Abstract
Myofascial release (MFR) is a technique for resolving fascial restriction; i.e., the fascia trapped with moderate pressure is continuously expanded to expand collagen fibers as well as fascial elastin fibers. In recent years fascia has increasingly been studied, as the roles and importance of fascia have become apparent. In many case reports pain and postural alignment have been designated as the outcome, and changes before and after MFR have been observed. Controlled studies have included a variety of researches for the presence or absence of the effects of MFR on patients with certain diseases, comparison of MFR with other techniques, and basic studies on the effects of MFR in healthy persons. It has been believed, however, that systematic reviews are of various quality levels because of the obscure content of intervention and insufficient exclusion of bias in spite of the favorable effects and the moderate quality of MFR techniques. The future task confronting us is thought to accumulate controlled studies, which will allow acquiring definite blinding and distinctly explaining fascial changes by detailed intervention methods.
Introduction
Myofascial release (MFR) is a technique for relieving fascial restriction; i.e., the fascia trapped with moderate pressure is expanded continuously, by which collagen fibers, as well as fascial elastin fibers, are expanded. Since MFR yields no any pain to the person treated by MFR without use of any specific tool, it can be used for every disease over all age groups; i.e., it is available for acute/chronic pain, restricted range of motion (ROM), conditioning in children and the aged, sports injury, and so on [1]. Some investigators have reported the origin of MFR. MFR is a fruit of soft tissue mobilization according to an American physical therapist, John F. Barnes [2], one of the Structural Integration (Rolfing®) techniques developed by an American biochemist, Ida P. Rolf [3], and a product of the technique developed by Thomas W. Myers [4], the author of “Anatomy Train”, who directly received training from Ida P. Rolf.
In recent years the roles and importance of fascia have become apparent, and at the same time fascia is being increasingly studied. Despite that MFR exerts the effects non-invasively on fascia via the superficial skin and fat layer, many MFR researches have designated changes in physical function, including changes in alignment and ROM, as the outcome. For this reason, the questions of whether fascia can be actually found or not and of how fascia changes remained. In recent years, however, imaging-out of fascia by an ultrasound imaging diagnostic device and observation of changes in the properties of fascia have become possible. This article introduces some previous researches for MFR with the author’s case reports. Self-MFR and foam roller MFR are excluded from the present study.
Previous Researches
Case reports
Barnes has reported treatment of a 35-year-old female patient who has suffered from thoracic outlet syndrome for 2 years. The 30-minute treatment including expansion of her upper limbs and MFR of the iliac muscle was conducted twice to three times a day for 2 weeks. Her pain was reduced, swing of her upper limbs during walking was normalized, kyphosis was improved, her body trunk and pelvis were restored to a median position, and the right-to-left load became even [5]. Le Bauer et al. have reported treatment of an 18-year-old female patient, who has suffered from bimodal scoliosis for 6 years. The 60-minute treatment including MFR involving her body trunk and expansion of her both lower limbs was conducted twice a day for 2 weeks. Postural alignment, X-ray images, pain, the condition with scale 22 based on the Scoliosis Research Society, and ROM of thoracolumbar rotation were markedly improved [6].
Martin has reported treatment of a female patient with diffuse systemic sclerosis. The treatment included 11 sessions of MFR involving the head and neck and 9 sessions of MFR involving her body trunk, and it took 60 minutes for each session. The treatment was conducted for 5 months, and symptoms of Raynaud’s phenomenon, thoracic mobility, and orificial distance were improved [7]. Walton has reported treatment of a 35-year-old female patient with primary Raynaud’s phenomenon. The 45-minute treatment including MFR of the region ranging from the neck to the dorsal surface of the chest and expansion of her upper limbs was conducted for 3 weeks. The duration and frequency of the appearance of Raynaud’s phenomenon and the severity of pain were decreased [8]. Many case reports have designated pain and postural alignment as the outcome and observed changes before and after MFR.
Controlled studies
Barnes et al. have divided 10 orthopedic outpatients into an MFR group of 6 patients who were treated with MFR [of the quadriceps muscle of thigh (QMT), iliopsoas muscle, and the contralateral iliopsoas muscle] for 10 minutes and a control group of 4 patients who were subjected only to lie on a bed for 10 minutes, and compared both groups concerning lateral tilt angle of the pelvis [the mean difference in the distance between the right and left anterior superior iliac spine (ASIS) and the central point at patient’s feet]. The difference in the distance was significantly reduced in MFR group, increasingly showing the symmetric form of the pelvis [9]. Takeda et al. have conducted MFR of the greater pectoral muscle and smaller pectoral muscle in 25 patients with retentive hemiplegia, and compared the angle of abduction of the shoulder on the affected side, speed and the degree of easiness of patients’ daily living lives, and 10-meter walking speed before and after MFR. They have reported the significant improvement in the abduction angle and the speed of the patients’ daily living lives [10]. Marszaiek has conducted MFR of the head, neck, upper limbs, and the upper body trunk in 40 patients who have undergone total laryngectomy. The esophageal pressure was significantly decreased after MFR, having led to easy training of esophageal phonation [11]. Some other reports have shown that MFR of the head and neck in patients with the forward head posture has induced the significant improvement in the craniospinal angle, neck disability index, and cervical ROM [12, 13] and that MFR of the body trunk involving the low back in low back pain patients has induced significant improvement in pain and the influence of low back pain on daily living activities [14–16].
Kain et al. have compared each ROM of flexion, extension, and abduction of the shoulder between an MFR group of 18 healthy subjects who underwent precordial MFR for 3 minutes and a hot pack group of 13 healthy subjects who underwent hot pack for 20 minutes. Both groups showed significantly increased ROM, compared to that before the implementation, except that only the flexion angle was significantly higher in the MFR group than in the hot pack group [17]. Henley et al. have compared heart rate on a tilt (50°) table, normalized ECG, and respiration rate between an MFR group of 17 healthy subjects who underwent MFR of the neck for 2 minutes and a pseudo-MFR group of 17 healthy subjects with their neck only touched by rater’s hands. Tachycardiac rate and normalized ECG were significantly increased in both groups, compared to those at rest, whereas the tachycardiac rate and the normalized ECG were lower in the MFR group than in the pseudo-MFR group [18].
Kuruma et al. have compared ROM of knee joint flexion, muscle stiffness, and reaction time among a QMT-MFR group of 10 healthy subjects who underwent MFR of the QMT for 8 minutes, a hamstrings (H)-MFR group of 10 healthy subjects who underwent MFR of H for 8 minutes, and a stretching group of 10 healthy subjects who underwent stretching of QMT. All groups significantly showed improvement in ROM, while reaction time was significantly reduced in the QMT-MFR and H-MFR groups [19]. Ichikawa et al. have compared muscle stiffness and the fascial transmission distance on ultrasonic images among an MFR group of 12 healthy subjects who underwent MFR of the lateral great muscle for 4 minutes, 10-min-hot-pack group of 12 healthy subjects who underwent hot pack for 10 minutes, and 20-min-hot-pack group of12 healthy subjects who underwent hot pack for 20 minutes. There were significant changes in muscle stiffness and the fascial transmission distance only in the MFR group [20].
We have compared angles of active and passive extension and elevation of lower limbs and muscle strength (extension/flexion of the knee joint) before intervention and for 6 days after intervention among an H-MFR group of 10 healthy subjects who underwent MFR of hamstrings (H), a QMT (re-education)-MFR group of 10 healthy subjects who underwent muscle re-education exercises of QMT (40 times at muscle strength of 40% of 1 repetition maximum) following MFR of H, and an H (re-education)-MFR group of 10 healthy subjects who underwent muscle re-education exercises of H following MFR of H. Improvements in the extension and elevation angles for the lower limbs and the muscle strength of knee flexion were much more in the H (re-education)-MFR group than in two other groups. There were also significant differences between those 6 days after and before the implementation. In the H-MFR group there were significant differences in the angle of extension and elevation of lower limbs and muscle strength of knee flexion between those for 4 days after and before MFR [21]. To investigate the fascial properties after MFR, we clarified intra-rater reliabilities [ICC (1, 1)] 4 days after measurements of superficial and deep fascial transmission distances on ultrasound images of lateral head of the gastrocnemius muscle by using an ultrasound imaging diagnostic device and measurement of muscle stiffness according to real-time tissue elastographic function (superficial layer: 0.89; deep layer: 0.98; muscle stiffness: 0.90) [22]. We compared ROM of ankle dorsal flexion, muscle strength of ankle plantar flexion, fascial transmission distance, and muscle stiffness before and after intervention and for 4 days after intervention between an MFR group of 17 healthy subjects who underwent MFR of the lateral head of gastrocnemius muscle for 3 minutes and a stretching group of 17 healthy subjects who underwent static stretching for 3 minutes. In both groups, ROM and fascial transmission distance were increased and muscle stiffness was decreased immediately after the intervention, compared to those before intervention. Immediately after the intervention muscle strength was increased in the MFR group and decreased in the stretching group, while ROM, muscle strength, and fascial transmission distance were increased and muscle stiffness was decreased 4 days after the intervention than those before the intervention only in the MFR group [23]. Thus, there have been a variety of controlled studies including comparative studies on the presence/absence of the effects of MFR on patients with certain diseases and between MFR and other techniques, as well as basic researches of the effects of MFR on healthy persons.
Systematic reviews
Yang et al. [24] have inspected 1329 references in the literature concerning chest physiotherapy for pneumonia in adults in 2010, which included 6 references of randomized controlled trials (434 subjects). As a result, it was revealed that osteopathic therapy including MFR allowed admission period and the duration required for intravascular and systemic antibiotic treatment having been decreased, although any symptom of pneumonia or X-ray finding was not improved [22]. Yuan et al. have investigated minutely 532 references in the literature concerning treatment for fibromyalgia in 2015, and 2 references about randomized trials of MFR (145 subjects) were included in meta-analysis. As a result, it was revealed that MFR had moderate evidence of its effects particularly on pain, anxiety, and depression [25]. McKenney et al. have examined closely 88 references in the literature to investigate the quality and reliability of MFR in 2013, and 10 references of randomized trials were included. Ajimsha et al. have also investigated 3 systematic reviews in 2019. The thus-described researchers’ studies have provided evidence of the favorable effects of MFR and the moderately technical quality, but according to them, it has various degrees of quality for the reason that the intervention contents are obscure and that bias is insufficiently removed. They have brought their researches to a conclusion by saying that individual systematic review will become a beginning toward future investigation of higher quality [26, 27].
Case reports
The author encountered 2 patients who acquired characteristic improvement as a result of MFR. These cases are introduced below. The first case was a male patient in his 50s, a physician, whose chief complaint was low back pain. When he tried to stand up after morning medical examination, he could not stand up because of low back pain. As for sites of low back pain, he had both lumbar regions, but the pain was particularly severe in the right region. He had no idea of any event by which low back pain was manifested in his recent daily activities. According to inquiries about his past history, he had right second metatarsal capital fracture 6 months ago. He has been unable to bear any load on the affected site and shown claudication because of pain for a while. At present, he had no pain in the right second metatarsal bone. He felt low back pain in getting-up and standing positions and during walking. Since he had pain when load was given to the affected site, evaluation was started with his feet on the assumption that the right second metatarsal capital fracture was responsible for low back pain. Subsequently, high-density regions were recognized in the right long extensor muscle of great toe, right anterior tibial muscle, lateral head of the right gastrocnemius muscle, right biceps muscle of thigh, right iliac muscle, bilateral lumbar iliocostal muscle, and bilateral lumbar quadrate muscles. Except for the lumbar quadrate muscles, it was considered that claudication to avoid using the second metatarsal bone resulted in the condition in which fascial dysfunction has spread along the anterior and posterior motion arrangement (referred to the concept of fascia and fascial approach) (Figure 1). Faced with this situation, we considered the feet as the cause of the condition, and we conducted MFR on each of the right long extensor muscle of great toe, right anterior tibial muscle, and lateral head of the right gastrocnemius muscle for 3 minutes. After MFR, low back pain was reduced from score 8 to score 3 based on the Numerical Rating Scale. When MFR was conducted on each of the bilateral lumbar iliocostal muscles for 2 minutes, low back pain disappeared and he felt no physical disorder at his low back. His subsequent course also appeared favorable.
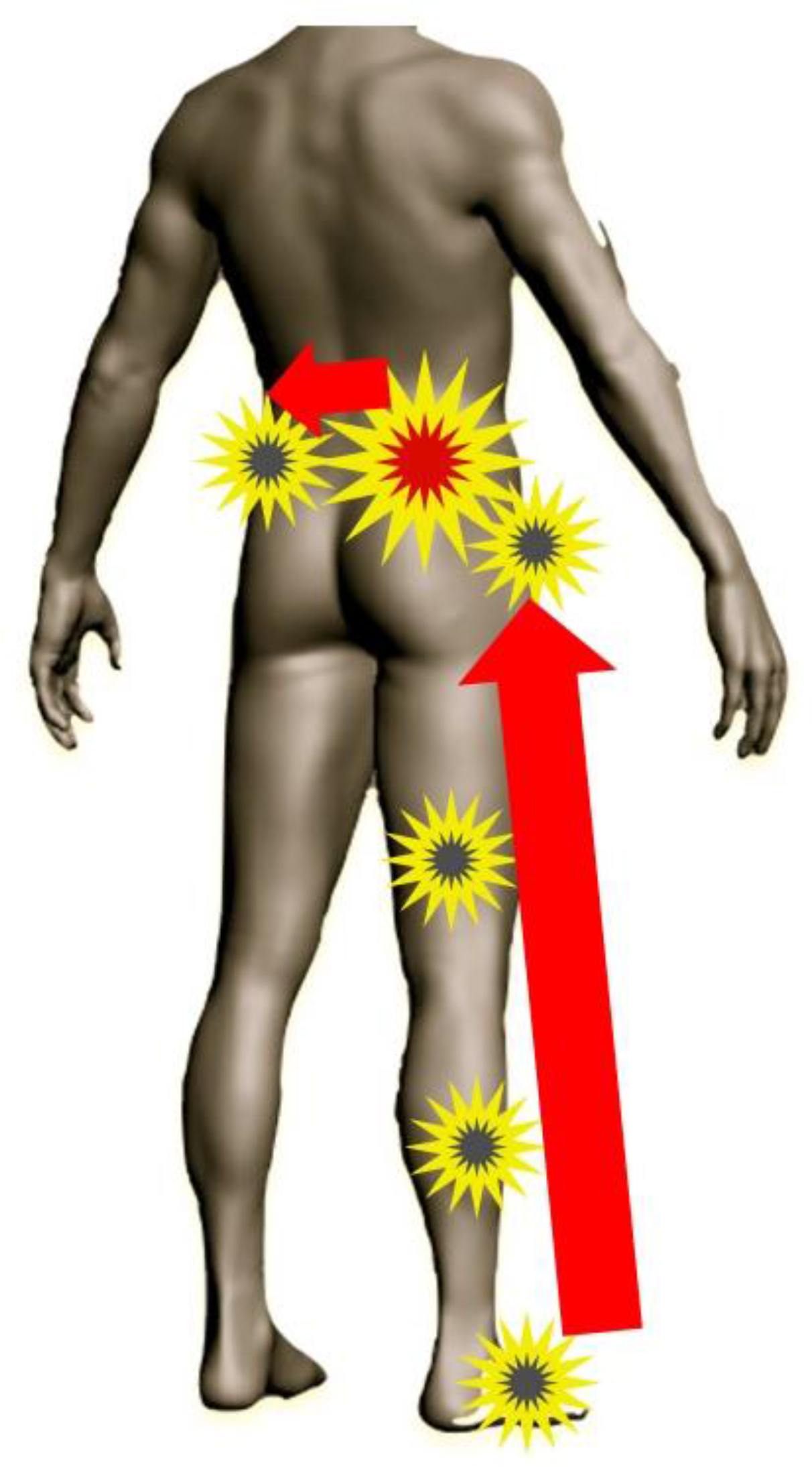
Figure 1. Fascia showing the ascending spread of high-density areas.
The second case was a male patient in his 80s, and diagnosed as having had left middle cerebral arteriosclerosis. Owing to (rt-PA) thrombolysis, paralysis was improved from complete paralysis to moderate right hemiplegia. It was improved even to mild paralysis by 3-week rehabilitation, and he acquired retentive self-supporting in a standing position and walking without support with light assistance. However, improvement of function of swallowing was worse than that of physical function. It was assumed from postural evaluation that anterior cephalic presentation and unbalance between the right and left postural alignments (effortive on the non-affected side) inhibited movements of the masticatory muscle and muscles of tongue. On this assumption, MFR of the suboccipital muscles, left sternocleidomastoid muscle, suprahyoid muscles, posterior region of neck, and upper fibers of left trapezius muscle, and expansion of the left upper limb were conducted for 40 minutes a day for 3 days. As a result, the anterior cephalic presentation was improved (Figure 2), the right and left postural alignments showed symmetric balance (Figure 3), and the swallowing function was also improved (Table 1).
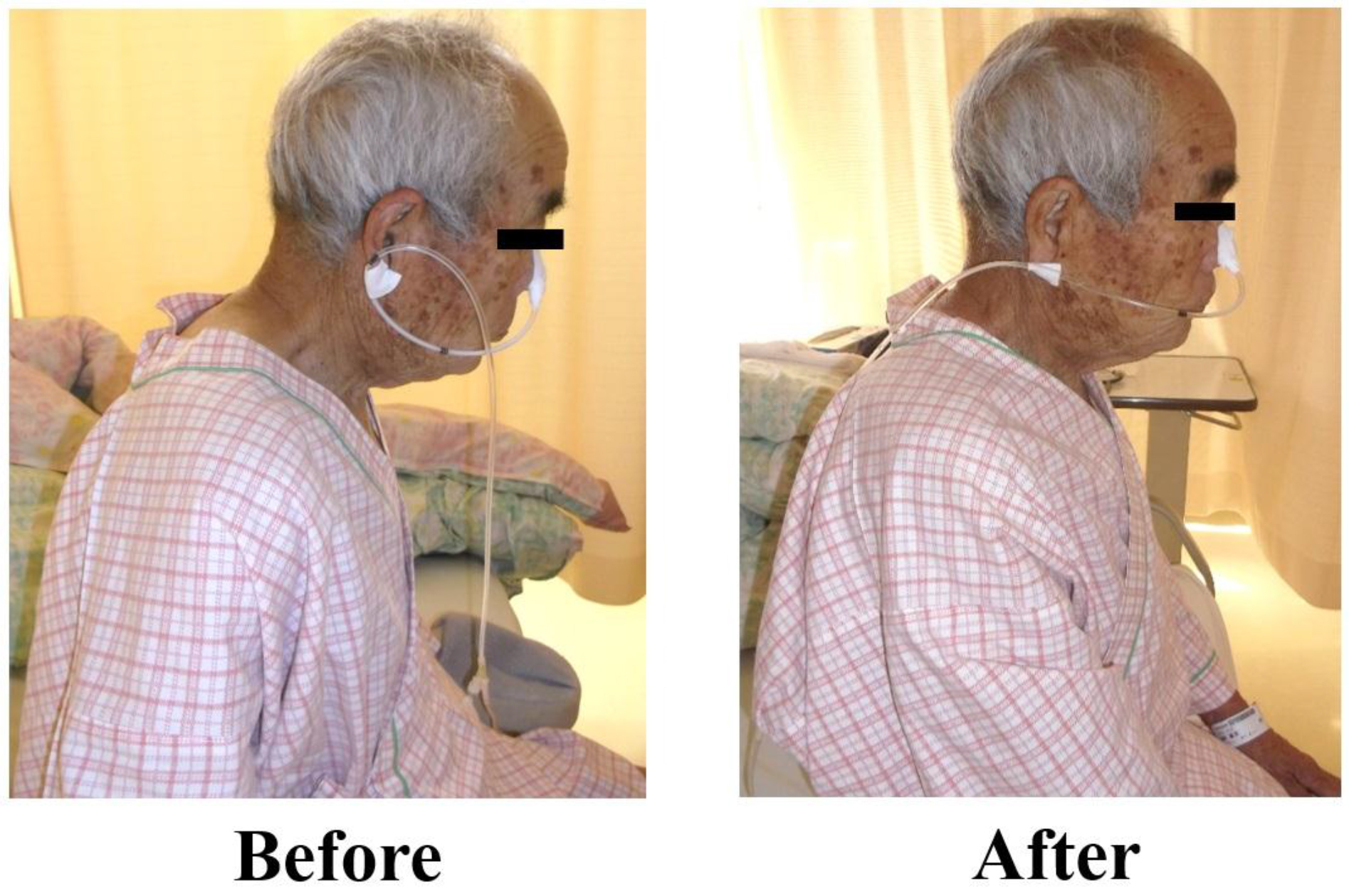
Figure 2. Postural alignment on the sagittal plane (rightward motion) before and after the treatment.

Figure 3. Postural alignment on the frontal plane (ante-motion) before and after the treatment.
Table 1. Evaluation of the swallowing function before and after the treatment.
|
|
Before intervention |
After intervention |
|
Swallowing |
Swallowed after several times |
Swallowed after once or twice |
|
The amount ingested |
1/3 spoonful |
a spoonful |
|
Pharyngeal residue |
(+) |
(±) |
|
Cough |
(+) immediately after meals |
(+) after some mouthfuls |
|
Tongue protrusion |
(-) |
(+) |
Conclusion
Establishment of evidence of the effects of MFR seems to be delayed, while approach to fascia is increasingly spreading along with the increasing recognized importance of fascia. The future task confronting us is thought to accumulate controlled studies, which will allow distinctly explaining fascial changes under the condition of definite blinding by detailed intervention methods.
References
- Takei H (2001) Myofascial Release. Rigakuryoho Kagaku. Apr: 103–107 (Japanese).
- Barnes JF (1990) How It Bagan Myofascial Release the search for excellence. Washington, USA: National Library of Medicine Pg No: 1–2.
- Yasushi F (2005) An Outline of Rolfing. Japanese Journal of Complementary and Alternative Medicine. Feb: 37–43(Japanese).
- Earls J, Myers TW (2010) An Introduction to Fascial Release Technique Fascial Release for Structural Balance Chichester, UKB: Lotus Publishing Pg No: 4–16.
- Barnes JF (1996) Myofascial release in treatment of thoracic outlet syndrome. J Bodyw Mov Ther Jan: 53–57.
- LeBauer A, Brtalik R, Stowe K (2008) The effect of myofascial release (MFR) on an adult with idiopathic scoliosis. J Bodyw Mov Ther 12: 356–363. [crossref]
- Martin MM (2008) Effects of the myofascial release in diffuse systemic sclerosis. J Bodyw Mov Ther Apr: 1–9.
- Walton A (2008) Efficacy of myofascial release techniques in the treatment of primary Raynaud’s phenomenon. J Bodyw Mov Ther Pg No: 274–280.
- Barnes MF, Gronlund RT, Little MF, Personius WJ (1997) J Bodyw Mov Ther. Oct: 289–296.
- Takeda S, Takahashi K, Kawasaki T, Kaneko T, et al. (2005) Ijikinouso cchuukatamahi kanja Mahisoku kyoubukingunn henokinnmakuriri- sunoouyou [abstract] Rigakuryouhougaku 32(Suppl 2): ID-868 (Japanese).
- Marszaiek S (2009) Estimation of influence of myofascial release techniques on esophageal pressure in patients after total laryngectomy. Eur Arch Otorhinolaryngol May: 1305–1308.
- Kim J, Kim S, Shim J, Kim H (2018) Effects of McKenzie exercise, Kinesio taping, and myofascial release on the forward head posture. J Phys Ther Sci Pg No: 1103–1107.
- Aggarwal A, Shete AV, Palekar TJ (2018) Efficacy of Suboccipital and Sternocleidomastoid Release Technique in Forward Head Posture Patients With Neck Pain: A Randomized Control Trial. Int J Physiother Pg No: 149–155.
- Tozzi P1, Bongiorno D, Vitturini C (2011) Fascial release effects on patients with non-specific cervical or lumbar pain. J Bodyw Mov Ther 15: 405–416. [crossref]
- Ajimsha MS, Daniel B, Chithra S (2014) Effectiveness of myofascial release in the management of chronic low back pain in nursing professionals. J Bodyw Mov Ther 273–281.
- Arguisuelas MD, Lison JF, Domenech-Fernandez J, Martinez-Hurtado I (2019) Effects of myofascial release in erector spinae myoelectric activity and lumbar spine kinematics in non-specific chronic low back pain: Randomized controlled trial. Clin Biomech (Bristol, Avon) 27–33.
- Kain J, Martorello L, Swanson E, Sego S (2010) Comparison of an indirect tri-planar myofascial release (MFR) technique and a hot pack for increasing range of motion. J Bodyw Mov Ther 63–67.
- Henley CE, Ivins D, Mills M, Wen FK, et al. (2008) Osteopathic manipulative treatment and its relationship to autonomic nervous system activity as demonstrated by heart rate variability a repeated measures study. Osteopath Med Prim Care 2–7.
- Kuruma H, Takei H, Nitta O, Furukawa Y, et al. (2006) Kinmakuriri-su to sutorecchingu womochiita rigakuryouho ukouka no hikakukentou [abstract] Rigakuryouhougaku 2006; 34 (Suppl 2) ID-259 (Japanese).
- Ichikawa K, Takei H, Usa H, Mitomo S, et al. (2015) Comparative analysis of ultrasound changes in the vastus lateralis muscle following myofascial release and thermotherapy: a pilot study. J Bodyw Mov Ther 327–336.
- Katsumata Y, Takei H, Hori T, Hayashi H (2016) Influences of muscle re-education exercises for myofascial extensibility and muscle strength after myofascial release. Rigakuryoho Kagaku 99–106.
- Katsumata Y, Takei H, Hayashi H, Ichikawa K (2017) Intra- and Inter-rater Reliabilities of measurements of fascial displacement and muscle stiffness by using ultrasound images. Rigakuryoho Kagaku 215–220 (Japanese).
- Katsumata Y, Takei H, Sasaki Y, Watanabe K (2019) Ultrasonographic changes in fascial properties over time after myofascial release. Integr J Orthop Traumato 1–6.
- Yang M, Yuping Y, Yin X, Wang BY, et al. (2010) Chest physiotherapy for pneumonia in adults. Cochrane Database Syst Rev CD006338.
- Yuan SL, Matsutani LA, Marques AP (2015) Effectiveness of different styles of massage therapy in fibromyalgia: a systematic review and meta-analysis. Man Ther 257–264.
- McKenney K, Elder AS, Elder C, Hutchins A (2013) Myofascial release as a treatment for orthopaedic conditions: a systematic review. J Athl Train 522–527.
- Ajimsha MS, Shenoy PD (2019) Improving the quality of myofascial release research – A critical appraisal of systematic reviews. J Bodyw Mov Ther 561–567.