Abstract
Lisfranc fracture-dislocation injuries are commonly associated with axial loading on plantar flexed foot [1]. The trauma causing the injury can occasionally be either a low or a high energy trauma [2]. Lisfranc fracture-dislocation injuries are often treated with open reduction and internal fixation [3]. Status of the soft tissues and the skin should be assessed before any surgical intervention [4]. Here we present a case of Lisfranc fracture-dislocation initially treated with open reduction and internal fixation which consequently developed soft tissue problems and had to be operated several more times. Six months after the injury the patient had mild midfood pain, no activity limitations and no soft tissue problems.
Introduction
The tarsometatarsal join is often called the Lisfranc joint [5]. Lisfranc injury is a rare foot trauma and it’s diagnosis is often missed [1]. It accounts for 0.2% of all fractures [6]. It is more common in males than females [3]. Lisfranc injuries lead to functional problems and gait impairty. Lisfranc injuries are generally classified using the Hardcastle & Myerson classification system. Lisfranc injuries are considered intra-articular injuries which concern the tarsometatarsal joint [5]. In high-energy traumas, there is often associated fractures and the Lisfranc injury can be missed in the acute polytrauma setting [7]. Early diagnosis of a Lisfranc injury is important to achieve anatomic reduction which is the most important surgical parameter to avoid long term complications such as flatfoot deformity, loss of medial arch of foot, limited range of motion, arthrosis and chronic pain syndrome [8]. The aim of Lisfranc injury treatment is to provide rapid soft tissue healing, prevention of repositioning, and stabilization of foot structures at the same time [9].
Here, we present a case of lisfranc fracture-dislocation who had been struggling with soft tissue complications. The treatment plan process of the case was arranged in accordance with orthopedic practice.
Case Report
A 51-year-old male applied to our emergency service after a tractor trailer fell on his feet. About two hours after the trauma, the patient presented to the emergency room. No neurovascular deficit was detected after the first evaluation in the emergency department. His foot was sore and swollen with a ‘toe up’ sign. After the radiological examinations, 2-3-4 metatarsal basis, middle and lateral cuneiform fractures were identified. Short leg plaster splint was applied after the patient was evaluated after consultation from the emergency department to the orthopedic clinic. In the radiological examinations performed in the emergency room, it was observed that the fleck sign and the alignment of the 2nd metatars with the medial edge of the medial cuneiform were impaired. As a result, the patient was diagnosed with type B2 Lisfranc fracture-dislocation. The patient was hospitalized in the orthopedic service for operation preparation. In accordance with his orthopedic practice, after 48 hours of moderate elevation, cold application and skin circulation, it was decided that the soft tissue was suitable for surgery and the patient’s surgery was performed (Figure 1)

Figure 1: Foot anteroposterior and lateral views
Surgical Procedure
After spinal anesthesia and pneumatic tourniquet application in the orthopedic operating room, the Lisfranc joint was approached with a dorsomedial incision of the foot after proper surgical preparation. After establishing a medial cuneiform relationship with the 2nd metatarsal, a headless cannula screw was sent to the medial cuneiform and 1st metatarsal joint. Afterwards, the medial cuneiform and the base of the second metatarsal were fixed with a headless cannulated screw while the reduction was maintained with the help of a clamp. After it was observed that lisfranc joint alignment was achieved with fluoroscopy controls, additional 3 percutaneous kischner wires provided support for the stability of the foot columns . After bleeding control and washing, the layers were closed in accordance with the anatomy. There was no opening in the skin after wound closure (Figure 2)

Figure 2: Postoperative foot anteroposterior, lateral, oblique views
A few days after the operation, skin necrosis began to develop on the dorsal side of the patient’s foot. It was thought that the discharges in the dorsum of the foot were due to necrotic tissue rather than infection. The patient was followed up with daily antibiotic-pomade-dressing, elevation and ice compression for two weeks. Intravenous dextran was used to avoid distal circulation problems. The patient was followed up daily before discharge due to necrosis and wound follow-up in the dorsum of the foot. When the demercation line became evident in wound necrosis, surgery was planned for the patient on the 15th postoperative day. A meticulous and detailed debridement and vacuum assisted closure (VAC) application was performed together with the plastic surgeon. Wound culture samples were taken during the surgical procedure. The culture sample was examined and S. aureus was identified by the laboratory. The patient was given vancomycin treatment for two weeks in line with the recommendations of the infectious diseases clinic. During the next two weeks, the debridement and VAC application procedure was performed four more times. The K-wires were removed approximately 1 month after the initial surgical fixation. In this process, the patient was consulted to the plastic and reconstructive surgery clinic and the infectious diseases clinic, and as a result of a multidisciplinary approach, sural fasciocutaneous flap operation was decided (Figure 3).

Figure 3: Wound necrosis and debride
The wide skin opening on the dorsum of the foot was closed with the planned sural fasciocutaneous flap with the support of the plastic surgery clinic. Flap viability was closely monitored in the first 48 hours after surgery. High sensitivity was shown in terms of daily circulation control, dressing applications and protection from infection (Figure 4). The patient was followed at the service for one more week. During this period, the distal part of the muscle flap developed skin necrosis. The decision was made again, together with the plastic and reconstructive surgery department. Thus, a skin graft was applied to the necrotic part of the dorsal side of the foot by the plastic and reconstructive surgery team. The patient was followed for one more week. He was dismissed as his neurovascular status was very good and his flap vitality was fine.
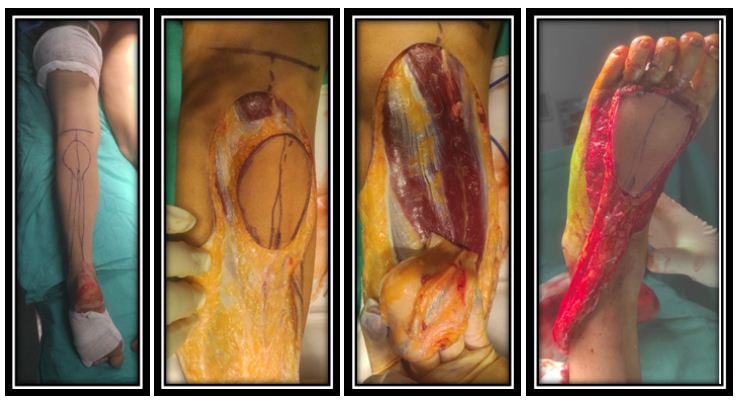
Figure 4: Fasciocutaneous flap surgery stage
After flap surgery, the patient was followed up in the ward for one more week. Outpatient follow-up from the outpatient clinic continued for about 6 months. Daily dressing with rifampicin was recommended to the patient. Oral antibiotic therapy was discontinued after discharge. After the flap sutures were removed, rifampicin administration was also discontinued. At 6th week partial weight-bearing was started and full weight-bearing was achieved in the 12th week. At the 6th month follow-up appointment of the patient, no signs of infection or soft tissue problems were detected. The patient had 10 degrees of dorsiflexion and 40 degrees of plantar flexion in ankle range of motion. Visual analogue scale (VAS) score was 30, American Orthopedic Foot & Ankle Society (AOFAS) function score was 39, and compliance score was 8, reaching a total of 77. There was no obstacle in finger flexion and extension (Figure 5).

Figure 5: At last control, skin fotography and anteroposteior/lateral radiographies
Discussion
Lisfranc fracture dislocation describes a range of injuries, from occult fractures/ligamental injuries to open crush injuries with extensive bone/soft tissue damage [10]. Early diagnosis of a Lisfranc injury is important to achieve anatomic reduction which is the most important surgical parameter to avoid long term complications [8]. Anatomical realignment, stabilization, and soft tissue coverage are key principles in the management of Lisfranc injuries [11]. There is no general consensus on the best fixation method. However, the current trend is to treat this injury with open anatomical reduction and internal fixation [12,13]. It is stated that in Lisfranc-fracture dislocation, soft tissue damage caused by inflammation and edema may affect the results more than the delay in surgical treatment, so early diagnosis is very important to avoid this [14]. Soft tissue management is fundamental for a Lisfranc injury treatment [15]. As the literature suggests, we made an early diagnosis of lisfranc fracture-dislocation injury in our case. Since there was no displaced joint dislocation, the surgical timing was decided according to soft tissue suitability. Open reduction and internal fixation were performed for the patient’s lisfranc injury in accordance with the guidelines.
In the treatment of Lisfranc fracture-dislocations, both the severity of soft tissue damage and non-anatomical reduction are unfavorable prognostic factors [16]. Soft tissue treatment is especially important in open Lisfranc fracture-dislocation. Compared to conventional methods, the vacuum assisted closure technique resulted in earlier wound closure, clean wound surface drainage, faster detumescence, accelerated tissue growth, and reduced clinical workload [17,18]. In the article by Wenqing Qu et al. [19] on open lisfranc injury, when the vacuum assisted closure was first replaced 5-7 days after surgery, wounds healed well in most cases. The soft tissue was quickly repaired by direct suture, skin graft, or skin flap transplantation, thanks to emergency measures such as washing with large volumes of normal saline. It has been mentioned that holding as much skin as possible, avoiding high tension sutures are essential elements for soft tissue closure in lisfranc injuries. An aggressive management by use of a ‘one-stage fix and flap protocol’ has been proven effective in the treatment for severe open fractures of the tibia (Gustilo IIIb or IIIc). This protocol consisted of immediate radical wound debridement, skeletal stabilisation and immediate soft-tissue cover [20]. In the case report of Ilknur et al. regarding another open lisfranc injury, a radical debridement of the foot followed by a Thiersch skin graft was performed one month after surgery due to superficial necrosis of the interposition skin flap. Four months after surgery, a patient with excellent wound healing and good functional outcome was seen. As it is understood from the studies, lisfranc injuries are a type of injury that is pregnant with soft tissue problems. Close follow-up of soft tissue and timing of surgery are the most essential points. It has been mentioned that even flap application can be performed in a single session in open lisfranc injuries. We believe that soft tissue healing aids such as not tight closure of the soft tissue, gradual closure and VAC application should be considered in lisfranc closed fractures. Otherwise, more serious soft tissue problems may be encountered.
There are very limited studies on soft tissue healing in lisfranc injury in the literature. Most of these studies also deal with open lisfranc injuries. In our case report, we encountered serious soft tissue problems, although we continued the treatment process of the patient, whom we diagnosed and treated with closed lisfranc fracture-dislocation, in accordance with the guidelines. Along with the Plastic and Reconstructive Surgery clinic, more difficult and costly surgical treatments were applied. Although the functional result is satisfactory, the lesson we will learn from our case is which methods can be preferred to provide soft tissue healing without complications.
Conclusion
Goal of the treatment of Lisfranc fractured location is to achieve a painless, functional plantigrade foot with a good appearance. The issue that we want to emphasize in our case is the timing of surgery in closed Lisfranc fracture-dislocations. As much as possible, minimally invasive approaches should be prioritized. Avoiding the use of tight sutures during surgery for the healing of soft tissue, and secondary healing can be considered with VAC application when necessary. It should be considered that closing the wounds with skin flaps, which can be closed with a partial skin graft if necessary, leads to possible consequences such as prolongation of the process, decrease in functional results and increase in cost.
References
- Desmond EA, Chou LB (2006). Current concepts review: Lisfranc injuries. Foot Ankle Int 27: 653-660. [crossref]
- Renninger CH, Cochran G, Tompane T, Bellamy J, Kuhn K (2017). Injury Characteristics of Low-Energy Lisfranc Injuries Compared With High-Energy Injuries. Foot Ankle Int 38: 964-969. [crossref]
- Moracia-Ochagavía I, Rodríguez-Merchán EC (2019). Lisfranc fracture-dislocations: current management. EFORT Open Rev. Jul 4: 430-444. [crossref]
- Peicha G, Labovitz J, Seibert FJ, Grechenig W, Weiglein A, et al. (2002). The anatomy of the joint as a risk factor for Lisfranc dislocation and fracture-dislocation. An anatomical and radiological case control study. J Bone Joint Surg Br 84: 981-985. [crossref]
- Myerson MS, Fisher RT, Burgess AR, Kenzora JE (1986) Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot Ankle 6: 225-242. [crossref]
- Myerson MS, Cerrato R (2009). Current management of tarsometatarsal injuries in the athlete. Instr Course Lect 58: 583-594. [crossref]
- Feng P, Li YX, Li J, Ouyang XY, Deng W, et al. (2017). Staged Management of Missed Lisfranc Injuries: A Report of Short-term Results. Orthop Surg 9: 54-61. [crossref]
- Aronow MS (2006) Treatment of the missed Lisfranc injury. Foot Ankle Clin 11: 127-142. [crossref]
- Kamin K, Rammelt S, Kleber C, Marx C, Schaser KD (2020). Fixateur externe: temporäre Fixation und Weichteilmanagement am oberen Sprunggelenk [External fixator: temporary fixation and soft tissue management of the ankle]. Oper Orthop Traumatol 32: 421-432.
- Ahmed N, Kugan R (2015) Ilizarov frame delayed internal fixation of Lisfranc fracture dislocation with severe soft tissue injury: New technique. Trauma Case Rep 1: 88-94. [crossref]
- Panagiotis S, Craig SR, Fragiskos NX, Peter VG (2010) The role of reduction and internal fixation of Lisfranc fracture-dislocations: a systematic review of the literature. Orthop 34: 1083-1091. [crossref]
- Boffeli TJ, Pfannenstein RR, Thompson JC (2014). Combinedmedial column primary arthrodesis,middle column open reduction internal fixation, and lateral column pinning for treatment of Lisfranc fracture-dislocation injuries, Foot Ankle Surg 53: 657-663. [crossref]
- García-Renedo RJ, Carranza-Bencano A, Leal-Gómez R, Cámara-Arrigunaga F. (2016)Análisis de las complicaciones en pacientes con fractura-luxación de Lisfranc [Complication analysis in Lisfranc fracture-dislocation]. Acta Ortop Mex 30: 284-290. [crossref]
- Gu W, Shi Z (2017) Staged management of open Lisfranc injury: Experience from 14 patients. Medicine (Baltimore) 96: e6699. [crossref]
- Demirkale I, Tecimel O, Celik I, Kilicarslan K, Ocguder A et al. (2013) The effect of the Tscherne injury pattern on the outcome of operatively treated Lisfranc fracture dislocations. Foot Ankle Surg 19: 188-193. [crossref]
- Li W, Ji L, Tao W (2015) Effect of vacuum sealing drainage in osteofascial compartment syndrome. Int J Clin Exp Med 8: 16112-16116. [crossref]
- Ko YS, Jung SW. (2014).Vacuum-assisted close versus conventional treatment for postlaparotomy wound dehiscence. Ann Surg Treat Res 87: 260-264. [crossref]
- Qu W, Ni S, Wang Z, Zhao Y, Zhang S, (2016) Severe open Lisfranc injuries: one-stage operation through internal fixation associated with vacuum sealing drainage. J Orthop Surg Res 11: 134. [crossref]
- Gopal S, Majumder S, Batchelor AGB, Knight SL, De Boer P et al. (2000). Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br 82-B: 959-966. [crossref]
- Sanli I, Hermus J, Poeze M (2012). Primary internal fixation and soft-tissue reconstruction in the treatment for an open Lisfranc fracture-dislocation. Musculoskelet Surg 96: 59-62. [crossref]