on studies. Similarly, [19] revealed that people with a heavy workload and family responsibilities might struggle to find time to further their studies. These findings reflect the need for nurse managers and employers to reduce nurses’ workload by proportionately distributing tasks in the different units. Additionally, Mbombi and Mothiba (2020) [19] reported that participants felt that the Department of Health attached no value to postgraduate qualifications because they did not increase one’s salary upon completion of the degree and, therefore, were demotivated to enrol for an advanced nursing degree. Career progression and financial rewards have been established as the most important motives for nurses to enrol in further studies [4]. Therefore, a lack of remuneration for nurses after acquiring additional nursing qualifications may discourage other nurses from enrolling in programmes meant to increase their qualifications as there are no increased financial benefits after obtaining an additional qualification. The findings of this study also support the assertion that advanced nursing courses may be costly, and as a result, lack of finances becomes a significant barrier to enrolling in an additional qualification [21,22]. Financial constraints due to minimal salaries and insufficient financial support from healthcare institutions hinder nurses from furthering their studies. Additionally, tuition, textbooks, and travel expenses often deter nurses from continuing their education.
Barriers to enrolment in further studies can also be institutional. According to Lhbibani et al. (2021) [6], barriers to continuing education that can be imposed by learning institutions include scheduling problems; lack of interesting, practical or relevant courses; procedural problems, time requirements; and inadequate information about programs and procedures. Hence, lack of workplace policies supporting educational leave can discourage nurses from pursuing further education. Lack of security of continuing to be employees of the organization after completing their education is also a barrier to nurses’ professional development. The requirement for nurses to resign from their posts in order to pursue further studies has become a significant barrier because, as the World Bank (2023) [23] noted, due to low recruitment post-training, employment opportunities for newly qualified nurses are limited in most sub-Saharan countries, including Eswatini. The barriers to continuing nursing education, from the personal to the national level, have dire consequences for patients and the healthcare system. Patient care errors can result from inadequately qualified nurses, and the healthcare system may fail to sufficiently meet the population’s needs.
In line with our findings, nurses in another study verbalized the need for their management to hire more staff to deal with staff shortages in order to avoid nurses missing out on important workshops and education programs [21]. Moreover, a study conducted by Munasinghe et al. (2023) [24] to explore the opportunities and challenges in lifelong learning and continuing professional development among nurses in Sri Lanka found that expanding the workforce to address shortage of nurses and provide more opportunities for professional development was viewed as one of the most essential strategies for facilitating increased participation of nurses in continuing education. Therefore, adequate staffing and flexible work shifts are important enablers or facilitators for nurses furthering their education. The availability of sufficient support systems, including management support, mentorship programs, realistic opportunities for professional development, and workplace policies for awarding study leave, are significant enablers for continuing professional education among nurses. Therefore, there is a need for organizational policies that promote and facilitate nurses’ continued education. Sponsorship from employment organizations is a major facilitator of continuing nursing education among nurses [25]. Governments and financial institutions must support nurses in furthering their education.
Implications of the Study
The study findings highlight the need for employers to develop training plans, promotional strategies, and reward systems that can enable nurses to further their education. Moreover, the Ministry of Health needs to formulate policies that enable nurses to continue their education, including providing financial support, adequate staff, and the award of study leave. Nurses also need to develop a desire to continue their education and identify programmes that will meet their professional development needs.
Strengths and Limitations
One strength is that the study has provided insight into the barriers to continuing nursing education in a developing country characterised by resource limitations. Moreover, the qualitative approach has provided an in-depth exploration of the barriers from the nurses’ perspectives. One limitation is that the study included only nurses; hence, factors that hinder other healthcare professionals from furthering their education were not explored. The qualitative approach also limited the generalisability of the findings to the entire population of nurses.
Conclusions
Although participants understood the value of continuing education, they encountered barriers which included staff shortages, financial challenges, lack of job security, time, and distance education. Absence of study leave was also identified as a barrier. Personal, workplace, and health system challenges hinder nurses from continuing their education. Nurses who do not further their education are more likely to provide poor quality care that is not evidence-based. Therefore, poor patient outcomes occur, thus bringing the nursing profession to disrepute. Governments need to design frameworks that enable nurses to further their education while being able to retain their employment. Nurse-training institutions should design flexible programmes that allow nurses to further their education while employed. Future research needs to investigate employers’ factors that hinder nurses from furthering their education.
References
- King R, Taylor B, Talpur A, Jackson C, Manley K, et al. (2021) Factors that optimise the impact of continuing professional development in nursing: A rapid evidence review. Nurse Education Today 98. [crossref]
- Curran V, Gustafson DL, Simmons K, Lannon H, Wang C, et al. (2019) Adult learners’ perceptions of self-directed learning and digital technology usage in continuing professional education: An update for the digital age. Journal of Adult and Continuing Education. 25: 74-93. [crossref]
- Julian JFE, Ruiz FB (2020) Continuing professional development (CPD) among educators in selected Colleges of Nursing: Perceived importance, impact, and challenges. Enfermería Clínica 30: 60-64.
- Mlambo M, Silén C, McGrath C (2021). Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature. BMC Nursing. 20: 1-13. [crossref]
- Longhini J, Rossettini G, Palese A (2021) Massive open online courses for nurses’ and healthcare professionals’ continuous education: A scoping review. International Nursing Review. 68: 108-121. [crossref]
- Lhbibani A. Lamiri A, Lotfi S, Tridane M, Belaaouad S (2021) Factors hampering the participation of nursing staff in the continuing education activities of hospitals centers in the Casablanca-Settat region. The Open Nursing Journal 15.
- Vázquez-Calatayud M, Errasti-Ibarrondo B, Choperena A (2021). Nurses’ continuing professional development: A systematic literature review. Nurse Education in Practice 50. [crossref]
- Bit-Lian Y, Woei-Ling T, Nachiappen S, Jajali NFM (2022). Factors affecting participation of registered nurses in continuing nursing education among selected private pospital in Penang, Malaysia. The Malaysian Journal of Nursing (MJN). 14: 82-89.
- Ait Ali D, Fazaz M, Ounaceur B, El Houate B, El Koutbi M, et al. (2023). Motivational factors influencing nurses’ participation in continuing education sessions: A hospital-based study. Journal of Adult and Continuing Education. 29: 395-407.
- Hakvoort L, Dikken J, Cramer-Kruit J, Molendijk-van Nieuwenhuyzen K, van der Schaaf M, et al. (2022). Factors that influence continuing professional development over a nursing career: A scoping review. Nurse education in practice 65. [crossref]
- Doyle L, McCabe C, Keogh B, Brady A, McCann M (2020). An overview of the qualitative descriptive design within nursing research. Journal of Research in Nursing, 25: 443-455. [crossref]
- Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care. 19: 349-357.
- Nanjundeswaraswamy T, Divakar S (2021) Determination of sample size and sampling methods in applied research. Proceedings on Engineering Sciences. 3: 25-32.
- Gray JR, Grove SK (2024) Burns & Grove’s the practice of nursing research: Appraisal, synthesis, and generation of evidence. St. Louis, Missouri, Elsevier, Inc.
- Naz N, Gulab F, Aslam M (2022) Development of qualitative semi-structured interview guide for case study research. Competitive Social Science Research Journal 3: 42–52.
- Braun V, Clarke V (2006) Using thematic analysis in psychology. Qualitative research in psychology. 3: 77-101.
- Tachtsoglou, K., Zioga, O., Iliadis, C., Frantzana, A., & Lambrini, K. (2020). Factors affecting nurses ‘ lifelong learning. International Journal of Health Administration and Education Congress (Sanitas Magisterium) 6: 1-9.
- Tsirigoti A, León-Mantero C, Jiménez-Fanjul N (2024) Motivation for continuing education in nursing. Educación Médica 25.
- Mbombi M, Mothiba T (2020) Exploring barriers that nurses experience to enrolment for a postgraduate nursing qualification at a higher education institution in South Africa. African Journal of Health Professions Education, 12: 41-45.
- Fang, D., Bednash, G. D., & Arietti, R. (2016). Identifying barriers and facilitators to nurse faculty careers for PhD nursing students. Journal of Professional Nursing. 32: 193-201. [crossref]
- Nyelisani M, Makhado L, Luhalima T (2023) Professional nurses’ experiences regarding continuing professional development (CPD) opportunities at public hospitals of Limpopo province, South Africa. Sage Open 13.
- Rocco TS, Smith MC, Mizzi RC, Merriweather LR, Hawley JD (2023) The handbook of adult and continuing education. Taylor & Francis.
- World Bank (2023). Global healthcare workers: Education, mobility, and financing.
- Munasinghe HK, Suraweera KAVS, Weerakkody WADH, Hiruni Kanchana U, Marikar FMMT (2023) Opportunities and challenges in lifelong learning and continuing professional development among nurses at a cancer hospital in Sri Lanka. Journal of Healthcare Administration 2: 61-85.
- Palma JAFS, Oducado RMF, Palma BS (2020) Continuing professional development: Awareness, attitude, facilitators, and barriers among nurses in the Philippines. Nursing Practice Today. 7: 198-207.