Abstract
Aim: Some nursing approaches are required to combat the problems that occur in patients due to the physical and psychosocial effects of diseases. It is aimed to address the areas where virtual reality glasses, which are frequently used as a distraction, are used as a current approach in nursing care.
Methods: The studies about virtual reality glasses in nursing care between 2008-2019 were scanned and the definition, purpose of use and the areas of use of virtual reality glasses were evaluated in the context of the role / responsibilities of the nurse and presented in the article.
Results: Diseases cause physical, social and psychological problems by affecting the daily life activities of individuals and decrease the quality of life. Current nursing care applied to control the negative effects of diseases; it increases the quality of life of individuals, their compliance with treatment, their ability to cope with the disease, and reduces the negative effects of treatment. Since the negative effects experienced by individuals during the disease cause changes in life, effective coping methods are required. As a coping method; With the use of virtual reality glasses, it is possible for the individual to move away from the situation, not to think about the disease and to feel in a different place. Virtual reality goggles can enable individuals to cope with symptoms associated with illnesses, as they are an effective tool in addressing more than one sensation at the same time and reducing sensations from around.
Conclusion: Nurses should guide the determination of the symptoms affecting patients and patients in care, and the determination of current methods to reduce these symptoms.
Keywords
Virtual reality glasses, Maintenance, Nursing
Introduction
Technological developments in health in recent years have necessitated new practices in nursing care. In care practices, nurses primarily tend to practices that will increase the quality of care and create the continuity of care. In our age, with the increase in the use of technology in the health system, different service areas have emerged and it has made it compulsory for nurses to innovate in the care they apply in order to be effective in solving health-related problems. Similar to the world, nursing practices in our country; Factors such as the increasing use of technology in the health system, innovations in information, the increase in the number of chronic patients, the symptoms caused by diseases and the elderly population [1,2]. Nurses have to follow current approaches in care and use them in practice in order to improve the quality of care they apply. For this purpose, it will contribute to the planning of nursing interventions aimed at increasing the time allocated to care, providing individualized care, ensuring the adaptation process to the disease, reducing the symptoms caused by the treatments and increasing the quality of life in health services provided by using virtual reality glasses in nursing practices [3-5].
Method of Research
Inclusion Criteria
- The results are research on the use of virtual reality glasses in nursing care,
- The publication language is Turkish or English,
- Published in the last ten years (2008-2018),
- Access to the full text. Randomized Controlled studies (RCTs) and quasi-experimental studies (YÇ) were included in the study.
Reasons for not Including in the Study
Studies examining virtual reality applications outside of nursing, observation studies and reviews were not included in the study. Due to the determination of up-to-date information, the studies carried out in the last eleven years were included in the research, and the studies conducted before 2008 were not included. Studies whose titles or abstracts are not clear, whose full texts cannot be accessed and whose publication language is not Turkish/English are not included.
Researching and Selecting Studies
Sample Definition
The studies were selected by scanning the databases of May 2019- June 2020 “Cochrane”, “OVID”, “Pubmed”, “Medline”, “Wiley Online Library”, “Google Scholar” and “YÖKSİS Theses”. Virtual reality glasses (VR), virtual reality glasses, nursing keywords were used. Master’s and doctoral theses, studies in nursing journals were also included in the research. The titles and abstracts of all studies found by electronic scanning were impartially examined by the researchers. Each of the selected articles covers research on the evaluation of methods in different areas of nursing care related to virtual reality glasses.
Discussion
The disease, which forces all the balances and harmony of individuals, appears both acutely and chronically. Both the disease and its side effects adversely affect the daily life activities of individuals and cause many problems. Especially psychosocial problems are among the problems that have the most negative impact on the individual.
Psychosocial problems that cannot be noticed in the early stages of the disease; It can negatively affect the individual’s satisfaction, quality of life, adherence to treatment, and coping with the disease and its symptoms. In addition, because of the psychosocial problems experienced by the individual, the meaning of his life, can affect their functionality and satisfaction with the place where they live [6,7].
Psychosocial problems experienced by individuals during the illness require effective coping methods because they create life changes. Current nursing interventions should be applied as a coping method in order to control and reduce the problems experienced by the individual [8]. Virtual reality glasses, one of the current nursing initiatives; It is widely used in nursing care to reduce the side effects of diseases by providing the opportunity to control health/disease conditions and to create therapeutic environments [3,9,10].
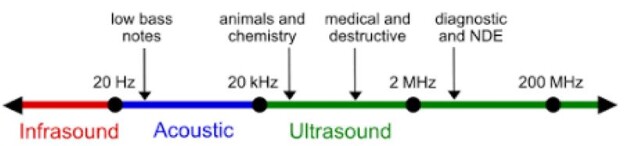
Virtual reality glasses is a computer simulation technique that allows individuals to hear and feel the sounds and stimuli with the headset they watch [9-11].
With virtual reality glasses, consisting of a pair of glasses connected to a mobile phone from a head-mounted screen, the individual gets away from the environment and concentrates his attention on the image and perceives himself as if he is in another place with this five-dimensional glasses [9,12]. The most basic feature that distinguishes virtual reality glasses from similar applications is that they make individuals feel real. Virtual reality glasses are a method of watching images taken from the computer in order to isolate the individual from real life for a while [12,13].
With the virtual reality glasses, different types of content such as 360-degree videos, games, movies and animation can be watched. Since these videos are created in 360 degrees, no matter which direction a glasses wearer looks, the feeling of being in the virtual world and being there lives. Thus, by concentrating his attention in a different place, the individual moves away from the visual, tactile and sensory stimuli around him.
It is thought that virtual reality applications reduce the physical and psychosocial effects of diseases [10]. Changing the user’s attention away from the symptoms of the disease interprets an incoming signal as well as changing the pathway, reducing symptom-related brain activity (Sil et al., 2014) [14]. In addition, using virtual reality can target cognitive and emotional pain pathways, thereby reducing pain intensity, distress, and anxiety by changing how pain signals are processed in the central nervous system. This distraction is achieved by a number of mechanisms such as editing the virtual reality image and reduced pain [15,16].
The use of virtual reality glasses in the field of health, which was originally designed for entertainment purposes, has recently increased [17,18]. With the developments in computer technologies, virtual reality is a new technique of focusing attention in another direction, which is frequently used to reduce physical and psychosocial symptoms during some applications (_nal and Canbulat, 2015; Sil et al., 2014; Guo et al.)
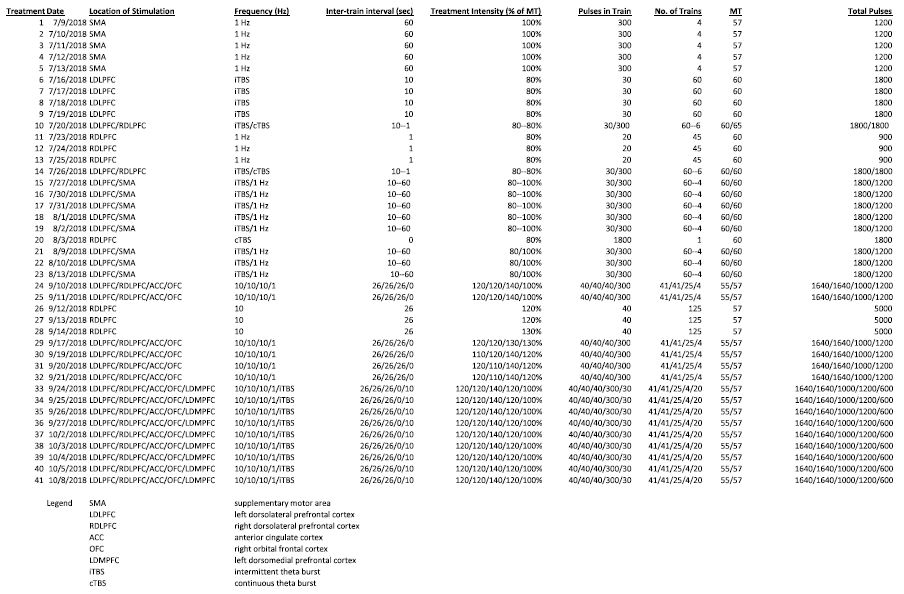
In the studies examined in the literature, virtual reality glasses; It is used as a current care approach in orthopedic surgery, dressing changes in patients with burns, invasive procedures, perioperative period, pain-inducing interventions, interventions such as lumbar puncture, endoscopy, labor pain, breast biopsy, arteriovenous fistula, cystoscopy and chemotherapy [3,19-24]. Virtual reality glasses, which are cheap to apply and use, have no side effects, and are effective in physical, psychological, social, emotional and spiritual healing, are a current application that can be preferred in nursing care with these features.
Sander et al (2002), in their study to determine the effect of virtual reality glasses applied during lumbar puncture in adolescents on the level of pain; virtual reality glasses during lumbar puncture for 17 patients in the study group; Only lumbar puncture was performed in 13 patients in the control group. As a result of the study, the level of pain was found to be significantly lower in the adolescents who were applied virtual reality glasses compared to the adolescents in the control group [25].
Wolitsky et al. (2005) in their study to determine the effect of virtual reality glasses on pain and anxiety levels during painful interventions in children; 10 children in the study group watched videos with virtual reality glasses for less than 5 minutes; Only the procedure was applied to 10 children in the control group. As a result of the study, it was determined that the pain and anxiety levels of the patients who were applied virtual reality glasses were significantly reduced [19].
In the study of Schneider and Hood (2007), they examined the effect of virtual reality glasses applied to patients with breast, colon and lung cancer who received first-cycle chemotherapy treatment on symptom distress, fatigue and anxiety levels; Videos were watched with virtual reality glasses during chemotherapy treatment (45-90 minutes) to 123 patients. It was observed that the application of virtual reality glasses in patients was effective in changing the perception of time and reducing the level of anxiety and fatigue, but it was not effective in relieving symptom distress [20].
Sharar et al. (2007) found that there was a significant amount of relief in their research in which they looked at the effect of virtual reality glasses on pain during physical therapy after burns [26].
Morris et al (2010) examined the effect of virtual reality glasses on pain and anxiety levels in adult burn patients receiving physiotherapy treatment; Two sessions, one in which virtual reality glasses were applied and one that was not applied, were given to 11 patients. As a result of the study, it was determined that the application of virtual reality glasses significantly reduced the level of pain and anxiety [27].
In the study of Schmitt et al. (2011) in which they examined the effect of virtual reality glasses on pain level in pediatric burn treatment,. patients were treated with virtual reality glasses for 5 sessions. As a result of the study, it was determined that the application of virtual reality glasses significantly reduced the level of pain [28].
Schneider et al. (2011) determined that the virtual reality glasses applied to 137 breast, lung and colon cancer patients who received chemotherapy treatment is an application that attracts attention, as well as a tool that reduces the anxiety and fatigue level of the patients who are applied virtual reality glasses and makes the time pass faster in the treatment process [29].
Espinoza et al. (2012) 41-85 It was determined that virtual reality glasses applied to 33 cancer patients receiving ambulatory chemotherapy were effective in reducing depression and anxiety levels and increasing the level of happiness [30].
Banos et al. (2013) It was determined that virtual reality glasses applied to 33 cancer patients hospitalized in the oncology service increased positive emotions and decreased negative emotions [13].
JahaniShoorab et al (2015) in their study to examine the effect of virtual reality glasses on pain level during episiotomy repair in women who gave birth for the first time; Videos were watched with virtual reality glasses during episiotomy to 15 women in the study group, and only episiotomy was applied to 15 women in the control group. As a result of the study, it was determined that the level of pain in women who applied virtual reality glasses was statistically significantly reduced [31].
Guo et al (2015) in their study to examine the effect of virtual reality glasses on pain level during dressing change in patients with hand injuries; Videos were watched with virtual reality glasses during dressing change to 49 patients in the study group, and only dressings were changed to 49 patients in the control group. As a result of the study, it was determined that the pain level of patients who were applied virtual reality glasses was statistically significantly reduced [14].
In the study conducted by Karaman (2016) to examine the effect of virtual reality glasses applied during breast biopsy in women on pain and anxiety levels; During the breast biopsy procedure, 30 women in the study group watched videos with virtual reality glasses, and 30 women in the control group underwent routine breast biopsy. As a result of the study, pain and anxiety levels of women who were applied virtual reality glasses were found to be significantly lower than women in the control group [23].
Ryu et al (2018) in their study to examine the effect of virtual reality glasses applied in the preoperative period on the level of anxiety in children; A 4-minute virtual reality video showing the operating room and describing the perioperative process was watched by 43 patients in the study group, and a routine explanation was given to 43 patients in the control group about the perioperative period. As a result of the study, the anxiety level of children who were applied virtual reality glasses was found to be significantly lower than the children in the control group [32].
In the study conducted by Chen et al. (2019) to examine the effect of virtual reality glasses applied during intravenous injection in the emergency room on the level of fear and pain in school-age (7-12 years old) children; In the study group, 18 children were watched by virtual reality glasses during the intravenous injection procedure, and only intravenous injection was applied to 18 children in the control group. As a result of the study, the fear and pain scores of the children who were applied virtual reality glasses were found to be significantly lower than the children in the control group [33-37].
Conclusion
Nursing; While it used to be a profession only for providing care and comfort, the changes in nursing have focused on preventing diseases and promoting health, and it has increasingly expanded roles. In parallel with the changing innovations and the system, it has become necessary to apply current approaches in nursing care in order to fulfill the expectations of the world. Since virtual reality glasses, which is one of the current approaches, is a tool that provides the ability to stimulate more than one sense at the same time and reduce the senses coming from the environment, it can help individuals to cope with the symptoms of the disease by diverting their attention.
References
- Birol L (2013) Hemşirelik Süreci Hemşirelik Bakımında Sistematik Yaklaşım. İzmir: Berke Ofset Matbaacılık.
- Karaca A, Durna Z (2018) Hemşirelik Bakım Kalitesi ve İlişkili Faktörler. Sağlık ve Toplum 28.
- Malloy KM, Milling LS (2010) The Effectiveness of virtual reality distraction for pain reduction: A systematic Review. Clinical Psychology Review 30: 1011-1018. [crossref]
- Akgün Şahin Z, Kardaş Özdemir F (2014) Hastaların hemşirelik bakımından memnuniyet düzeyleri. İzm Üniv Tıp Derg 2: 1-10.
- Cerit B (2016) Hastaların hemşirelik bakımından memnuniyet düzeyi. Hacettepe Üniversitesi Hemşirelik Fakültesi Dergisi 27-36.
- Townsend CM (2016) Ruh Sağlığı ve Psikiyatri Hemşireliğinin Temelleri Kanıta Dayalı Uygulama Bakım Kavramları (6. Baskı) içinde (C. T. Özcan, N. Gürhan, çev.) (s. 608-643). Ankara: Akademisyen Tıp Kitabevi.
- Aksan AT, Gizir CA (2017) Sağlık psikolojik danışmanlığı çerçevesinde meme kanserli kadınların yaşantıları ve psiko-sosyal gereksinimleri. Mersin Üniversitesi Eğitim Fakültesi Dergisi 13: 977-999.
- Özveren H (2011) Ağrı kontrolünde farmakolojik olmayan yöntemler. Hacettepe Üniversitesi Sağlık Bilimleri Fakültesi Hemşirelik Dergisi 1: 83-92.
- İnal S, Canbulut N (2015) Çocuklarda işlemsel ağrı yönetiminde dikkati başka yöne çekme yöntemlerinin kullanılması. The Journal of Current Pediatrics 13: 116-121.
- Youngjun K, Hannah K, Yong OK (2017) Virtual reality and augmented reality in plastic surgery: a review. Arch Plast Surg 44: 179-187. [crossref]
- Schneider SM, Paul MP, Allen MJ, Silverman P, Talaba D (2004) Virtual reality as a distraction ıntervention for women receiving chemotherapy. Oncology Nursing Forum 31: 81-88. [crossref]
- Freitas DMDO, Spadoni VS (2019) Is virtual reality useful for pain management in patients who undergo medical procedures? Einstein (Sao Paulo) 17. [crossref]
- Banos RM, Espinoza M, Palacios AG, Esquerdo G, Barrajón E, et al. (2013) A positive psychological intervention using virtual reality for patients with advanced cancer in a hospital setting: a pilot study to assess feasibility. Support Care Cancer 21: 263-270. [crossref]
- Guo C, Deng H, Yang J (2015) Effect of virtual reality distraction on pain among patients with hand injury undergoing dressing change. J Clin Nurs 24: 115-120. [crossref]
- Lambert V, Matthews A, Hicks P, et al. (2013) Virtual reality simulation for reducing pain in children. The Cochrane Library 1-11.
- Pratiw IG, Husin F, Ganiem AR, Susiarno H, Arifin A, et al. (2017) The Effect of virtual reality on pain in primiparity women. International Journal of Nursing and Health Science 4: 46-50.
- Won AS, Bailey J, Bailenson J, Tataru C, Yoon IA, et al. (2017) Immersive virtual reality for pediatric pain. Children (Basel) 234: 52. [crossref]
- Atzori B, Hoffman HG, Vagnoli L, Messeri A, Grotto RL (2019) Virtual reality as distraction technique for pain management in children and adolescents. In Advanced Methodologies and Technologies in Medicine and Healthcare 483-494.
- Wolitzky K, Fivush R, Zimand E, Hodges L, Rothbaum B (2005) Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychol Health 20: 817-824.
- Schneider SM, Hood LE (2007) Virtual reality: a distraction intervention for chemotherapy. Oncology Nursing Forum 34: 39-46. [crossref]
- Schneider SM, Kisby C, Flint E (2011) Effect of virtual reality on time perception in patients receiving chemotherapy. Support Care Cancer 19: 555-564. [crossref]
- Walker MR, Kallingal GJ, Musser JE, Folen R, Stetz MC, et al. (2014) Treatment Eficacy of virtual reality distraction in the reduction of pain and anxiety during cystoscopy. Military Medicine 179: 891-896. [crossref]
- Karaman D (2016) Meme biyopsisi sırasında sanal gerçeklik uygulamasının ağrı ve anksiyete üzerine etkisi. Yüksek lisans tezi, Bülent Ecevit Üniversitesi, Zonguldak.
- Chan PY, Scharf S (2017) Virtual reality as an adjunctive non pharmacological sedative during orthopedic surgery under regional anesthesia. İnternational Anesthesia Research Society 30: 1-3. [crossref]
- Sander WS, Eshelman D, Steele J, Guzzetta CE (2002) Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer. Oncol Nurs Forum 29: E8-E15. [crossref]
- Sharar SR, Carrougher GJ, Nakamura D, Hoffman HG, Blough DK, et al. (2007) Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: Preliminary results from 3 ongoing studies. Arch Phys Med Rehabil 88: 43-49. [crossref]
- Morris LD, Louw QA, Crous LC (2010) Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing country. BURNS 36: 659-664. [crossref]
- Schmitt YS, Hoffman HG, Blough DK, Patterson DR, Jensen MP, et al. (2011) A randomized, Controlled Trial Of İmmersive Virtual Reality Analgesia, During Physical Therapy For Pediatric Burns. BURNS 37: 61-68. [crossref]
- Schneider SM, Kisby C, Flint E (2011) Effect of virtual reality on time perception in patients receiving chemotherapy. Support Care Cancer 19: 555-564. [crossref]
- Espinoza M, Baños RM, García-Palacios A, Cervera JM, Esquerdo G, et al. (2012) Promotion of emotional wellbeing in oncology inpatients using VR. Stud Health Technol Inform 181: 53-57. [crossref]
- JahaniShoorab N, Ebrahimzadeh Zagami S, Nahvi A, Mazluom SR, Golmakani N, et al. (2015) The Effect of Virtual Reality on Pain in Primiparity. Iran J Med Sci 40: 219-224. [crossref]
- Ryu JH, Oh AY, Yoo HJ, Kim JH, Park JW, et al. (2018) The effect of an immersive virtual reality tour of the operating theater on emergence delirium in children undergoing general anesthesia: A randomized controlled trial. Pediatric Anesthesia 29: 98-105. [crossref]
- Chen YJ, Cheng SF, Lee PC, Lai CH, Hou IC, et al. (2019) Distraction using virtual reality for children during intravenous injections in an emergency department: A randomized trial. J Clin Nurs 1: 1-8. [crossref]
- Allday E (2016) For children in pain, virtual reality offers dolphins and hope. San Francisco Chronicle.
- Arane K, Behboudi A, Goldman RD (2017) Virtual reality for pain and anxiety management in children. Can Fam Physician 63: 932-934. [crossref]
- Bukola IM, Paula D (2018) The Effectiveness of distraction as procedural pain management technique in pediatric oncology patients: a meta-analysis and systematic review. Journal of Pain and Symptom Management 54: 589-600.e1. [crossref]
- Chan E, Foster S, Sambell R, Leong P (2018) Clinical efficacy of virtual reality for acute procedural pain management: A systematic review and meta-analysis. Plos One 1-13. [crossref]