Abstract
Objective: To explore the effects of COVID-19 on urolithiasis management and on the medical practice of urologists in Gulf countries.
Methods: A web-based survey was sent to urologists in the six countries in the Gulf Cooperation Council (GCC). The survey consisted of 23 questions about their working environment, urolithiasis management experience, and the policies of their facilities during the COVID-19 pandemic.
Results: During the one-week survey period, responses were received from 191 urologists working in the six GCC countries. Responses were received from urologists in all six countries but the numbers differed markedly. Of the 191 urologists who responded, 160 (83.8%) were experienced urologists and 31 (16.2%) were urology residents. Eighty-four (44.0%) volunteered for COVID-19 management rather than urology, 22 (11.5%) were infected with COVID-19 and 38 (19.9%) sought mental health support. Clinical duties related to urolithiasis management were reduced for most of the urologists, with elective procedures postponed and urolithiasis management confined to emergency conditions. In the absence of COVID-19 infection, 67 (35.1%) preferred to actively manage ureteral stones, whereas the remaining urologists preferred less invasive methods, such as conservative or instant drainage.
Conclusion: COVID-19 is hazardous to urologists in GCC countries, with 11.5% being infected and most reducing their clinical duties related to urolithiasis management. Although urolithiasis management in GCC countries during the COVID-19 pandemic was generally consistent with worldwide guidelines, some differences were observed, with further studies warranted to compare different management strategies.
Introduction
COVID-19 is a species of coronavirus that causes severe acute respiratory syndrome (SARS-COV-2) [1]. The first documented cases were in Wuhan, China, in September 2019. Infection subsequently spread worldwide, with the World Health Organization announcing an epidemic in March 2020 [2]. Since then, all countries worldwide have started to lockdown, with many activities being restricted, including flying, attending schools, participating in and watching sports activities, shopping at malls, and public gatherings. The health system has also been affected, with elective procedures and clinics being restricted. These restrictions have affected urologic practice and patient management [3]. Although the populations of the six countries in the Gulf Cooperation Council (GCC) have similar demographic characteristics, each country has devised its own lockdown strategy to deal with the pandemic. The present study explored the effects of the pandemic on the management of urolithiasis patients across the Gulf countries, as well as the impact of the pandemic on urologists practicing in these countries.
Methodology
A web-based survey was developed by a group of urologists from the six GCC countries. The survey, written in English, included 23 general and specific questions about COVID-19, including ten questions with free-response prompts. Upon developing the survey, it was sent to another few urologists as a pilot for validation.
The survey was sent to many urologists in the GCC countries who were easily approachable by the study investigators during the week of 10-16 May 2020. The 23 questions on the survey are detailed in Figure 1.
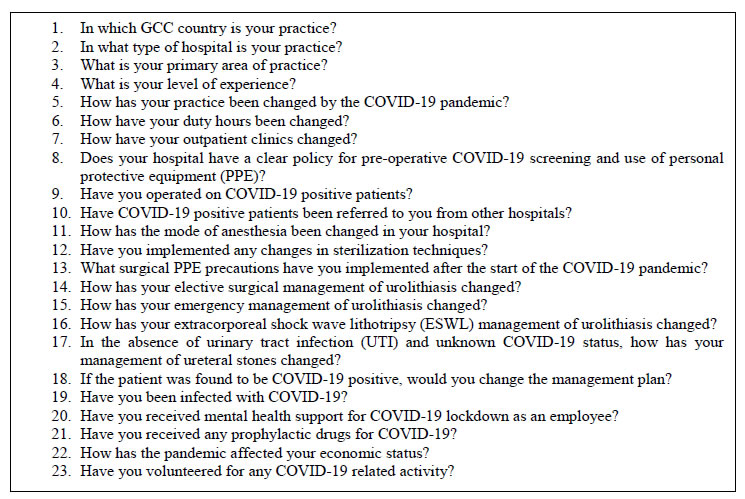
Figure 1. Questions of the survey.
Results
Responses were received from 191 urologists, representing the six GCC countries. Of these respondents, 72 (37.7%) were from Qatar, 39 (20.4%) from Kuwait, 30 (15.7%) from the United Arab Emirates (UAE), 19 (9.9%) each from Oman and the Kingdom of Saudi Arabia, and 12 (6.3%) from Bahrain (Figure 2).
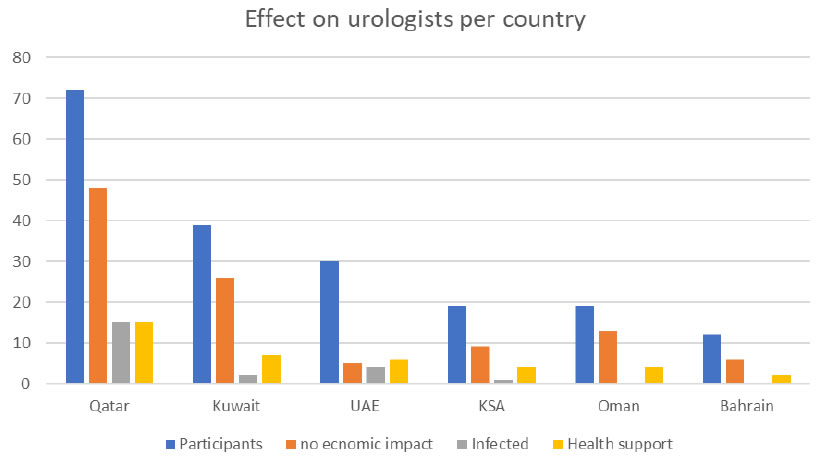
Figure 2. The effect of COVID-19 on urologists in each country.
Of the 191 urologists, 145 (75.6%) worked in governmental hospitals, including 27 (14.1%) at academic centers, and 46 (24.4%) worked in private practice. The respondents differed in working experience, with 82 (42.9%) being consultants, 54 (28.3%) being specialists, nine (4.7%) being senior registrars, ten (5.2%) being registrars, four (2.1%) being assistant registrars, and 31 (16.2%) being urology residents. Of the respondents, 124 (64.9%) were general urologists, 42 (22.0%) were endo-urologists, and 25 (13.1%) were primarily interested in subspecialties in addition to urolithiasis.
Interestingly, 128 (67%) respondents changed their regular urology practice in response to COVID-19, 48 (25.1%) continued their routine practice, and 15 (7.9%) stopped practicing medicine following the lockdown. The lockdown reduced duty hours for 118 (61.8%) of the respondents and increased duty hours for 22 (11.5%), whereas 49 (25.7%) had almost the same number of duty hours, and two (1.0%) stopped practicing medicine.
Outpatient clinics and elective surgeries were closed or limited to minimize contact with patients. Only 26 (13.6%) reported no changes in the management of their clinics, whereas 37 (19.4%) closed their clinics, 91 (47.6%) changed to telemedicine phone consultations, four (2.1%) are consulting by video conference, and one (0.5%) is communicating with patients through the facility website.
Of the 191 respondents, 118 (61.8%) are not operating on patients infected with COVID-19, and 139 (72.8%) have stopped performing elective urolithiasis procedures. In contrast, 44 (23%) have reduced the number of elective urolithiasis procedures, whereas eight (4.2%) have not changed the number of procedures. Ninety-two respondents (48.2%) continue to perform the same number of emergency urolithiasis procedures, whereas 66 (34.5%) have reduced and 27 (14.1%) have increased the number of procedures. The remaining five (2.6%) urologists have stopped performing any operations, even emergency operations.
ESWL management was stopped by 98 (51.3%) of the urologists and reduced by 64 (33.5%) but remained unchanged by 18 (9.4%).Most of these respondents have changed the mode of anaesthesia to spinal anaesthesia. For example, 76 (39.7%) reported using spinal anaesthesia for all their patients and 16 (8.5%) for patients with proven COVID-19 infection. In contrast, 67 (35.1%) reported no change in anaesthesia preference in response to the pandemic.
To prevent infection, 112 (58.6%) urologists are screening their patients preoperatively, and 32 (16.5%) have worn full PPE routinely since the start of the pandemic.
In managing ureteral stones in patients lacking urinary tract infection and with unknown COVID-19 status, 67 (35.1%) urologists prefer more conservative management, 53 (27.7%) favour instant drainage followed by ureteroscopy after the easing of lockdown measures, 40 (20.9%) reported no change in management and 27 (14.1%) favour ureteroscopy for stone clearance. This is illustrated in Figure 3. These physicians were highly susceptible to COVID-19 infection, with 22 (11.5%) urologists found to be infected by positive swab results. Hospitals have been advised to support their employees psychologically, as evidenced by the 38 (19.9%) who received mental health support. Assessment of the impact of COVID-19 on these urologists showed that 107 (56%) were not affected, 55 (28.8%) had mild salary reduction, 25 (13.1%) experienced an almost 50% reduction in salary, and three (1.6%) stopped working because of the lockdown. Urologists are actively involved in COVID-19 management, with 84 (44%) shifting their medical practice from urology to volunteer in the treatment of COVID-19 patients. The impact of COVID-19 pandemic on urologists is illustrated in Figure2.
Discussion
About one-third of the respondents were from the state of Qatar. Response rates do not reflect the relative number of urologists in the six countries but may reflect the short time provided for the return of the survey. A large country like KSA requires more than one focal urologist, as well as additional time to reach urologists throughout the entire country. In 2016, approximately 257 urologists were estimated to be working in governmental hospitals (2), suggesting that our survey included only a small percentage of practicing urologists-most of the urologists who participated in the survey work in the governmental sector. In contrast, more than 50% of practicing urologists in the United States work in private practice [3].
The outbreak of COVID19 led most of the GCC to adopt lockdown measures, including preventing people from entering these countries during the outbreak period. Furthermore, medical services to treat COVID-19 patients were increased in most of these countries, including an increase in staff to provide these services. This led to an increase in staff exposure to COVID-19, increasing the incidence of COVID-19 among the staff. This, in turn, reduced the number of staff members available to treat COVID-19, requiring the deployment of urologists to work in COVID-19 facilities and reducing the ability to provide non COVID-19 related services.
Similar to other countries, most countries in the GCC have utilized telephone communications or telemedicine to manage outpatients, restricting surgery to emergency and oncology procedures. Also, the duty hours for physicians increased from 8 to 12 hours per day, making more staff members available to work in COVID-19 facilities. This was reflected in the survey results, as nearly two-thirds of the urologists were treating COVID-19 infected patients, whereas only about 25% continued practicing urology, which likely consists of emergency and oncology services. Similar changes were applied during the outbreak of COVID19 in Singapore [4].
EAU guidelines advise following local recommendations to test staff and patients for COVID-19 if resources are available [5]. Nearly two-thirds of the respondents are testing their patients for COVID-19 preoperatively, and only 16% reported wearing full PPE. This does not conform to EAU guidelines, perhaps because of a relative lack of availability of the test kits or the equipment for full PPE. The EAU guidelines advise full PPE, irrespective of the COVID status of the patient [5].
Testing patients for COVID-19 is crucial because asymptomatic patients from Wuhan, China, who tested positive for COVID-19 before surgery, had a postoperative mortality rate of 20% [6].
Since the EAU guideline considered that surgery is harmful to the patients if he is tested COVID positive, this should result in a change in the practice of management of urolithiasis. Our survey showed inconsistencies in the management of urolithiasis during the COVID-19 pandemic. For example, 20% of urologists surveyed did not alter their management of ureteral stones in the absence of infection, with only 38% selecting conservative management (Figure3).
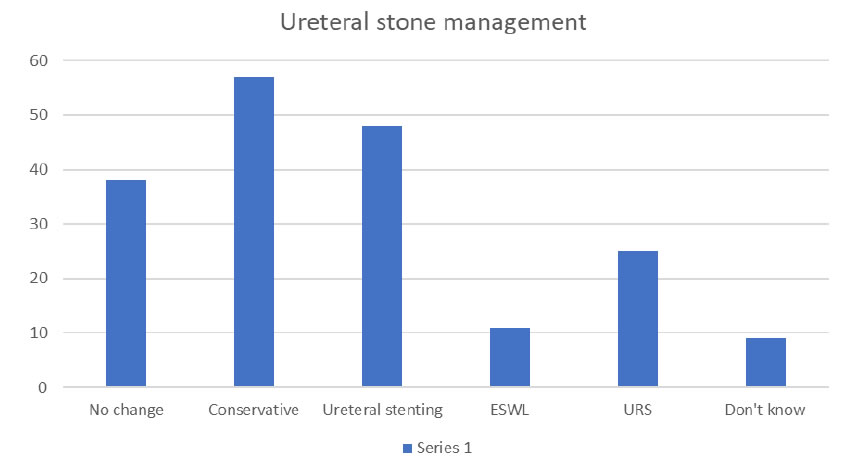
Figure 3. Management of ureteral stones in patients lacking urinary tract infection and with unknown COVID-19 status.
Studies have advised that, whenever possible, patients should be treated non-surgically or surgery should be deferred until the demands for ventilators and inpatient beds are reduced [7]. The EAU guidelines recommend treating intermediate priority patients if the capacity is available but not during COVID-19 surge [5].
Healthcare workers are members of the frontline response team and are therefore highly susceptible to infection. The WHO–China Joint Mission on COVID-19 reported that by 20 February 2020, there were 2,055 laboratory-confirmed cases of COVID-19 among healthcare workers, with 22 (1.1%) deaths [8].In Italy, at least 2,629 health workers, or 8.3% of all infected individuals, have been infected with coronavirus since the pandemic broke out in February [9]. In our survey, 11.5% of respondents were laboratory confirmed as having COVID-19. In addition to the infection itself, COVID-19 may be an independent risk factor for mental health problems in health care workers, including depression, anxiety, insomnia, and distress [10,11]. The WHO recommendations for health workers mention various hazards, including exposure to the pathogen, long working hours, psychological distress, fatigue, occupational burnout, stigma, and physical and psychological violence [12]. The WHO recommendations include providing access to mental health and counselling resources. This is supported by our survey, which found that 20% of the respondents had been provided mental health support by their facilities. The lockdown has also had an economic impact on the urologists working in this region. For example, our survey found that 75% of the urologists working in government hospitals, as well as some in private hospitals, were mildly affected economically, whereas around 15% experienced a greater economic impact, which may worsen the psychological impact of the pandemic on health care workers. The effect of COVID-19 on urologists in each country is illustrated in Figure 2.
Despite surveying a relatively large number of respondents, the results of this survey were limited by its narrow distribution among urologists in the region, which may have led to uneven distribution and collection bias. This may have been avoided had the survey been kept open for a longer period. However, this survey explored the common and variable practices among the health care organizations in the Gulf countries and emphasized the need for further studies to compare various practice strategies. The survey also showed the relatively high risk of COVID-19 infection to urologists, which warrants further evaluation by well-designed observational studies.
Conclusion
COVID-19 is hazardous to urologists in GCC countries, with 11.5% being infected and most reducing their clinical duties related to urolithiasis management. Although urolithiasis management in GCC countries during the COVID-19 pandemic was generally consistent with worldwide guidelines, some differences were observed, with further studies warranted to compare different management strategies.
References
- Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten C, et al. (2020) The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiology 5: 536-544.
- Otaibi KE (2016) Challenge facing the urologist in Saudi Arabia in the future. Urol Ann 184-188.
- The State of the Urology Workforce and Practice in the United State (2018).
- Chan MC, Yeo SEK, Chong YL, Lee YM (2020) Stepping Forward: urologists’ Efforts during the COVID-19 outbreak in Singapore. EurUrol 78: 38-39. [crossref]
- European Association of Urology. https://uroweb.org/wp-content/uploads/EAU-Guidelines-Office-Rapid-Reaction-Group-An-organisation-wide-collaborative-effort-to-adapt-the-EAU-guidelines-recommendations-to-the-COVID-19-era.pdf
- Lei S, Jiang F, Su W, Chen C, Chen J, Wei W, et al. (2020) Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 21: 100331. [crossref]
- Stensland KD, Morgan TM, Moinzadeh A, Cheryl T, Briganti A, et al. (2020) Consideration in the triage of urologic surgeries During the COVID-19 pandemic. EurUrolEpub 77: 663-666.
- World Health Organization. 2020. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)
- Psychiatry Res (2020) Jun; 288: 112972. Published online 2020 of Apr 13. doi: 10.1016/j.psychres.2020.112972. PMCID: PMC7152886
- SaiSpoorthy M, KarthikPratapa S, Supriya M (2020) Mental health problems faced by healthcare workers due to the COVID-19 pandemic- A review. Asian J Psychiatr 51: 102119. [crossref]
- Jianbo Lai, Simeng Ma, Ying Wang, ZhongxiangCai, Jianbo Hu, et al. (2020) Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open 3: 203976.
- Coronavirus disease (COVID-19) outbreak: rights,roles and responsibilities of health workers, including key considerations for occupational safety and health. 18 March 2020. COVID-19: Schools, businesses and institutions. WHO reference no.: WHO/2019-nCov/HCW_advice/2020. https://apps.who.int/iris/rest/bitstreams/1272583/retrieve.