Abstract
Background: Inadequate bowel preparation before a colonoscopy is troublesome for patients and costly for healthcare. Therefore, some patients are hospitalized for bowel preparation, but the number of patients and criteria involved in decision-making vary.
Aim: To investigate the variables included in decision-making concerning whether patients should be hospitalized for bowel preparation before colonoscopy.
Methods: Qualitative dynamic system modeling, including interviews with patients, nurses, and physicians and examining guidelines
Findings: The decision to offer hospitalization for bowel preparation was discussed only in a few cases with patients, and there was no dialogue with primary care. The decision was based on guidelines, rules of thumb, and healthcare professionals’ subjective judgment and did not follow evidence-based criteria.
Conclusion: Several factors, such as dialogue across healthcare sectors, involving patients in decision-making and adjusting clinical guidelines, were identified in the model that can be used to improve clinical practice and the experiences of patients.
Keywords
Clinical decision making, Colonoscopy, Qualitative
Introduction
Worldwide, colonoscopy is the most common method for diagnosing diseases of the intestinal mucosa, such as cancer or inflammatory conditions [1]. The number of colonoscopies is steadily increasing in most countries [2]. Likewise, in Denmark, where the implementation of a screening program for colorectal cancer for the population between the ages of 50 and 74 years has significantly increased the number of colonoscopies [3]. To ensure adequate visualization of the intestinal mucosa and thereby optimize the possibility of successful diagnosis and treatment during the colonoscopy, bowel preparation is crucial [4]. Bowel preparation implies that the patient must follow specific diet restrictions and consume laxatives to achieve successful bowel cleansing [5]. Most patients manage bowel preparation at home, while some patients are hospitalized, but overall patients experience bowel preparation as unpleasant and challenging due to uncontrolled diarrhoea, nausea, and sleep deprivation [6,7]. A guideline from the European Society of Gastrointestinal Endoscopy highlights that 18–35% of bowel preparation is inadequate in patients undergoing colonoscopy [8]. Notably, a study found that outpatients had more adequate bowel preparations than inpatients [9]. In the context of three major gastroenterology centres in the Capital Region of Denmark, the complex challenges of daily decision-making concerning the management of the growing number of colonoscopies and the shortage of available hospital beds have been identified. An overview of the number of colonoscopies at each of the three hospitals and the number of patients hospitalized for bowel preparation are illustrated in Table 1.
This study aimed to investigate the variables included in the decision and to determine whether patients were offered hospitalization for bowel preparation.
Table 1: Overview of colonoscopies and hospitalizations for bowel preparation at three hospitals in Denmark
|
Site |
Colonoscopies per year (2020) |
Colonoscopies per month # |
Hospitalization for bowel preparation n (%) # |
||||
| HGH |
5689 |
475 |
477 |
490 |
15 (3.2) |
12 (2.5) |
12 (2.4) |
| AHH |
7500 |
361 |
422 |
459 |
34 (9.4) |
29 (6.9) |
40 (8.7) |
| BFH |
5581 |
430 |
521 |
535 |
29 (6.7) |
22 (4.2) |
26 (4.9) |
HGH: Herlev and Gentofte Hospital, AHH Amager and Hvidovre Hospital, BFH Bispebjerg and Frederiksberg hospital.
#Numbers from HGH and AHH are from April, May, and June 2021, and numbers from BFH are from January, February, and March 2022.
Methods
Design
We developed a descriptive model based on participatory system modelling (SDM) to explore the interactions between variables included in the process of deciding if a patient is offered hospitalization for bowel cleansing [10]. The intended outcome was to help stakeholders illustrate the process of decision-making, and thereby also highlight potential areas for improvement of the process. SDM is a method used to explore and understand complex decision-making involving multiple actors [10]. In the data collection phase, this entails identifying the current and potential decision-makers, understanding their influence and rationale behind the decision-making. Relevant policies and guidelines are also considered as part of the data. The data was analyzed and discussed using a qualitative approach. This study was conducted in the Capital Region in Denmark at the Departments of Gastroenterology at three university hospitals: Herlev and Gentofte Hospital (HGH), Amager and Hvidovre Hospital (AHH), and Frederiksberg and Bispebjerg Hospital (FBH).
Data Collection
Data were collected from March to June 2021 and included patients admitted for bowel preparation before colonoscopy, above 18 years of age, capable of giving informed consent, and able to speak and understand Danish. Patients were contacted after admittance and before bowel preparation. After obtaining informed consent, the time for a telephone interview was agreed upon with the patient one or two days after discharge. The interviews included questions on experiences of hospital admission and bowel preparation, as well as data on patients’ living conditions, support from primary care, and functional status (using the Barthel Index for Activities of Daily Living (ADL)) [11]. Data regarding patients’ age, gender, diagnosis, and cause for colonoscopy were obtained from the patients’ medical records. Physicians’ and nurses’ written documentation regarding their considerations and reasoning on whether this patient should be hospitalized for bowel preparation and, their knowledge of clinical guidelines. Ward managers’ experiences and general views on hospital admission for bowel preparation were investigated at each hospital through individual interviews. In the cases where the patients received help from home care, primary care nurses in the municipality were interviewed by telephone regarding their views on the possibility of the patients carrying out bowel preparation at home. Clinical guidelines at the three hospitals were collected to identify formal criteria for admission for bowel preparation.
Data Analysis
The analytic process developed continuously alongside the data collection. First, we identified key variables that potentially influenced the decision for hospitalization. The basic structure of a model was first agreed upon by the group of authors. A template was developed from which data were collected. In an iterative process, the data were discussed and analyzed at each group meeting. The analysis focused on the development of a descriptive model; therefore, data were grouped into categories and re-grouped until the model was clear. The process continued until a consensus was reached on the final model.
Ethics
All patients were informed orally and in writing about the project, after which they provided informed consent and agreed to have their anonymized responses published. Healthcare professionals were informed orally and agreed to have their anonymized responses published. Permission to store data confidentially was obtained from the Danish Data Protection Agency (ID no: P-2020-1172). According to Danish law, no formal ethical approval was needed for this study.
Results
A model of the decision process and related variables in the decision on hospitalization before colonoscopy was developed (Figure 1). The study included 17 patients (5 from HGH, 3 from FBH, and 9 from AHH). The median age of the patients was 74 years (ranging from 50 to 86), of whom 10 were male. The demographics of the participating patients are shown in Table 2. Of those involved in the decision-making process, 10 physicians and 12 nurses were also included. Two of the physicians were the patient’s family physician, and 10 were hospital-employed physicians from the Departments of Gastroenterology. The 12 nurses were employed in outpatient clinics and had between 1 and 15 years of experience in the specialty of gastroenterology. Furthermore, nine nurses from the municipalities were contacted. Management at the departments was interviewed at the hospitals.
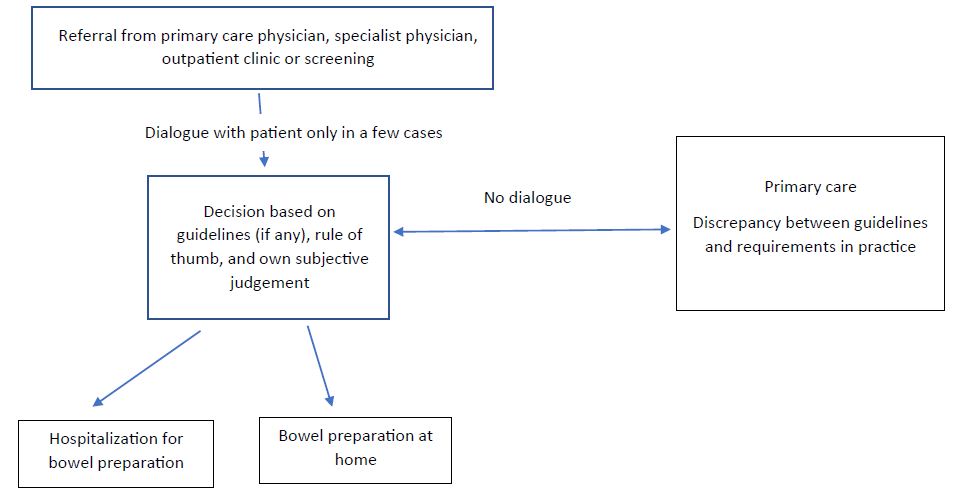
Figure 1: A flow chart model of the decision process for patients to either stay at home or be hospitalized for bowel preparation before a colonoscopy
Table 2: Demographics of the participating patients
|
Number |
Age (years) |
Gender |
Cohabitating |
Housing type |
Home care services |
Bartell score |
Cause of referral for colonoscopy |
|
1 |
80 |
male |
no |
sheltered housing | medication |
18 |
suspected colorectal cancer |
|
2 |
85 |
female |
no |
apartment | none |
20 |
suspected colorectal cancer |
|
3 |
74 |
female |
no |
apartment | cleaning, shopping, food preparation, laundry, medication, treatment of ulcer, personal hygiene, and mobilization |
10 |
diarrhea, reduced appetite, weight loss |
|
4 |
64 |
female |
no |
apartment | cleaning |
20 |
suspected colorectal cancer |
|
5 |
74 |
female |
no |
house | tube feeding 4 times a day |
20 |
bleeding from the rectum |
|
6 |
70 |
female |
yes |
house | none |
20 |
abdominal pain and bleeding from the rectum |
|
7 |
81 |
male |
no |
apartment | cleaning, shopping, and laundry |
18 |
diarrhea for several weeks |
|
8 |
74 |
female |
no |
house | help for anti-embolism stockings twice a day and wound care twice a week |
19 |
suspected colorectal cancer |
|
9 |
69 |
male |
no |
apartment | personal hygiene daily, bath two times a week, cleaning every 14 days |
18 |
suspected colorectal cancer |
|
10 |
76 |
male |
yes |
house | change of bladder catheter every ten week |
16 |
abdominal pain, weight loss, suspected colorectal cancer |
|
11 |
63 |
male |
no |
house | every morning for medicine, cleaning every 14 days. |
18 |
removal of polyps |
|
12 |
83 |
female |
yes |
house | shower once a week, medicine and food delivery twice a week, and incontinence treatment daily |
15 |
alternating bowel movements |
|
13 |
82 |
male |
no |
nursing home | medication, help with personal hygiene, and mobilization every day |
5 |
suspected colorectal cancer |
|
14 |
50 |
male |
no |
apartment | cleaning every other week |
20 |
suspected colorectal cancer |
|
15 |
81 |
male |
no |
house | cleaning every other week |
20 |
diarrhea for six months |
|
16 |
73 |
male |
yes |
house | none |
20 |
suspected colorectal cancer |
|
17 |
86 |
male |
no |
house | none |
19 |
bleeding from the rectum |
Referral for Colonoscopy
Overall, there were different ways in which patients could be referred for colonoscopy. However, the decision on whether the patient should be admitted to the hospital for bowel preparation was formally decided by a physician employed at the hospital, and no signs of nurses being involved in this decision were found. Sometimes the decision was made concerning the patient visiting the outpatient department and sometimes as an administrative decision, without seeing or talking to the patient.
Decision
The three hospitals had very different administrative guidelines for identifying patients who needed hospitalization for bowel preparation. One hospital’s guidelines stated that patients with severe renal insufficiency (creatinine clearance > 30 ml/min), congestive heart failure (NYHA III or IV), or needing help from healthcare professionals to go to the toilet must be admitted during bowel preparation. The second hospital only used general guidelines for being hospitalized, such as diabetes, heart disease, kidney disease, or disability. The third hospital had no guidelines and relied on an individual assessment by the admitting physician. In some cases, the possibility of hospital admission for bowel preparation was discussed with the patient and/or relatives, i.e., when the referral for colonoscopy was decided after a visit to the outpatient clinic or if a clear decision was stated in the referral from a family physician. The arguments for admitting patients included being nervous about undergoing bowel preparation at home, faecal incontinence, dizziness, difficulty walking, and insufficient help at home. In the guidelines for the two hospitals, only difficulty walking was mentioned as a recommendation for admission, but despite that, in all cases, the recommendations from the family physician were followed without question by both the nurse and admitting physician. Most often, when the hospital physician decided that a patient should be hospitalized for bowel preparation; the decision was primarily based on the physician’s subjective judgment, without talking to the patient or primary care or following guidelines (if there were any). Reasons such as suffering from a cognitive disability or a previously cancelled colonoscopy due to inadequate bowel preparation were not mentioned in the guidelines. Still, both nurses and physicians agreed that these patients should be admitted for bowel preparation without further dialogue with the patient. At one hospital, there was an administrative rule of thumb stating that there could be no more than two patients admitted for bowel cleansing at a time. This rule of thumb would therefore determine when a colonoscopy could take place.
Collaboration with Primary Care
The care offered by the six municipalities included in this study was very similar. However, there was considerable variation between municipalities’ rules for visitation for help with bowel preparation at home. Significantly, the notification deadline for the preparations varied. One municipality needed to be advised 24 hours before, while another municipality needed three days. At the administrative level, there was broad agreement from the nurses in primary care to follow their service catalogue, in which it was specified, which services they could offer a citizen who had to go through bowel preparation before a colonoscopy. The services the primary sector could offer included help to read and understand the instructions for bowel preparation, medication administration, help with toilet visits, change of diapers, change of bed linen, follow-up visits, phone calls to make sure the person was okay, and visitation based on an emergency call from the person. However, in practice, there were several challenges, such as planning the visits, which could make it difficult to help with toilet visits because it was unpredictable when the person needed to go to the toilet. Even if a person had an emergency call, some healthcare professionals expressed concerns since it could take a long time from the call until someone came for help. Optimally, the person should, to a certain extent, be able to control bowel movements and manage toilet visits relatively independently. Similarly, if the person needed help during the night, there would be a long waiting time, and the primary care nurse would need a key to the home. They also required that the person be cognitively well-preserved and follow the bowel preparation instructions.
Patients’ Experiences
Some patients were thankful that they were admitted to a hospital ward instead of undergoing bowel preparation at home. In addition, receiving the medication from the nurses at the precise hours contributed to a feeling of being taken care of and safe. The loss of control over bodily responses meant that they had to run to the toilet, and not knowing whether they would be able to hold back the faeces was highly stressful. Some patients felt embarrassed due to the lack of privacy in the hospital ward as they shared the toilet with another patient. They needed unrestricted access to the toilet, and the lack of privacy made them uncomfortable. Patients mentioned the importance of being well-informed. Some felt a lack of information but, even so, found it safer to be admitted than to undergo bowel preparation at home. On a few occasions, the patients went through bowel preparation, but their colonoscopy was cancelled due to miscommunication regarding their medication. For example, if the patient had not paused an anticoagulant drug or iron, the coloscopy could not be completed, and it had to be scheduled for weeks later. Consequently, the patients had to undergo bowel preparation once again. A situation that made the patients frustrated and angry. Generally, the patients feared managing the bowel preparation procedure at home because of their fear of making a mess.
Discussion
Our results indicate that nurses and primary care was not involved in the decision-making process whether a citizen could undergo bowel preparation at home with assistance from home care nurses or if hospital admission would be necessary. These results may contrast with the Danish healthcare systems’ vision of coherent care pathways across regions, municipalities, and the primary healthcare sector, intending to improve and coordinate tasks in close collaboration [12]. It also contrasts with the highly experienced nurses’ ability to include their assessment of the patient in clinical decision making. Our results also indicate that the services primary care could offer align with the care needs of most patients during hospitalization for bowel cleansing. This suggests that more patients might conduct bowel cleansing at home with the support of primary care. However, primary care faced challenges related to the time sensitivity of assisting patients. Considering the substantial number of patients hospitalized for bowel cleansing, it may be worthwhile to further explore involving primary healthcare professionals in the decision-making process, potentially leading to the development of new workflows. This approach may not only help patients feel confident about undergoing bowel cleansing at home but also avoid the costs associated with hospitalization. Moreover, it is worth noting that one of the patients in our study resided in a nursing home, which raises questions about the necessity of hospitalizing the patient for bowel cleansing. It may be reasonable to involve healthcare professionals from nursing homes in the decision-making to identify potential barriers in assisting patients during bowel cleansing. This collaborative effort could lead to development of workflow that eliminates the need for hospitalization in such cases.
Overall, we found no national guidelines describing which criteria should determine which patients should be hospitalized for bowel preparation before a colonoscopy. Furthermore, the practices at the three hospitals varied. Studies indicate that factors such as high age, male sex, low level of physical activity, lower educational level, several comorbidities, diabetes, chronic constipation, and polypharmacy are associated with inadequate bowel preparation [13-16]. However, none of these factors was reflected in the hospitals’ local guidelines. Although comprehensive European guidelines underline the importance of sufficient bowel preparation for a successful colonoscopy [8], it has not been possible to clarify recommendations identifying factors that determine whether a patient should be hospitalized for bowel preparation or undergo bowel preparation at home. Another study also found that several patients were referred directly to colonoscopy without being in contact with the hospital. These patients participated in screening programs, follow-up on colon cancer screening tests, and surveillance colonoscopy. This may be problematic, as many patients undergo colonoscopy unnecessarily because no physician has engaged in a conversation with the patients regarding the indications and risks of the procedure or the reason why some patients decide not to show up for the colonoscopy [17]. A recent study found that patients’ decision on whether to undergo a colonoscopy was characterized by uncertainty about what to expect [18]. Shared decision-making has been found to improve patients’ feelings of being well-informed [19] and to improve patients’ attentiveness and adherence to recommendations [20]. Thereby, whether shared decision-making is a tool to reduce the number of inadequate bowel preparations should be discussed. We found no studies investigating shared decision-making concerning patients referred to colonoscopy, but shared decision-making is recommended in other gastroenterological settings such as general screening for colon cancer [21,22]. Several factors have been related to the adequacy of bowel preparation, and inpatient status represents one of the strongest independent predictors of inadequate colon cleansing. Inadequate inpatient bowel preparation may increase the length of hospital stay by about 25% and costs by 30% compared to adequate preparation [14]. Ideally, patients understand and are well prepared for the procedure, which requires dialogue between patients and healthcare professionals [17]. However, some patients miss pieces of information [18]. The completion of bowel preparation is incredibly challenging for older patients, and a low score of ADL has been found to be a significant predictor of inadequate bowel preparation [23]. However, in our study, the patients had a high Barthel score, indicating a high level of physical functional performance. This indicate that no formal assessment of patients’ physical status are included in the decision of whether a patient should be hospitalized. Furthermore, undergoing bowel cleansing is a stressful procedure, unfamiliar to most patients. Therefore, relying solely on scores such Barthel may not provide an accurate assessment of patients’ ability to independently manage bowel cleansing at home. In our study, other factors, such as psychological aspects or previous experiences of inadequate bowel cleansing, influenced the decision for hospitalization.
Hospitalization for bowel preparation is associated with an almost two-fold higher risk of inadequate bowel preparation before colonoscopy. This may be associated with the fact that inpatients have more comorbidities than patients undergoing bowel preparation at home. Likewise, it may be associated with nurses’ and physicians’ need for specific education in bowel preparation [24-26]. Interventions, such as videos or phone calls the day before the colonoscopy, have been explored, but the optimal solution has still not been found [27].
The findings in this study might not be transferrable to settings outside Denmark, even though the high number of patients not sufficiently prepared for colonoscopy is well known in many countries. In addition, there are factors influencing the decision for hospitalization that have not been considered in this study, including the economic constraints of the healthcare system, the lack of nurses influencing the number of beds available, the need for further improvement of the medication used for bowel preparation, and screening the level of patients’ constipation before a decision on admission. This will probably also affect the future administrative procedures of patient care. Moreover, we did not explore the perspectives of the relatives, which could have provided insight into the feasibility and appropriateness of asking close relatives to support their family member during bowel cleansing. Such insight could have shed light on the role of the relatives in this context.
Conclusion
Different variables included in the decision to hospitalize patients for bowel preparation were identified. The lack of evidence-informed decision-making, the involvement of patients in decision-making, and the missing collaboration across healthcare sectors are possible essential factors to include in developing better care trajectories.
Acknowledgment
We wish to thank the patients, nurses, and physicians participating in this study for taking the time to talk to us.
Funding
This research did not receive any specific grant from funding agencies
References
- Kastenberg D, Bertiger G, Brogadir S (2018) Bowel preparation quality scales for colonoscopy. World J Gastroenterol 24: 2833-2843. [crossref]
- Kim SY, Kim HS, Park HJ (2019) Adverse events related to colonoscopy: Global trends and future challenges. World J Gastroenterol 25: 190-204. [crossref]
- Petersen MM, Ferm L, Kleif J, Piper TB, Rømer E, et al. (2020) Triage May Improve Selection to Colonoscopy and Reduce the Number of Unnecessary Colonoscopies. Cancers (Basel) 12. [crossref]
- Parra-Blanco A, Ruiz A, Alvarez-Lobos M, Amorós A, Gana JC, et al. (2014) Achieving the best bowel preparation for colonoscopy. World J Gastroenterol 20(47): 17709-26. [crossref]
- Alvarez-Gonzalez MA, Pantaleon MA, Flores-Le Roux JA, Zaffalon D, Amorós J, et al. (2019) Randomized Clinical Trial: A Normocaloric Low-Fiber Diet the Day Before Colonoscopy Is the Most Effective Approach to Bowel Preparation in Colorectal Cancer Screening Colonoscopy. Diseases of the Colon and Rectum 62: 491-497. [crossref]
- Shamim S, Andresen YLM, Vind Thaysen H, Hovdenak Jakobsen I, Nielsen J, et al. (2021) Experiences of Patients Undergoing Bowel Preparation and Colonoscopy: A Qualitative Longitudinal Study. Journal of Multidisciplinary Healthcare.14: 349-358. [crossref]
- Ryhlander J, Ringstrom G, Simrén M, Stotzer PO, Jakobsson S (2019) Undergoing repeated colonoscopies – experiences from patients with inflammatory bowel disease. Scandinavian Journal of Gastroenterology 54: 1467-1472.
- Hassan C, East J, Radaelli F, Spada C, Benamouzig R, et al. (2019) Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2019. Endoscopy 51: 775-794. [crossref]
- Almadi MA, Alharbi O, Azzam N, Altayeb M, Thaniah S, et al. (2018) Bowel preparation quality between hospitalized patients and outpatient colonoscopies. Saudi Journal of Gastroenterology: Official Journal of the Saudi Gastroenterology Association 24: 93-99. [crossref]
- Currie DJ, Smith C, Jagals P (2018) The application of system dynamics modelling to environmental health decision-making and policy – a scoping review. BMC Public Health.18. [crossref]
- Collin C, Wade DT, Davies S, Horne V (1988) The Barthel ADL Index: A reliability study. International Disability Studies.10: 61-63. [crossref]
- Sundhedsministeriet (2017) Udvalg om det nære og sammenhængende sundhedsvæsen.
- Tontini GE, Prada A, Sferrazza S, Ciprandi G, Vecchi M (2021) The unmet needs for identifying the ideal bowel preparation. JGH Open: An Open Access Journal of Gastroenterology and Hepatology 5: 1135-1141. [crossref]
- Fuccio L, Frazzoni L, Spada C, Mussetto A, Fabbri C, et al. (2021) Factors That Affect Adequacy of Colon Cleansing for Colonoscopy in Hospitalized Patients. Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association 19. [crossref]
- Kim HG (2016) Is Elderly Age a Simple Predictive Factor for Inadequate Bowel Preparation before Colonoscopy? Gut and Liver 10: 489-490. [crossref]
- Neilson LJ, Thirugnanasothy S, Rees CJ (2018) Colonoscopy in the very elderly. British Medical Bulletin 127: 33-41. [crossref]
- Restall G, Walker JR, Waldman C, Zawaly K, Michaud V, et al. (2018) Perspectives of primary care providers and endoscopists about current practices, facilitators and barriers for preparation and follow-up of colonoscopy procedures: a qualitative study. BMC Health Services Research 18. [crossref]
- Rosvall A, Axelsson M, Toth E, Kumlien C, Annersten Gershater M (2021) Patients’ Experiences Before, During, and After a Colonoscopy Procedure: A Qualitative Study. Gastroenterology Nursing: The Official Journal of the Society of Gastroenterology Nurses and Associates 44: 392-402. [crossref]
- Pieterse AH, Finset A (2019) Shared decision making—Much studied, much still unknown. Patient Education and Counseling 102(11): 1946-1948. [crossref]
- Amir N, McCarthy HJ, Tong A (2021) A working partnership: A review of shared decision-making in nephrology. Nephrology (Carlton, Vic) 26: 851-857. [crossref]
- Hadjiliadis D, Khoruts A, Zauber AG, Hempstead SE, Maisonneuve P, Lowenfels AB (2018) Cystic Fibrosis Colorectal Cancer Screening Consensus Recommendations. Gastroenterology 154: 736-745. [crossref]
- Nee J, Chippendale RZ, Feuerstein JD (2020) Screening for Colon Cancer in Older Adults: Risks, Benefits, and When to Stop. Mayo Clinic Proceedings 95: 184-196. [crossref]
- Kumar A, Lin L, Bernheim O, Bagiella E, Jandorf L, et al. (2016) Effect of Functional Status on the Quality of Bowel Preparation in Elderly Patients Undergoing Screening and Surveillance Colonoscopy. Gut and Liver 10: 569-573. [crossref]
- Chambers K, Whiteman K, Stephens K, Goodloe L, Kirsteen H (2016) Improving Inpatient Colonoscopy Preparation in a University Hospital: An Evidence-Based Practice Project. Gastroenterology Nursing: The Official Journal of the Society of Gastroenterology Nurses and Associates 39: 86-94. [crossref]
- Lee YJ, Kim ES, Park KS, Cho KB, Jang BK, et al. (2015) Education for Ward Nurses Influences the Quality of Inpatient’s Bowel Preparation for Colonoscopy. Medicine 94. [crossref]
- Shah-Khan SM, Cumberledge J, Reynolds GJ (2017) Using the plan-do-study-act approach to improve inpatient colonoscopy preparation. BMJ Open Quality 6. [crossref]
- Gkolfakis P, Tziatzios G, Papanikolaou IS, Triantafyllou K (2019) Strategies to Improve Inpatients’ Quality of Bowel Preparation for Colonoscopy: A Systematic Review and Meta-Analysis. Gastroenterology Research and Practice 2.