DOI: 10.31038/MIP.2023412
Abstract
Introduction: Prolonged viral persistency and shedding are the major concerns associated with emerging variants of SARS-CoV-2. Complete viruses and viral fragments may persist for unusual and longer periods in both symptomatic and non-symptomatic patients.
Case presentation: In this study, we have reported unusual persistency of SARS-CoV-2 in 26 years old young patient from Islamabad, Pakistan.
Conclusion: In conclusion, to avoid viral persistency for a long duration, precise treatment and immune-boosting therapies must be recommended. Further, nontherapeutic interventions and preventive measures are necessary to avoid viral transmission and possible reinfection.
Keywords
COVID-19, Immunocompromised, Persistency, Viral shedding
Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the causative agent of Coronavirus disease 2019 (COVID-19) is a major concern of twenty first century [1]. This detrimental zoonotic and highly transmissible virus is responsible for the ongoing pandemic and poses threats to public health globally [2]. Continuous efforts revealed the epidemiology, pathogenicity, presiding results, genomic sequences, and precise diagnostic approaches of SARS-CoV-2 infections. Despite these facts, the burden of pandemic is still increasing due to the emerging variants[3,4], microbial coinfections [5], recrudescence [6], reinfections [7], prolonged viral shedding [8] and persistent RNA positivity [9] (Table 1).
Table 1: Definitions
|
Terms |
Descriptions |
| Persistency | Unusual and prolonged presence of viral RNA in the body fluids. |
| Re-positivity | Detecting the presence of viral RNA following negative RT-PCR tests up to 90 days. |
| Recrudescence | Reactivation/ relapse of infection after clinical improvement within 90 days of first infection due to persisting viral fragments. |
| Reinfection | Infection caused by same or phylogenetically distinct respiratory and non-respiratory viruses after natural immunity and or vaccination. |
Recently, patients with COVID-19 revealed persistently positive SARS-CoV-2 nucleic acid test results despite resolved clinical symptoms have attracted a lot of attention [10]. Researchers assumed long-term persistency of virus in the human body even after apparent recovery or negative results of nasopharyngeal specimens via PCR. Viral load appeared to be higher in the upper respiratory tract within the first week after symptom onset, and later in the lower respiratory tract. Viral shedding and viral load are important determinants of disease progression and transmission [11].
In this study, we reported a ruled-out case of SARS-CoV-2 in young male patient of 26 years from Islamabad Pakistan, with extremely prolonged and persistent viral shedding for six weeks.
Case Presentation
A young student of 26 years with past medical history of respiratory tract problems including pulmonary tuberculosis, recovered in 2019 with COVID-19 symptoms including cough, fatigue, body pain and mild dyspnea introduced for the diagnosis of SARS-CoV-2 infection. The RT-PCR of nasopharyngeal samples were tested positive initially on April 20, 2021. Self-isolation was suggested with symptoms resolving treatment (paracetamol). The test was performed after RNA extraction (Qiagen Viral RNA Mini Kit) on ABI 7500 Real-Time PCR detection system with internal and external positive controls via the SARS-CoV-2 detection protocols.
After initial diagnosis, the patient was again COVID-19 positive after five days i.e. on April 25, 2021. At this stage, no clinical or physical examinations were performed while antibiotic treatment was recommended for five days. The symptoms were resolved during first week of antibiotic treatment. On May 18, 2021, persistency for SARS-CoV-2 with altered and mild symptoms were observed again. The major symptoms were anosmia and dyspnea (Figure 1 – Case timeline). Empirical antibiotic treatment was recommended to overcome the possible health problems i.e. Azithromycin 500 mg/day with two-fold increase compared to initial dose of 250 mg/day.
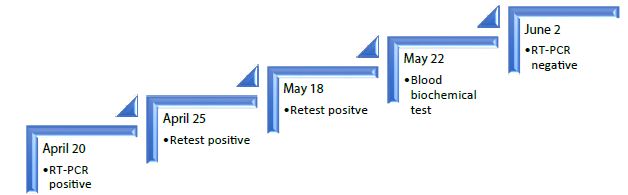
Figure 1: Case timeline of patient 1 (male, age 26 years)
To investigate the patients’ health status and immune response, recommended biochemical tests were performed on 33rd day of infection i.e. on May 22, 2021. Anti-SARS-CoV-2 antibody test was performed on Cobas e411 analyzer (Diagnostic Roche), a fully automated instrument employing Electro Chemiluminescence (ECL) technology for immunoassay analysis using FDA approved kits in human serum and plasma, revealed development of SARS-CoV-2 antibodies (titer 15.13 cut of index COI > 1).
The health status was normal with mild morbidity as the biochemical markers associated with COVID-19 including Ferritin, C-reactive proteins (CRP) and D-dimers were normal (Table 2). Complete blood count revealed drop in neutrophil counts while lymphocytes level was high (Table 3). Fortunately, the patient was declared recovered according to general discharge criteria (Figure 2) [12] on 43rd day of primary infection.
Table 2: Biochemical tests
|
Tests |
Value |
Reference value |
Interpretation |
| Ferritin |
160.9 ng/ml |
14-250 |
Normal |
| CRP |
0.13 mg/l |
0.00-10.00 |
Normal |
| FDPs (D-Dimer) |
0.1 mg/l |
0.00-0.50 |
Normal |
| Antibodies |
15.13 COI |
Cut off 1.00 |
Reactive |
Abbreviations: CRP: C-reactive proteins; FDPs: Fibrin Degradation Products, COI: Cut Off Index.
Table 3: Complete blood count
|
Parameters (units) |
Reference value |
Value |
| White blood cells (TLC) (10⁹/L) |
4.00-11.00 |
5.8 |
| Neutrophils (%) |
50.00-70.00 |
40 |
| Lymphocytes (%) |
20.00-40.00 |
48 |
| Monocytes (%) |
3.00-12.00 |
10 |
| Eosinophils (%) |
0.50-5.00 |
02 |
| Basophils (%) |
0.00-1.00 |
0.0 |
| Red blood cells, count (Mil/Cm) |
4.00-6.00 |
5.02 |
| Hemoglobin (Hb) (Gm/dl) |
11.00-16.00 |
14.0 |
| Hematocrit (PCV) (%) |
37.00-54.00 |
46.5 |
| MCV (f/L) |
80.00-100.00 |
93.0 |
| MCH (Pgm) |
27.00-34.00 |
27.8 |
| MCHC (g/L) |
30.00-36.00 |
30.0 |
| Platelets (10⁹/L) |
150.00-450.00 |
333 |
| MPV (f/L) |
7.00-11.00 |
7.5 |
| PDW (f/L) |
8.30-25.00 |
16.2 |
| Procalcitonin (mL/L) |
1.08-2.82 |
1.82 |
Abbreviations: TLC: Total Leucocytes Counts, PCV: Packed Cells Volume, MCV: Mean Corpuscular Volume, MCH: Mean Corpuscular Hemoglobin, MCHC: Mean Corpuscular Hemoglobin Concentration, MPV: Mean Platelet Volume, PDW: Platelet Distribution Width.
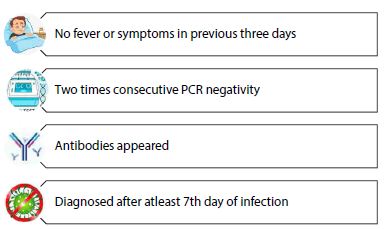
Figure 2: Criteria of discharge/declaring recovered
Discussion
Viral load remains high in upper respiratory tract during first week of infection or onset of symptoms and tends to decrease with time. Virus median duration of shedding is 8 days post onset of symptoms and drops below 5% after 15.2 days post onset of symptoms [13]. However, recent studies demonstrated viral shedding for long duration in immune-compromised individuals [14] in both symptomatic and asymptomatic patients of older age [15]. The current study reported unexpected and persistent infection of SARS-CoV-2 in young patient of 26 years for more than six weeks. To our understanding, this is the first report addressing prolonged and persistent viral positivity from Pakistan.
RT-RNA based repeated RNA positivity was considered primary indication of persistent infection as documented in previous studies [16]. Persistent shedding was significantly associated with persistent dyspnea and anosmia. Detection of viral RNA and confirmed retest positivity for SARS-CoV-2 in recovered patients is clinical indication of prolonged viral persistency or relapse of infection [17]. Analgesics and Azithromycin were recommended to eradicate disease morbidity. In persistent COVID-19 treatment, azithromycin plus hydroxychloroquine were more efficient previously [18].
In contrast to our findings, a study reported SARS-CoV-2 persistency for 59 days in young female patient with the age of 25 years [16]. The patient recovered without any antibiotic and antiviral therapy as no consequences were observed with health issues and underlying morbidities. Another case report from Thailand revealed prolonged SARS-CoV-2 shedding in asymptomatic patient (age 30 years) for 110 days [15]. Symptoms resolution with shedding duration or asymptomatic patient could promote disease transmission and hence asymptomatic virus carriers can be still infectious [19]. Therefore, there is need of monitoring the surroundings of patients to prevent the risk of viral transmission.
Immunodeficiency plays a major role in prolonged viral shedding that can be observed even in asymptomatic individuals with weak immune system [14,20]. We demonstrated that delayed treatment, low dose medication, previous medical history, higher susceptibility due to weak immune system were responsible for persistent viral infection. Similarly, viral clearance in COVID-19 patients varies and delayed in patients with older age, multiple re-exposure, underlying comorbidities such as diabetes [21] respective therapies [22] and myeloma [23] etc. (Figure 3).

Figure 3: Major reasons of that can contribute to prolonged viral shedding (SARS-CoV-2)
The worldwide discharge criteria (Figure 2) are improved clinical symptoms and two PCR negative test, needs modification for accurate and precise diagnosis [12]. Various studies emphasize precise and accurate decision of prolonged viral shedding and true infection. Confirmation and differentiating these hurdles might provide an insight of infection and beneficial support to the physician while treating the victim [24].
In addition, the patients experiencing only mild symptoms with extreme infection develops a weaker immune response which might explain predisposition to the reinfection [25]. Prolonged viral shedding and its particles poses diagnostic challenges. It might complicate infection control, treatment and might significantly contribute its role in morbidity and mortality associated with COVID-19 [26].
We declared patient recovered based on general discharge criteria (Figure 2). Laboratory biochemical tests, development of antibodies and clearance of symptoms are major factors which helped declaring recovery of patient from this regime. In summary, the possibility of prolonged viral shedding is significantly associated with health status of patient, timely diagnosis, and treatment strategies without any discrimination of age and gender. Further, patients recovered in long duration should be vaccinated after few weeks of recovery to prevent reinfection with emerging variants of SARS-CoV-2.
Conclusion
Comorbidities, immunodeficiency, unspecific drugs, drug discontinuation and wanning immunity are the major contributors of prolonged and persistent viral infection. These regimes might further increase the susceptibility of patient for reinfection with various emerging variants. In this ruled out situation, the unusual persistency of SARS-CoV-2 and delayed viral clearance could be due to weak immune system, previous history of lung infection (tuberculosis) and drug discontinuation. In conclusion, to avoid viral persistency for long duration, precise treatment and immune boasting therapies must be recommended.
Funding
No funding or grant was received
Conflict of Interest
The authors declare no competing interest
References
- da Costa VG, Moreli ML, Saivish MV (2020) The emergence of SARS, MERS and novel SARS-2 coronaviruses in the 21st century. Arch Virol. [crossref]
- Hu B, Guo H, Zhou P, Shi ZL (2020) Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol.[crossref]
- Nonaka CKV et al (2021) Genomic Evidence of SARS-CoV-2 Reinfection Involving E484K Spike Mutation, Brazil. Emerg Infect Dis. [crossref]
- Hafeez S, Din M, Zia F, Ali M, Shinwari ZK (2021) Emerging concerns regarding COVID-19; second wave and new variant. J Med Virol. [crossref]
- Chen X et al.(2020) The microbial coinfection in COVID-19. Appl Microbiol Biotechnol. [crossref]
- Yuan B et al.(2021) Recurrence of positive SARS-CoV-2 viral RNA in recovered COVID-19 patients during medical isolation observation. Sci Rep. [crossref]
- Brehm TT et al.(2021) Sars-cov-2 reinfection in a healthcare worker despite the presence of detectable neutralizing antibodies. Viruses. [crossref]
- Li J, Zhang L, Liu B, Song D (2020) Case Report : Viral Shedding for 60 Days in a Woman with COVID-19. Am J Trop Med Hyg. [crossref]
- Yang JR, Deng DT, Wu N, Yang B, et al. (2020) Persistent viral RNA positivity during the recovery period of a patient with SARS-CoV-2 infection. J Med Virol. [crossref]
- Wang W et al.(2020) Persistent SARS-COV-2 RNA positivity in a patient for 92 days after disease onset: A case report. Medicine (Baltimore) [crossref]
- Cevik M, Tate M, Lloyd O, Maraolo AE, et al. (2020) SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. The Lancet Microbe. [crossref]
- Falahi S and Kenarkoohi A (2020) COVID-19 reinfection: prolonged shedding or true reinfection? . New Microbes New Infect. [crossref]
- van Kampen JJA et al. (2021) Duration and key determinants of infectious virus shedding in hospitalized patients with coronavirus disease-2019 (COVID-19) . Nat Commun. [crossref]
- Tarhini H et al. (2021) Long-Term Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infectiousness Among Three Immunocompromised Patients: From Prolonged Viral Shedding to SARS-CoV-2 Superinfection. J Infect Dis. [crossref]
- Individual A, Study AC, Kewcharoenwong C, Khamduang W,et al.(2022) Prolonged Detection of SARS-CoV-2 RNA in An. Emerg Infect Dis. [crossref]
- Penchenat A, Alavi Z, Payan C, and Pers JO (2020) Prolonged 59-day course of COVID-19: The case of a SARS-CoV-2 shedding persistency in a healthcare provider. Clin Case Reports. [crossref]
- Yahav D et al.(2022) Definitions for coronavirus disease 2019 reinfection, relapse and PCR re-positivity. Clin Microbiol Infect. [crossref]
- Drancourt M et al.(2021) SARS-CoV-2 persistent viral shedding in the context of hydroxychloroquine-azithromycin treatment. Viruses. [crossref]
- Zhang L, Li C, Zhou Y, Wang B, et al.(2020) Persistent viral shedding lasting over 60 days in a mild COVID-19 patient with ongoing positive SARS-CoV-2. Quant Imaging Med Surg. [crossref]
- Alsaud AE et al.(2021) Case report: Prolonged viral shedding in six COVID-19 patients. Am J Trop Med Hyg. [crossref]
- Buetti N et al.(2020) Diabetes mellitus is a risk factor for prolonged SARS-CoV-2 viral shedding in lower respiratory tract samples of critically ill patients. Endocrine. [crossref]
- Xiao AT, Tong YX, and Zhang S (2020) False negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: Rather than recurrence. J Med Virol. [crossref]
- Bellesso M, Bruniera FR, Trunkel AT, and Nicodemo IP (2020) Second COVID-19 infection in a patient with multiple myeloma in Brazil – reinfection or reactivation?. Hematol Transfus Cell Ther. [crossref]
- William A, Kaur R, and William A (2021) COVID-19 Reinfection and its Diagnostic Approach. vol. 31, 2021, doi: 10.3844/ajassp.2021.71.78.
- Roberts AT, Piani F, Longo B, Andreini R, et al.(2021) Reinfection of SARS-CoV-2 – analysis of 23 cases from the literature. Infect Dis (Auckl) [crossref]
- Elzein F et al.(2020) Reinfection, recurrence, or delayed presentation of COVID-19? Case series and review of the literature. J Infect Public Health. [crossref]