Abstract
Background: Healthcare waste is produced from various therapeutic procedures in hospitals, such as chemotherapy, dialysis, surgery, delivery, resection of gangrenous organs, autopsy, biopsy, and injections, and most of the wastes are toxic, harmful, carcinogenic, and infectious materials. Medical Waste handlers faced massive exposure to hazardous waste and occupational accidents as a result of manual handling of waste and working under unfavorable conditions. There are limited studies and updated information concerning these issues in the country.
Objective: To assess safety practice and associated factors among waste handlers at public hospitals in Somali Region, Ethiopia.
Method: An institutional-based cross-sectional study was carried out among 417 waste handlers in selected public hospitals from June 15 to July 15, 2021. Data were collected from respondents by using a simple random sampling technique. The collected data were entered into Epi-data 3.1 software and exported to SPSS 20 for analysis. Bi-variable analysis was done, and variables with p-values below 0.25 were identified as candidates for multi-variable analysis. Then multi-variable analysis was done, and an adjusted odd ration was computed and interpreted. A p-value less than 0.05 is the cut-off point for determining the significance of the association.
Result: The proportion of current safe practice among public hospital waste handlers was found to be 38.2% (95% CI: 33.2, 43.1). Good availability of safety materials (AOR=9.3; 95% CI: 5, 17.2), Good knowledge (AOR=7.2; 95% CI: 3.7, 14), a positive attitude (AOR: 5.4; 95% CI: 2.53, 11.47), and age group were significantly associated with safety practice.
Conclusion: The proportion of safe practices among hospital waste handlers was found to be low compared to national and international standards. Good knowledge, a positive attitude, a good supply of safety materials, and an age group are the determinants of safety practice. To provide good safety practice, adequate professional support and supervision should be in place to increase their knowledge about safety precautions, and similarly, providing enough safety materials is recommended to strengthen adherence to safety practice among hospital waste handlers.
Keywords
Safety Practice, Determinant Factors, Waste Handlers, Government hospitals, Somali Region, Ethiopia
Introduction
Workers and waste pickers handling solid waste throughout the world are exposed to occupational health and accident risks related to the content of the materials they are handling, emissions from those materials, and the equipment being used [1]. About 85% of wastes produced in health facilities are non-hazardous, and the remaining 15% of health care waste is characterized as hazardous and can pose a number of health risks [2,3]. Waste handlers are often at higher risk than health care professionals. Because healthcare professionals produce the waste and throw it in the garbage. However, waste handlers handle it extensively throughout, and mostly very little attention is given to their safety [4]. Medical waste handlers are working in a very poor and unsafe working environment, and mostly they are victims of occupational health hazards from poor safety practices [5]. The prevalence of needle stick injuries, sharp injuries, and blood and body fluid splashes among hospital waste handlers is higher because of the lack of personal protective equipment while on duty and inappropriate waste segregation practices [6]. The occupational safety of health care waste handlers cannot be overlooked because health care waste handlers are at constant risk of exposure to blood-borne pathogens .In Ethiopia, we have a set of Standard Precautions for health safety practices that have been demonstrated to be effective in reducing the occurrence of adverse healthcare events. Additionally, the set can help medical waste handlers and healthcare providers assess the degree to which safe practices have already been implemented in their settings and the degree to which the practices provide tangible evidence of the medical waste handler’s safety improvement and increased patient satisfaction and loyalty [7].
Worldwide, information on the spread of infections resulting from waste handling is limited. Studies from developed countries have shown that occupational exposure to waste may result from exposure to various work hazards [8]. There are studies showing different health complaints, such as respiratory problems [9,10], increased risk of hepatitis A and B [11,12] and skin diseases [13], for people working in waste handling. In addition, self-reported risks, including musculoskeletal, fatigue, gastrointestinal, and hearing complaints, were also identified [14]. Professional-related risk assessment reports showed that waste collectors had the third highest needle stick injury rate (18.4 per 1000 per year) and the second highest other sharps injury rate (7.1 per 1000 per year) compared with healthcare workers [15]. One study showed that each year, waste collectors reported 50–100 puncture wounds as a result of collecting medical waste from private medical practitioners and from the disposal of needles by drug addicts [16].Health care waste should be collected and transported in a safe way to avoid unnecessary exposure [17,18]. But about 58.8% and 41.2% of waste handlers were exposed to blood and body fluids due to carrying overfilled waste bags, which increase the risk of infection for different pathogens like HBV, HCV, and HIV/AIDS, and about 47% of medical waste handlers, had at least one accidental Sharp injury because of improperly discarded needles and sharp materials [19,20].Unavailability or shortage of personal protective devices aggravates the risk of acquiring infection while exposed to hazardous wastes (5). Waste handlers usually do not wear sufficient protective clothing during waste handling, which increases the potential risk of accidents .Inappropriate collection, storage, processing, transport, and handling of the health care waste exposes the staff of the facility, patients, and their attendants to the risk of serious health hazards. Many healthcare facilities in developing countries dispose of their waste in dustbins along with general waste; some even re-use sharps and syringes, thereby increasing the risk of transmission of infections [21].
Even though the impact of healthcare waste on healthcare workers is well described globally [22], less attention is given to waste collectors, and countrywide official statistical data do not address the health and working conditions of waste handlers [23].The study done in Eastern Ethiopia also showed that 30% of waste handlers were exposed to any sharp materials due to improper handling, poor waste segregation, and poor utilization of personal protective equipment (5). Waste handlers in Hawassa city in south Ethiopia have reported that they have experienced needle-stick injuries at least once in their lives at the different healthcare facilities, ranging from 25–100% [24,25].Studies in developing countries, including Ethiopia, indicate that there are limitations on safe waste handling practices among health care waste handlers due to different factors. However, there are few studies conducted regarding the prevalence of safety practices among hospital waste handlers in Ethiopia, and less attention is given to the prevalence of safety practices and factors exposing waste handlers to possible injuries and accidents. Hence, the intended study will determine the prevalence of safety practice and its associated factors among hospital medical waste handlers, which in turn will enable us to understand the overall situation of safety practice and minimize those factors that hinder the safety practice of hospital waste handlers.
Methods and Materials
Study Area and Period
The study was conducted in the Somali region, which is the second-largest and easternmost of the ten regions. The regional state borders the Ethiopian states of Afar and Oromia and the chartered city of Dire Dawa to the west, as well as Djibouti and Somalia to the south and north-east. Based on the 2007 census conducted by the central statistical agency of Ethiopia, the Somali region has a total population of 7,445, 2219, consisting of 3,472,490 men and 3,972,729 women. Urban inhabitants’ number 1,489,044 or 20% of the population and a further 5,956,175 or 80% were pastoralists and farmers. This region has an estimated density of 20.9 people per square kilometer in an area of 279,252 square kilometers. The region is divided into six councils and 93 districts for administrative purposes. The Somali Regional Health Bureau is responsible for the overall Health activity in the region.
There are Ten Primary Hospitals, Two General hospitals, and One Referral Hospital in the Somali region, namely, Dagahbour Primary Hospital, Qabri Dahare Primary Hospital, Warder Primary Hospital, Filtu Primary Hospital, Dollo Ado Primary Hospital, Raso Primary Hospital, Hargelle, Sitti/Biki Primary Hospital, Gashamo Primary Hospital, Fik Primary Hospital, Karamara General Hospital, Godey General Hospital, and Jig-jiga University. Sheik Hassen Yabare Referral Hospital, respectively, and the major common services given by those general hospitals and referral hospitals are maternal and child health services, prevention and control of major communicable diseases, non-communicable disease prevention and control, emergency services, laboratory services, and operational services. Generally, in the Somali region, there were approximately 710 medical waste handlers working in government hospitals. In selected hospitals, there were around 458 medical waste handlers. The study was conducted from June 15 to July 15, 2021, at public hospitals in the Somali Region and Eastern Ethiopia.
Study Design
Hospital based cross-sectional study was employed.
Source Population
Source populations were waste handlers working in Somali region public hospitals.
Study Population
All selected waste handlers working in the selected public hospitals during study period.
Inclusion Criteria
All waste handlers were enrolled in the selected government hospitals, present on duty during data collection period.
Exclusion Criteria
Waste handlers who were absent during the time of data collection and those with hearing impairments.
Sample Size Determination
Sample Size Calculation for the 1st Objective
The sample size for the first objective had been determined using the single population proportion formula by considering the prevalence of safe practice as 44.1% [26,27] from a previously conducted study on safety practice among waste handlers in Adisababa city administration public hospitals in central Ethiopia. Hence, assuming a 5% marginal error (d), a 95% confidence level (alpha=0.05), and the sample size for the first objective, it can be calculated as follows:
![]()
n=required sample size
Z=the standard normal deviation at 95%confidence interval=1.96
P=expected proportion (44.1%)
d=margin of error that can be tolerated 5% (0.05)
1-p=proportion of population that do not possess the character of interest.
Therefore n=(1.96) ^2 .0.441(1-0.559)=379
(0.05) ^2
=379 and by adding 10% non-response rate 417 was the sample size for the 1st objective.
Sample Size Calculation for the 2nd Objective
Sample size for specific objective 2 was calculated using the statcalc for sample size and power for cohort or cross-sectional studies of Epi Info version 7, considering the following assumptions (Table 1):
Therefore, from the calculated sample sizes for both objectives, the maximum sample size from the first objective, 417, was taken as the study sample since it covers the two objectives.
Table 1: Sample size determination for second specific objective using some important factors of safety practice
|
Factor |
Cl | Power (1-β) | Ratio | Proportion of outcome among exposed | Proportion of outcome among un-exposed | OR |
Sample size(n) |
| Good Knowledge (27) |
95% |
80% | 1 | (Good) 53.3% | (Poor) 24% |
3.57
|
100 |
| Received Training (28) |
95% |
80% | 1 | (Trained) 73% | (Not trained)53% | 2.39 |
202 |
| (Yes) Availability of colour coded bin (29) |
95% |
80% | 1 | (Yes)74.2% | (No)31.1% | 6.3 |
50 |
Sampling Technique
There are Ten Primary Hospitals, Two General hospitals, and One Referral Hospital in the Somali region; Three Primary Hospitals and One General Hospital were selected by lottery. Whereas the referral hospital was selected purposefully. Then the calculated sample size was proportionally allocated to each selected hospital based on the number of total medical waste handlers they had. To determine the total number of participants from each selected health facility, a computer-generated simple random sampling technique was used.
Sampling Procedure
Sampling procedure is shown in Figure 1.
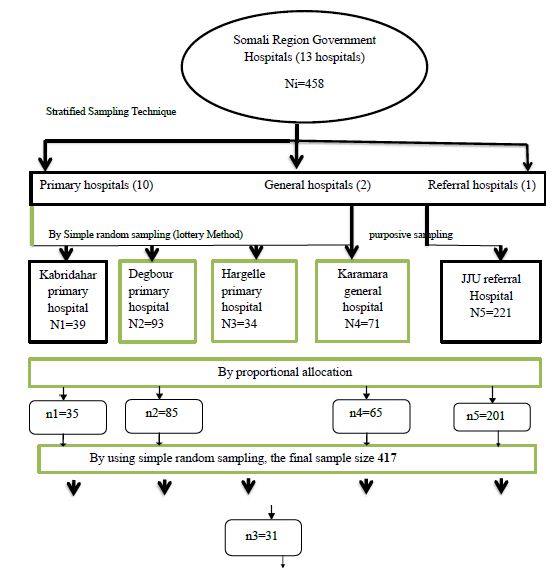
Figure 1: Schematic presentation of sampling procedure of waste handlers at selected government hospitals in Somali Region, Ethiopia 2021.
Data Collection Tool and Procedure
The data was collected by the interviewer through a structured questionnaire. A structured questionnaire was developed by the principal investigator after reviewing WHO, FMOH infection prevention guidelines, and different literature with modifications based on research objectives. Prior to the actual data collection, the questionnaire was adjusted and corrected based on the pre-test result, and the final questionnaire was translated into Somali and then back to English to ensure its consistency. Finally, one environmental health scientist and two public health professionals conducted face-to-face interviews to collect the data using the Somali version questionnaire.
Variables
Dependent Variable
Safety practice (Safe/Unsafe)
Independent Variables
Socio-Demographic and Economic Factor
- sex
- Age
- Marital status
- Educational Status
- monthly income
Work Related Factors
- working hours per day,
- working departments/units,
- Work experience
Waste handlers risk perceptions
- Attitudes
- Knowledge about safety practice
Organizational factors
- Training,
- Supportive supervision,
- Availability of equipment’
Data Quality Control
To maintain the quality of the data, adequate training was given to data collectors and supervisors for three days on the techniques of data collection. The questionnaire was pre-tested by taking 5% of the study sample at one of the selected hospitals. The collected data was checked for completeness and consistency. Each questionnaire was coded and cleaned. Then the coded and cleaned data was entered into Epi-data version 3.1 software.
Operational Definition
Safety practice is the practice of using personal protective equipment’s such as (heavy duty glove, gown, boots and masks), hygiene, vaccination for HBV and appropriate waste segregation with separated bins to prevent oneself from disease causing microorganisms.
Waste handlers are cleaners that are involved in the handling of medical wastes.
Safe Practice
Respondents who scored more than mean of correct answer for seven practice questions with yes or no answer were classified as safe practiced [28].
Good Knowledge
Medical waste handlers who correctly responded4 and above out of the 7 knowledge-based questions were considered as having good knowledge [30].
Good Attitude
Attitude questions responses were indicated with the three-point Likert type scale of measurement as “ Disagree”, “neutral”, and Agree” and numerical values of 1,2 and 3 respectively were given. The mean score was determined after computing attitude assessing questions[26].
Good Supplies Availability
The presence of supplies like personal protective equipment’s (heavy duty glove, gown, masks and boots), three colour coded bins and hand washing facilities like soap and anti-septic hand rub.
Trained
Waste handlers who got any types of training concerning safe waste handling.
Data Processing and Analysis
The completeness of the data was checked manually and coded accordingly. The coded and cleaned data was entered into the computer using EpiData version 3.1 and exported to SPSS version 20. After completion of data entry, it was cleaned before analysis. A description of frequency, mean, proportion, and SD was done for the first objective. Binary logistic regression was employed to identify factors associated with safety practices. Initially, bivariate analysis was done, and variables with a p-value below 0.25 were identified as candidates for multivariate analysis. Then multi-variable analysis was done, and an adjusted odd ration was computed and interpreted. A p-value less than 0.05 is the cut-off point for determining the significance of the association. The results of the study were presented in text, tables, and graphs. Multi-collinearity was checked by the variance inflation factor (VIF), and the goodness of model fit was checked by the Hosmer-Lemeshow test.
Ethical Consideration
An ethical clearance letter was acquired from the ethical review board of the College of Medicine and Health Sciences, Jigjiga University, and a permission letter was secured from the regional health bureau and delivered to the public hospital administrations. Written informed consent was secured from each participant. The confidentiality of the information and the privacy of the study participants were maintained. The participation was voluntary, and they had the right to withdraw from the interview if it was not comfortable for them.
Dissemination and Utilization of Finding
The findings will be disseminated to Jigjiga University, the School of Graduate Studies, the School of Public Health, the Department of Epidemiology, the Somali Regional Health Bureau, and those selected hospitals through presentations and printed materials.
Results
Socio–demographic Characteristics and Work Related Factors of Respondents
From the total sample of 417 included in the study. 401 waste handlers were interviewed, with a response rate of 96.2%. The mean age of the study participants was 32.1 (SD 6.1) years, and all respondents were females (100%). About 118 (29.4%) of them were in the age group 31–35 years. Married hospital waste handlers were 220 (54.9%), while 251 (66.1%) were illiterate. The majority of them, 255 (63.6%), had greater than 5 years of working experience, and 235 (58.6%) of them had an income level of 2000 birr per month. Two hundred eighty-four (70.8%) waste handlers were working their job in regular time (8 hours only). As compared with the other departments, the highest numbers of participants (133, 33.2%) and 69, 17.2%) were from the emergency and surgical wards, respectively (Table 2).
Table 2: Socio demographic characteristics and work related factors of medical waste handlers in selected public hospitals in Somali region, Eastern Ethiopia, August, 2021(N=401).
|
Sn |
Variables | Category | Frequency |
Percentage (%) |
| 1 | Age | ≤25yrs |
56 |
14% |
| 26-30yrs |
107 |
26.7% |
||
| 31-35yrs |
118 |
29.4% |
||
| >35yrs |
120 |
29.9% |
||
| 2 | Marital status | Married |
265 |
66.1% |
| Single |
97 |
24.2% |
||
| Widowed |
17 |
4.2% |
||
| Divorced |
22 |
5.5% |
||
| 3 | Religion | Muslim |
296 |
73.8% |
| Orthodox |
49 |
12.2% |
||
| Protestant |
24 |
6% |
||
| Other |
32 |
8% |
||
| 4 | Education level | Illiterate |
251 |
62.6% |
| Primary(1-8) |
108 |
26.9% |
||
| Secondary(9-12) |
28 |
7% |
||
| Diploma & above |
14 |
3.5% |
||
| 5 | Service year | ≤5yrs |
146 |
36.4% |
| >5yrs |
255 |
63.6% |
||
| 6 | Monthly Income | ≤2000ETB |
235 |
58.6% |
| >2000ETB |
166 |
41.4% |
||
| 7 | Working hours per day | ≤8hrs |
284 |
70.8% |
| >8hrs |
117 |
29.2% |
||
| 8 | Working departments | Outpatient |
50 |
12.5% |
| Emergency |
133 |
33.2% |
||
| Laboratory |
33 |
8.2% |
||
| Surgical |
69 |
17.2% |
||
| Medical |
33 |
8.2% |
||
| Pediatric |
46 |
11.5% |
||
| Gyne & Obs |
28 |
7% |
||
| Other |
9 |
2.2% |
Proportion of Safety Practice
The proportion of safe practice in this study was found to be153 (38.2%) with 95% CI: 33.2, 43.1) (Figure 2).
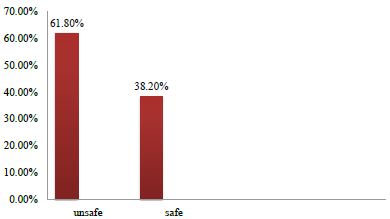
Figure 2: The prevalence of safety practice among medical waste handlers at selected government hospitals in, Somali Region, Eastern Ethiopia, August 2021. Safety Practice of health care waste handlers.
About 108 (25.9%) of them wore at least four and above four types of personal protective equipment during the handling of health care waste. where 44 (11% of them) washed their hands at all the selected critical times of hand washing. Two hundred (49.9%) of the waste handlers were immunized for HBV. Among the medical waste handlers who participated in the study, 63.6% separated hazardous and non-hazardous waste during the collection and transportation of hospital waste to the disposal site. Nearly 90% of them used a separated, color-coded bin system during collection. But 265 (66.1%) were mixing waste stored at separate bins during transportation of hospital waste to the disposal site. Only 112 (27.9%) of them asked for decontamination of hazardous waste before disposal.
Among the respondents, 384 (95.8%) had ever had a needle stick injury. 127 (30.1%) of the respondents reported that they use antiseptic hand rub after handling medical waste, and 397 (99%) of the respondents reported that they hadn’t ever received post-exposure prophylaxis for HIV/AIDS. About 17 (4.2%) of the waste handlers had the intention to move medical waste using trolleys in the future.
Only 51 (12.7%) medical waste handlers of the study participants reported that they had been exposed to the blood or other body fluids of patients through contact; 383 (95.5%) of these waste handlers reported that they had ever faced a sharp injury in the last year. Finally, among all waste handlers asked, 153 (38.2%) of them were practicing safely, and the rest (248, 61.8%) were practicing unsafely (Table 3).
Table 3: The prevalence of safety practice among waste handlers in selected public hospitals of Somali region, eastern Ethiopia, August 2021.
|
Sn |
Safety practice | Category | Frequency |
Percentage (%) |
|||
| 1 | Wore at least four and above four types of personal protective equipment’s |
Yes |
108 |
25.9% |
|||
|
No |
293 |
73.1% |
|||||
| 2 | Hand washing at five critical time |
Yes |
44 |
11% |
|||
|
No |
357 |
89% |
|||||
| 3 | Immunized for HBV |
Yes |
200 |
49.9% |
|||
|
No |
201 |
50.1% |
|||||
| 4 | use colour coded bine system |
Yes |
360 |
89.8% |
|||
|
No |
41 |
10.2% |
|||||
| 5 | separate hazardous and non-hazardous waste |
Yes |
255 |
63.6% |
|||
|
No |
146 |
36.4% |
|||||
| 6 | Ask decontamination of waste before disposal |
Yes |
112 |
27.9% |
|||
|
No |
289 |
72.1% |
|||||
| 7 | Mix waste stored in a separate bins during transportation |
Yes |
265 |
66.1% |
|||
|
No |
136 |
33.9% |
|||||
| 8 | Ever had needle stick injury |
Yes |
17 |
4.2% |
|||
|
No |
384 |
95.8% |
|||||
| 9 | Have you faced a sharp |
Yes |
18 |
4.5% |
|||
| Injury in the last one year |
No |
383 | 95.5% | ||||
| 10 | Have you ever exposed to blood or other body fluids of patients through contact |
Yes |
51 |
12.7% |
|||
| No | 350 |
87.3% |
|||||
| 11 | Ever got post exposure prophylaxis for HIV/ADIS |
Yes |
4 | 1% | |||
| No | 397 |
99% |
|||||
| 12 | Move medical waste using trolley |
Yes |
17 | 4.2% | |||
| No | 384 |
95.8% |
|||||
| 13 | Do you use antiseptic hand rub |
Yes |
127 | 30.1% | |||
| No | 274 |
64.9% |
|||||
| Safety practice |
Safe practice |
153 | 38.2% | ||||
| Unsafe practice | 248 |
61.8% |
|||||
Knowledge of the Respondents Regarding Safety Practice
Concerning knowledge of the study participants 244(60.9%) of the respondents were having knowledge about safety practice (Figure 3).
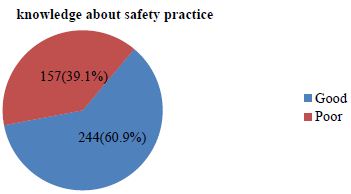
Figure 3: Proportion of knowledge on safety practice of the study participants at selected public hospitals in Somali region, eastern Ethiopia, August 2021.
Knowledge of the Respondents Regarding Safety Practice
Out of 401 respondents, seven knowledge questions with a yes or no answer were asked to assess their knowledge about safety practices. 289 (72.1%) of the respondents knew they were at risk of hospital-associated infections. Nearly 70% of them knew that washing hands with plain soap and water inhibits resident flora, and 68.2% of them knew that gloves should be used not only in anticipation of blood or body fluid exposure. The majority of the respondents (274, or 68.3%) knew being vaccinated for the HBV vaccine was a means of preventing infection. Nearly 60% of them had knowledge of post-exposure prophylaxis. Nearly 61% of study participants had good knowledge (Table 4).
Table 4: Safety practice Knowledge related item responses of the study at selected public hospital waste handlers in Somali region, Ethiopia, August 2021.
|
Sn |
Knowledge | Category | Frequency |
Percentage (%) |
| 1 | Are hospital waste handlers are at risk of infections |
Yes |
289 | 72.1% |
| No | 112 |
27.9% |
||
| 2 | Washing hand with plain soap and water inhibit resident flora |
Yes |
277 | 69.1% |
| No | 124 |
30.9% |
||
| 3 | Gloves should be worn if blood or body fluid exposure is anticipated |
Yes |
276 | 68.2% |
| No | 125 |
31.8% |
||
| 4 | Washing your hands with soap and alcohol decrease transmission of infectious disease |
Yes |
284 | 70.8% |
| No | 117 |
29.2% |
||
| 5 | Immunized for HBV is a means of prevention from infections |
Yes |
274 | 68.3% |
| No | 127 |
31.7% |
||
| 6 | Getting PEP with in 72hr of exposure is a means of treatment |
Yes |
240 | 59.9% |
| No | 161 |
40.1% |
||
| 7 | Have you ever heard about safety practice |
Yes |
293 | 73.1% |
| No | 108 |
26.9% |
||
| Knowledge about safety practice |
Good |
244 | 60.9% | |
| Poor | 157 |
39.1% |
Attitude of Health Care Waste Handlers about Safety Practice
A total of 401 respondents were asked five attitude questions with Likert-type scale options ranging from “disagree to agree to assess their attitude about safety practices. The majority of them, 195 (48.6%), agreed that washing hands with soap or alcohol-based antiseptics decreased the risk of transmission of hospital-acquired infections. Nearly 56.1% of them disagreed that gloves provide complete protection against acquiring or transmitting hospital-acquired infections, and 252 (62.8%) disagreed that hand washing is unnecessary when gloves are worn. About 245 (61.1%) of the study participants disagreed that frequent hand washing damages the skin and causes cracking, dryness, irritation, and dermatitis. A total of 235 (58.6%) of the study participants disagreed that hospital waste handlers have a very low risk of acquiring infection from improperly disposed hospital waste. More than 50% (209) of the study participants had a positive attitude towards. Safety practices (Table 5).
Table 5: Attitude about safety practice of public hospital waste handlers in Somali region, Ethiopia, August 2021.
|
Sn |
Attitude | Category | Frequency |
Percentage (%) |
| 1 | Glove provides complete protection against acquiring /transmitting infections | Disagree |
225 |
56.1% |
|
Neutral |
46 |
11.5% |
||
| Agree |
130 |
32.4% | ||
|
2 |
Washing hands with soap or alcohol based antiseptic decrease the risk of transmission of hospital acquired infections |
Disagree |
161 |
40.2% |
| Neutral |
45 |
11.2% | ||
|
Agree |
195 |
48.6% |
||
| 3 | Hand washing is unnecessary when gloves are worn | Disagree |
252 |
62.8% |
|
Neutral |
22 |
5.5% |
||
| Agree |
127 |
31.7% | ||
|
4 |
You have a very low risk of acquiring infection from improperly disposed hospital wastes |
Disagree |
235 |
58.6% |
| Neutral |
106 |
26.4% | ||
|
Agree |
60 |
15% |
||
| 5 | Frequent hand washing damages skin and causes cracking, dryness, irritation and dermatitis | Disagree |
245 |
61.1% |
|
Neutral |
58 |
14.5% |
||
| Agree |
98 |
24.4% | ||
|
Attitude |
Positive attitude |
209 |
52.1% |
|
| Negative attitude |
192 |
47.9% |
Organizational Factors Affecting Safety Practice of Hospital Waste Handlers
Out of 401 waste handlers interviewed, 185 (46.2%) had gained any type of training about safety practices, 177 (44.1%) were supervised regularly by the organization, and 39 (9.7%) had both training and regular supportive supervision (Figure 4).

Figure 4: Organizational factors affecting safety practice of hospital waste handlers in Somali region, Eastern, Ethiopia, August 2021.
Availability of Personal Protective Equipment’s among Waste Handlers
A total of 401 respondents were interviewed to check the availability of personal protective equipment in the health facility. From the interviewed respondents, almost 251 (95%) of them responded that gloves were available, while 376 (93.8%) of them responded that gowns were available. Almost 62.6% of them also responded that masks were available. Nearly 14.7% of them answered that caps were available, and 24 (6%) of them responded that goggles were available at the facilities. A few respondents (2.5%) responded that boots were available at the hospitals during the data collection period (Figure 5).
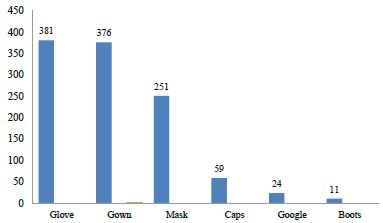
Figure 5: Availability of personal protective equipment’s among waste handler in selected government hospitals in Somali region, Eastern, Ethiopia, August 2021.
Factors Associated with Safety Practice
Bivariate Analysis of Socio-demographic Factors Relating with Safety Practice
In this study, there is a significant association between respondent’s age and safety practices. Waste handlers whose age is between 31 and 35 years were 78% times (COR=0.22, 95% CI=0.13, 0.379; P=0.0001) less likely to be safe practiced compared to waste handlers whose age is included in other age categories. Also, health care waste handlers whose age is between 26 and 30 were 87% times (COR=0.13, 95% CI=0.72, 0.24; P=0.0001) less likely to be safe practiced compared to waste handlers whose age is included in other age categories.
The service year also showed a significant association with safety practices. Waste handlers who have worked less than or equal to 5 years were 34% (COR=0.66, 95% CI 0.44, 0.998; P=0.049) times less likely to be safe practiced compared to waste handlers who have worked greater than 5 years of working experience (Table 6).
Table 6: Sociodemographic and work related factors associated with safety practice using bivariate logistic regression at public hospitals in Somali Region, Eastern Ethiopia, August 2021.
|
Variable |
Category | Safety Practice | COR (95% CI) | P-value | |||||
| Safe | Unsafe | ||||||||
| Age In Years | ≤25yrs |
4 |
52 | 0.033(0.11-0.098) | 0.0001* | ||||
|
26-30yrs |
25 | 82 | 0.131(0.72-0.237) |
0.0001* |
|||||
| 31-35yrs |
40 |
78 | 0.22(0.13-0.379) | 0.0001* | |||||
|
>35yrs |
84 | 36 | 1.00 | ||||||
| Marital status | Married |
102 |
163 | 0.52 (0.22-1.25) | 0.145 | ||||
|
Single |
32 | 65 | 0.41(0.16-1.1) |
0.06 |
|||||
| Widowed |
7 |
10 | 0.58(0.16-2.1) | 0.41 | |||||
|
Divorced |
12 | 10 | 1.00 | ||||||
| Education | Illiterate |
84 |
167 | 1.84(0.5-6.79) | 0.36 | ||||
|
Primary(1-8) |
54 | 54 | 3.67(0.97-13.88) |
0.056 |
|||||
| Secondary(9-12) |
12 |
16 | 2.75(0.63-12.1) | 0.18 | |||||
|
Diploma & above |
3 | 11 | 1.00 | ||||||
| Monthly income | ≤2000ETB |
97 |
138 | 1.38(0.1-2.1) | 0.126 | ||||
|
>2000ETB |
56 | 110 | 1.00 | ||||||
| Service year | ≤5yrs |
55 |
114 | 0.66(0.44-0.998) | 0.049* | ||||
|
>5yrs |
98 | 134 |
1.00 |
||||||
| Working hours | ≤8hrs |
103 |
163 | 1.1(0.69-1.62) | 0.81 | ||||
|
>8hrs |
50 | 84 | 1.00 | ||||||
| Working unit | Outpatient |
15 |
35 | 0.54(0.21-0.81) | 0.398 | ||||
|
Emergency |
52 | 81 | 0.8(0.44-2.1) |
0.75 |
|||||
| Laboratory |
7 |
26 | 0.34(0.17-0.86) | 0.17 | |||||
|
Surgical |
28 | 41 | 0.85(0.65-3.1) |
0.83 |
|||||
| Medical |
13 |
20 | 0.81(0.67-2.94) | 0.79 | |||||
|
Pediatric |
21 | 25 | 1.1(0.5-2.93) |
0.95 |
|||||
| Gyne & Obs |
13 |
15 | 1.1(0.43-5.64) | 0.92 | |||||
|
Others |
4 | 5 | 1.00 | ||||||
Bivariate Analysis of Associated Variables Relating with Safety Practice
In this study, there was a statistically significant association between knowledge of waste handlers and safety practice. Waste handlers who had good knowledge were 4.3 times safer than those who had poor knowledge (COR=4.3, 95% CI 2.75, 6.75; P=0.0001).
Regarding attitude, there is also a significant association between attitude and safety practice. Respondents who had a positive attitude were 1.66 times (COR=1.66, 95% CI 1.1–2.6; P=0.024) more likely to be safe practitioners compared to respondents who had a negative attitude toward safety practices.
Whereas availability of materials is associated with safety practice, health care waste handlers who had availability of safety materials were 7.1 times (COR=7.1, 95% CI 4.4, 11.46; P=0.0001) more likely to be safe practitioners than those who had a shortage of safety materials (Table 7).
Table 7: Associated variables about safety practice of waste handlers using bivariate logistic regression at government hospitals in Somali Region, Eastern Ethiopia, August 2021.
|
Safety practice |
COR (95% CI) | P-value | |||
| Variable | Categories | Safe | Unsafe | ||
| Knowledge | Good | 116 | 104 | 4.3(2.72-6.75) | 0.0001* |
| Poor | 37 | 144 | 1.00 | ||
| Attitude | Positive | 113 | 156 | 1.67 (1.1,2.6) | 0.024* |
| Negative | 40 | 92 | 1.00 | ||
| Training
|
Trained | 83 | 111 | 1.46(0.976-2.19) | 0.065 |
| Not trained | 70 | 137 | 1.00 | ||
| Availability of materials
|
Good | 125 | 96 | 7.1(4.4-11.46) | 0.0001* |
| Poor | 28 | 152 | 1.00 | ||
Multivariate Logistic Regression Analysis of Safety Practice among Hospital Waste Handlers in Somali Region, Ethiopia, August 2021
Bivariate logistic regression was done, and variables with p-values <0.25 were selected for the multiple logistic regression analysis, and multicollinearity was checked by looking at the VIF (variance inflation factor) in the linear regression model. In the bivariate analysis, it was found from socio-demographic variables: age group, had a statistically significant association with safety practice (p-value <0.05). From work-related variables, service year was significantly associated with safety practices. Also, the results revealed in the bivariate analysis of the variables, including knowledge, attitude, and availability of supplies, were significantly associated with safety practice.
In multivariate logistic regression, the confounding effect of one variable over the other variables was adjusted. Based on this, age category, knowledge of the participants, attitude, and availability of safety supplies were significantly associated with safety practice at a P-value of <0.05 (Table 8).
The odds of respondents with a positive attitude were 5.4 times more likely to be safe practiced compared to respondents who had a negative attitude toward safety practice (AOR: 5.4; 95% CI: 2.53, 11.47; P=0.05). The odds of waste handlers with good knowledge were 7.21 times safer than those who had poor knowledge (AOR=7.21, 95% CI 3.7–14; P=0.05). The odds of respondents who had availability of safety materials were 9.3 times higher than those who had a shortage of safety materials (AOR=9.3, 95% CI 5, 17.2); p=0.05. The odds of waste handlers with an age category between 31 and 35 years were 81.1% less likely to be safe practitioners than those whose age group was greater than 35 years (AOR=0.189, 95% CI: 0.094, 0.38; P=0.05). The results of the final multiple logistic regression models are found in the Table 8.
Table 8: Result of multiple logistic regression analysis on safety practice among hospital waste handlers in Somali region, Eastern Ethiopia, August, 2021.
|
Variable |
Category | Safety practice | COR (95% CI) | AOR (95%CI) | |
| Safe |
Unsafe |
||||
| Age in years | ≤25yrs |
4 |
52 | 0.03(0.11-0.098) | 0.047(0.014-0.16)* |
|
26-30yrs |
25 | 82 | 0.13(0.72-0.237) |
0.146(0.065-0.33)* |
|
| 31-35yrs |
40 |
78 | 0.22(0.13-0.379) | 0.189(0.094-0.38)* | |
|
>35yrs |
84 | 36 | 1.00 |
1.00 |
|
| Service year | ≤5years |
55 |
114 | 0.66(0.44-0.998) | 1.2(0.62-2.34) |
|
>5years |
98 | 134 | 1.00 |
1.00 |
|
| Knowledge | Good |
116 |
104 | 4.3(2.72-6.75) | 7.21(3.7-14)** |
|
Poor |
37 | 144 | 1.00 |
1.00 |
|
| Availability of materials | Good |
125 |
96 | 7.1(4.4-11.46) | 9.3(5-17.2)** |
|
Poor |
28 | 152 | 1.00 |
1.00 |
|
| Attitude | Positive |
113 |
156 | 1.66 (1.1,2.6) | 5.4(2.53-11.47)** |
|
Negative |
40 | 92 | 1.00 |
1.00 |
|
Discussion
The overall current prevalence of safety practice among hospital waste handlers in this study was 38.2% (95% CI: 33.2, 43.1). The finding was higher as compared with the study done in Shiraz, Iran [31]. This difference might be due to the difference in the study design, setting, and time of the study, as well as the implementation of different reforms by the federal ministry of health at hospitals like infection prevention and patient safety, which were promoting the safety practices of hospital waste handlers.
The prevalence of this study was lower than the prevalence of safety practice among medical waste handlers in Addis Ababa town and with research done in Gonder town among waste collectors, 44.1% (95% CI: 37.3-51) and 45% (95% CI: 40.3-49.4), respectively [26,32]. This difference might be due to the difference in the study setting and time, as well as the implementation of hospital infection prevention protocols. The number of participants with good safety practices reported in the finding was lower than the study done at KwaZulu-Natal (50%) [33]. This difference may be due to the study setting and time. Also, the finding was lower than the findings from Cameroon, in which 100% of the medical waste handlers used all the appropriate protective gear [34]. This difference might be due to the study setting, the difference in knowledge of hospital waste handlers, and the attention given to safety by the governing body. The finding was also lower than the finding from Debra Markos (80%) [35]. This difference may be due to the lower sample size they used.
In principle, all medical waste handlers should properly utilize personal protective equipment during the handling of medical wastes [5]. However, in this study, only 25.9% of medical waste handlers properly utilized personal protective equipment. The result was better than the study done in tertiary care health facilities at Shiraz Iran hospitals, the metropolitan city of Pakistan, and Adis Ababa government hospitals, in which 15%, 22.8%, and 25.2% of waste handlers utilized personal protective equipment properly[26,31,36]. This difference might be due to the implementation of different initiatives by the ministry of health like CASH, infection prevention, and patient safety, as well as an increase in knowledge of hospital-acquired infections among medical waste handlers.
In this study, attitude was shown to be an independent predictor of safety practice among medical waste handlers. The odds of safety practice among waste handlers with a positive attitude were 5.4 (AOR: 5.4; 95% CI: 2.53, 11.47; P=0.05) times higher than those who had a negative attitude. This was slightly higher with the study done in Adisababa [26] which showed that health care waste handlers with favorable attitudes had 4.78 (AOR=4.78, 95% CI 1.64, 13.9) higher safe practices compared to respondents with unfavorable conditions. The difference might be due to the setting in which the study was conducted, the lower sample size they used, and the difference in providing pre-service and in-service supervision to increase their intention for safe medical waste handling.
The odds of safety practice among waste handlers with good knowledge were 7.21 (AOR=7.21, 95% CI 3.7–14; p=0.05) times higher than those who had poor knowledge. This was slightly higher with the study done by DebreMarkos and Adisababa [32,36], which showed that waste handlers with good knowledge practiced safety more than those with poor knowledge. The findings of this study were inconsistent with those of a study done in South India [8]. The difference might be due to the difference in study settings, which were undertaken at a tertiary care hospital, and the sampling techniques they used, which were purposive sampling, which may introduce selection bias, and that the knowledge acquired may not necessarily be translated into practice.
The odds of safety practice among waste handlers with adequate supplies were 9.3 (AOR=9.3, 95% CI 5, 17.2); p=0.05 times higher than those with a lack of supplies. This finding was higher in studies conducted in DebreMarkos and Adisababa [26,37], in which those respondents with adequate supplies had good safety practices. This difference might be due to the attention given by the state health bureau and hospital administration to the fulfillment of the required supplies and inputs. In this study, the age group has shown a significant association with safety practices among medical waste handlers. The odds of waste handlers with an age group between 31 and 35 years were 81.1% (AOR=0.189, 95% CI: 0.094, 0.38; P=0.05) times less likely to be safe practitioners than those whose age group is greater than 35 years. The findings were lower with the study done in Bahardar [38], which showed that respondents in the age group 30-35 years had 4.1 (AOR=4.1, 95% CI: 1.27, 13.4) times more safe practices compared to their counterparts. The difference might be due to the lower sample proportion they used.
Limitation of the Study
The study was conducted only in government hospitals, which do not represent private hospitals. Moreover, since this study was a cross-sectional study, it may not allow for the establishment of a causal link between the factors associated with safety practices.
Conclusion
The result of this study showed that the level of safety practice was low compared to the national and international standards among hospital waste handlers in relation to waste handling and safety, which may increase the chance of getting infected with hospital-acquired infections and occupational infections. So reducing those problems through adequate professional support and supervision should be in place to increase their knowledge about safety precautions, and availing of safety supplies should be implemented to increase adherence to safety practices among hospital waste handlers. This study will also help hospital administrators take appropriate interventions, including providing important PPE, motivating the worker to utilize it properly, and planning to improve the safety practices of medical waste handlers working in public hospitals in the Somali Region.
References
- Cointreau S (2018) Occupational and environmental health issues of solid waste management: special emphasis on middle-and lower-income countries. Urban Papers. 2006.
- Xiao F. A novel multi-criteria decision making method for assessing health-care waste treatment technologies based on D numbers. Engineering Applications of Artificial Intelligence 71: 216-25.
- Prüss-Üstün A, Giroult E, Rushbrook P, Organization WH (2019) Safe management of wastes from health-care activities: World Health Organization;
- Cook E, Velis C, Woolridge A, Stapp P, Edmondson S (2020) Medical and healthcare waste generation, storage, treatment and disposal: A systematic review of risks to occupational and public health.
- Alemayehu T, Worku A, Assefa N (2016) Medical waste collectors in eastern Ethiopia are exposed to high sharp injury and blood and body fluids contamination. Prev Inf Cntrl 2: 2.
- Fatusi A, Moyosola A. Bamidele, Abimbola O. Sowande, Jennifer Pearson (2016) Infection Prevention and Control and Health Care Waste Management for Waste Handlers. Aidsfree Nigeria Training Manual. 46.
- Geberemariyam BS, Donka GM, Wordofa B (2018) Assessment of knowledge and practices of healthcare workers towards infection prevention and associated factors in healthcare facilities of West Arsi District, Southeast Ethiopia: a facility-based cross-sectional study. Archives of Public Health 76: 1-11. [crossref]
- WHO: . Aide memoire for a national strategy for safe and appropriate use of injections. Department of Blood Safety and ClinicalTechnology. Geneva; 2003.
- Heldal KK, Thorn J, Djupesland P, Wouters I, et al. (2013) Upper airway inflammation in waste handlers exposed to bioaerosols. Occup Environ Med 60: 444-450. [crossref]
- Yang CY, Chuang HY, Tsai SS, Wu TN, et al. (2011) Adverse health effects among household waste collectors in Taiwan. Environ Res 85: 195-9. [crossref]
- Dounias G RG (2016) Prevalence of hepatitis A virus infection among municipal solid-waste workers. Int J Clin Pract 60: 1432-6.
- Luksamijarulkul P, Charupoonphol P (2018) Risk behaviours, occupational risk and seroprevalence of hepatitis B and A infections among public cleansing workers of Bangkok Metropolis. Hepat Mon 8: : 35-40. .
- Kuusisto S, Rantio T, Priha E, Tuhkanen T (2017) PCB contaminated dust on indoor surfaces – health risks and acceptable surface concentrations in residential and occupational settings. Chemosphere 67: 194-201. [crossref]
- PPFM K (2012) Effectiveness of interventions to reduce workload in refuse collectors. Coronel Institute for Occupational and Environmental Health, AmCOGG: Center for Research into Health and Health Care 51: 79-87.
- Alamgir H, Cvitkovich Y, Astrakianakis G, Yu S, Yassi A (2008) Needlestick and other potential blood and body fluid exposures among health care workers in British Columbia, Canada. American Journal of Infection Control 2008;36: 12-21. [crossref]
- Rachiotis G, Papagiannis D, Markas D, Thanasias E, Dounias G, et al. (2012) Hepatitis B virus infection and waste collection: prevalence, risk factors, and infection pathway. American Journal of Industrial Medicine 55: 650-5. [crossref]
- Mote BN, Kadam SB, Kalaskar SK, Thakare BS, Adhav AS, et al. (2016) Occupational and environmental health hazards (physical and mental) among rag-pickers in Mumbai slums: A cross-sectional study. Sci J Pub Health 4: 1-10.
- Jayakrishnan T, Jeeja MC, Bhaskar R (2013) Occupational health problems of municipal solid waste management workers in India. Int J Env Health Eng 2(1): 42.
- Shiferaw Y, Abebe T, Mihret A (2011) Hepatitis B virus infection among medical waste handlers in Addis Ababa, Ethiopia. BMC Research Notes 4: 1-7. [crossref]
- Soliman SM, Ahmed AI (2007) Overview of biomedical waste management in selected Governorates in Egypt: A pilot study. Waste Management 27: 1920-3. [crossref]
- Tadesse ML, Kumie A (2014) Healthcare waste generation and management practice in government health centers of Addis Ababa, Ethiopia. BMC Public Health 14: 1-9. [crossref]
- Ruoyan G, Huijuan L, Chengchao Z, Jiangjiang H, et al. (2010) Investigation of health care waste management in Binzhou District, China. Waste Manag Res 30: 246-50. [crossref]
- Blenkharn J, Odd C (2008) Sharps injuries in healthcare waste handlers. Annals of Occupational Hygiene 52: 281-6. [crossref]
- Alamgir H, Cvitkovich Y, Astrakianakis G, Yu S, Yassi A (2008) Needlestick and other potential blood and body fluid exposures among health care workers in British Columbia, Canada. American Journal of Infection Control 36: 12-21. [crossref]
- Haylamicheal ID, Yirsaw BD, Zegeye HA (2011) Assessing the management of healthcare waste in Hawassa city, Ethiopia. Waste Manag Res 29: 854-62. [crossref]
- Tekle T, Abegaz T, Wondimagne A, Abdo ZA (2021) Safety Practice and Associated Factors Among Waste Handlers in Governmental Hospitals in Addis Ababa, Ethiopia. European Journal of Preventive Medicine 9: 107-13.
- Muluken A, Haimanot G, Mesafint M (2014) Healthcare waste management practices among healthcare workers in healthcare facilities of Gondar town, Northwest Ethiopia.
- Mesfin A, Worku W, Gizaw Z (2013) Assessment of Health Care Waste Segregation Practice and Associated Factors of Health Care Workers in Gondar University Hospital, North West Ethiopia.
- Gulilat K, Tiruneh G (2014) Assessment of knowledge, attitude and practice of health care workers on infection prevention in health institution Bahir Dar city administration. Sci J Public Health 2: 384-3.
- Mariam FAaZAA (2018) Medical Waste Handling Practice and Associated Factors among Cleaners in Public Hospitals under Addis Ababa Health Bureau, Addis Ababa, Ethiopia.
- Lakbala P, Azar FE, Kamali H (2012) Needlestick and sharps injuries among housekeeping workers in hospitals of Shiraz, Iran. BMC Research Notes 5: 1-5. [crossref]
- Mesfin A, Gizaw Z (2013) Assessment of Health Care Waste Segregation Practice and Associated Factors of Health Care Workers in Gondar University Hospital, North West Ethiopia, 2013.
- Anozie OB, Lawani LO, Eze JN, Mamah EJ, Onoh RC, et al. (2017) Knowledge, attitude and practice of healthcare managers to medical waste management and occupational safety practices: Findings from Southeast Nigeria. Journal of Clinical and Diagnostic Research: JCDR 11: IC01. [crossref]
- Gillian Dzekashu L AJ, Mbacham WF (2016) Medical waste management and disposal practices of health facilities in kumbo east and kumbo west health districts. J Environ Health Sci 2: 1-9.
- Deress T, Jemal M, Girma M, Adane K (2019) Knowledge, attitude, and practice of waste handlers about medical waste management in Debre Markos town healthcare facilities, northwest Ethiopia. BMC Research Notes 12: 1-7.
- Kumar R, Samrongthong R, Shaikh BT (2013) Knowledge, attitude and practices of health staff regarding infectious waste handling of tertiary care health facilities at metropolitan city of Pakistan. J Ayub Med Coll Abbottabad 25: 109-12. [crossref]
- Patwary MA, O’Hare WT, Sarker MH (2011) Assessment of occupational and environmental safety associated with medical waste disposal in developing countries: a qualitative approach. Safety Science 49: 1200-7.
- Lulie Walle EA (2017) Safety Practice Among Medical Waste Collectors in souther Ethiopia Journal of Prevention & Infection Control 2: 7