Abstract
Introduction: The symptom complex caused by vulvovaginal atrophy negatively impacts postmenopausal women’s quality of life. Several studies have already conferred a solid base to the rationale for vulvovaginal restructuring and control of atrophy-related symptoms thanks to a few sessions of PN-HPT® injected in the vulvar skin dermis and mucosal lamina propria in combination with hyaluronic acid.
Methods: A real-world cohort of 60 ambulatory women spontaneously seeking help to alleviate their menopausal vulvovaginal atrophy symptoms. Treatment: a five-session cycle of vulvar injections with a Class-III CE-mark medical device (NewGyn®, Mastelli, Sanremo, Italy)—PN-HPT® (10 mg per mL), HA (10 mg per mL), mannitol (220 micromoles per mL). Assessments: vaginal dryness, irritation, dyspareunia, itching, tenderness and tingling, blood losses, urgency, dysuria, recurrent urinary infections; scoring with 10-cm visual analogue scales (VAS, 0=no symptom, 10=unbearable symptom).
Results: The typical VVA symptoms that were more severe at baseline improved markedly over the 90-day follow-up period: –63.5% for vaginal dryness, –57.7% for irritation, –59.4% for dyspareunia,–68.8% for itching, and –70.0% for tenderness/tingling. The occasional mild local pain and irritation at the injection site, expected and known in the previous PN-HPT® literature, were of no clinical significance and rapidly transitory.
Conclusions: Once again, the outcomes of this real-world cohort study suggest that the PN-HPT® bio-restructuring properties in connective tissues and the documented synergy between PN-HPT® and hyaluronic acid translate into a fine control of vulvovaginal atrophy symptoms.
Keywords
Hyaluronic acid, PN-HPT®, Polynucleotides Highly Purified Technology, Vulvovaginal atrophy, Vulvar skin quality
Introduction
Embryologically, the female genital and lower urinary tract share a common origin, with the trigone, vulvar vestibule, upper vagina, and urethra and bladder deriving from the primitive urogenital sinus tissue rich in estrogen receptors [1]. Unfortunately, only a little circulating oestradiol survives in the postmenopausal woman—less than 30 pg/mL indirectly originating from adrenal androgens after conversion via estrone in adipose tissue [2,3].
The atrophic vulvovaginal symptoms and signs, experienced by middle-aged women and often extended to the bladder and urethral areas, do not subside without treatment. The resulting severe burden on the woman’s quality of life is a troubling perspective, both socially and individually, since Western women can reasonably expect to live almost 40% of their existence in the menopausal condition [4].
The labia, clitoris, vestibule, introitus, and vagina, but also the urethra and bladder, change in up to 50% of menopausal women. The collective label of Genitourinary Syndrome of Menopause (GSM) summarises the related symptom cohort of genital dryness with burning and irritation, lack of lubrication leading to discomfort or frank dyspareunia during sexual activity, and dysuria, urgency, and recurrent urinary tract infections [1,4].
Symptomatic vulvovaginal atrophy (VVA) dominates the GSM picture. Several surveys have documented the impact of VVA on postmenopausal women’s life. Recent examples are the “Real Women’s Views of Treatment Options for Menopausal Vaginal Changes” (REVIVE) in 3,046 US women or the multinational “Vaginal Health: Insights, Views & Attitudes” (VIVA) online survey in 3,520 women [5,6]. In the VIVA survey, 80% of women reported a negative effect on their lives, including severe interference with sexual intimacy for almost all of them, but also “feeling less sexual” and attractive (68%) and, often and dramatically for self-confidence, “feeling old” (26%) [6].
The label PN-HPT® indicates a mixture of highly purified DNA polynucleotides extracted from male salmon trout gonads; advanced purification and high‐temperature sterilisation procedures ensure the high PN-HPT® safety [7-9]. Intradermal vulvar injections of PN-HPT® in combination with hyaluronic acid, a technically simple and safe procedure, already showed to improve VVA symptoms with a visually evident restructuring of local connective tissues and improvement of genital atrophy and related symptoms [10,11]. A recent study focused on the disrupted sexual life and couple relationship of menopausal women showed great benefits, assessed with the internationally validated “Personal Assessment of Intimacy in Relationships” (PAIR) scale, from a five-session course of technically simple PN-HPT®/HA vulvar injections every fifteen days [11].
This cohort study followed and complemented the previous investigation in a similar cohort of menopausal women centred on the sexual problems of menopause and the benefits of PN-HPT® and HA protected with mannitol [11]. This new study aimed to complement the previous information with more data about PN-HPT®/HA/mannitol vulvar rejuvenation and benefits for VVA symptoms.
Methods
Study Design
A prospective real-world cohort of 60 ambulatory menopausal women with prominent VVA symptoms spontaneously looking to alleviate postmenopausal vaginal dryness and other disturbing atrophy symptoms like thinning or loss of rugae, mucosal pallor, petechiae, and tenderness of the vaginal introitus. The adopted experimental design qualifies the study as observational. Preserving the real-world nature of the investigation required adopting only a few exclusion criteria—genitourinary infections, pelvic organ prolapse surpassing the hymenal ring, vulvar dermatitis or dystrophy causing vulvodynia or chronic vulvar pain, viral infections, and high risk for human Papillomavirus infections, positive Papanicolau test, hormone replacement therapy and all local treatment aimed at the control of vulvovaginal symptoms.
The office-based study respected the Helsinki Declaration and Good Clinical Practice principles. All study materials, which included informed consent forms, study protocol, and case report forms, were preliminarily peer-reviewed for ethical problems.
Vulvar Injection Technique
After full disclosure and written acceptance, by signing an informed consent form, of the foreseeable benefits and risks of vulvar PN-HPT®/HA injections, all enrolled women underwent a five-session cycle of PN-HPT®/HA injections in the skin dermis and mucosal lamina propria of the vulva. Content of the Class-III CE-mark medical device chosen for the study (NewGyn®, Mastelli, Sanremo, Italy)—PN-HPT® (10 mg per mL), HA (molecular weight, 1000-1500 kDa; 10 mg per mL), and mannitol as an inhibitor of enzymatic and oxidative HA degradation (220 micromoles per mL). Formulation: isotonic viscoelastic gel in 2-mL prefilled single-use sterile apyrogenic syringes with 30G/13 mm needles.
As in the previous study that focused on VVA disruption of personal sexual gratification and couple relationships [11], linear retrograde injections were the usual technique in the labia majora area, while micro-wheals were the preferred technique in the labia minora area and around the vaginal meatus and peri-clitoral areas (0.1 mL per wheal with wheals distanced 0.5-1 cm). Needle inclination during intradermal injections: 30-45 degrees.
The usual procedure involved no more than two injections below the posterior labial commissure overlying the perineal body and one or two injections at the anterior labial commissure below the mons pubis. The usual technique calls for injecting the residual syringe content in several small hives on the labia minora at the side of the vestibule and towards the prepuce. Other injection techniques (fan-like pattern, reticular pattern, mixed) were occasionally helpful in individual cases.
The preliminary preparation involved local disinfection and, if needed, a galenic (e.g., 30% lidocaine gel) or proprietary anaesthetic cream applied at the smallest dose sufficient to numb the target vulvar area 30 minutes before the injection. All sessions ended with a prolonged massage of the treated areas to help the local gel diffusion, the suggestion of self-administering further PN-HPT® topically as either vaginal pessaries or vaginal cream at home, and the recommendation of avoiding intercourse and other activities involving rubbing or pressure on treated areas for some days.
Clinical Assessments, Timing, and Parameters
Assessment of demographics and vulvovaginal symptoms — vaginal dryness, irritation, dyspareunia, itching, tenderness/tingling, blood losses, vaginal discharge, urgency, dysuria, recurrent urinary infections; scoring with 10-cm visual analogue scales (VAS, 0=no symptom, 10=unbearable symptom) — was planned at baseline (T0) and after 21, 35, 50, 70 and 90 days (T21, T35, T50, T70 and T90, respectively).
The investigator carefully questioned for side effects and complications at all study visits.
Statistics
The sample size was estimated with the G*Power statistical program version 3.14 based on the worst-case hypothesis, two effect sizes, and the assumption of a 90% power of avoiding false-negative type II errors (ß=0.10) [12]. The sample size was estimated considering a fictional cumulative VAS symptom score and conservatively assuming a conservative 60% estimated improvement at the end of the PN-HPT®/protected HA treatment course. Under these assumptions, the statistical power to detect a significant (two-tailed) divergence in clinical evolution (curves of symptom VAS scores) in 60 postmenopausal women would have been greater than 0.85.
Descriptive data were tabulated as means ± standard errors of the mean (SEM). The statistical analysis was based on the general linear model for repeated measures (Kruskal-Wallis test for independent samples or non-parametric one-way ANOVA on ranks) to assess how PN-HPT®/HA treatment influenced the symptom curves. After detecting a significant divergence from the null-hypothesis lack of treatment effect, pairwise post-hoc Šidák multiple comparisons identified the exact time points of divergence during the follow-up period. All statistical tests were two-tailed 5% significance level [13].
Results
The mean age of the 60 cohort women was 57.6 ± 5.13 years old (median 58.5 years old; range 48-68), with a standard body framework for middle-aged women (weight 64.5 ± 6.60 kg; median 64.0, range 49-78). A natural, usual-age menopause (45 to 53 years old) occurred in 50 women and late natural menopause in five women 55 to 56 years old, while five women underwent surgical menopause because of total hysterectomy in the previous five years. All women of the prospective cohort completed the study; compliance to injections, verified at all visits, was always excellent, and all women completed the planned study sessions.
Figure 1 illustrates the evolution of VAS scores at different assessment times between baseline (T0) and T90 for the more typical and troubling VVA symptoms that presented most severely at baseline—vaginal dryness, irritation, dyspareunia, itching, and tenderness/tingling. At the first short-term follow-up visit after the first intradermal injection (T21), the mean vaginal dryness, dyspareunia, and itching VAS scores had already decreased significantly by 24.0%, 24.7%, and 30.5%, respectively, vs the T0 baseline session. All VVA symptom scores but vaginal dryness and irritation were highly significant at the third treatment session (T50). Secondary VVA symptoms (vaginal discharge, dysuria, frequency, urge incontinence, recurrent urinary tract infections); yet, all women informally reported improvement of those secondary symptoms.
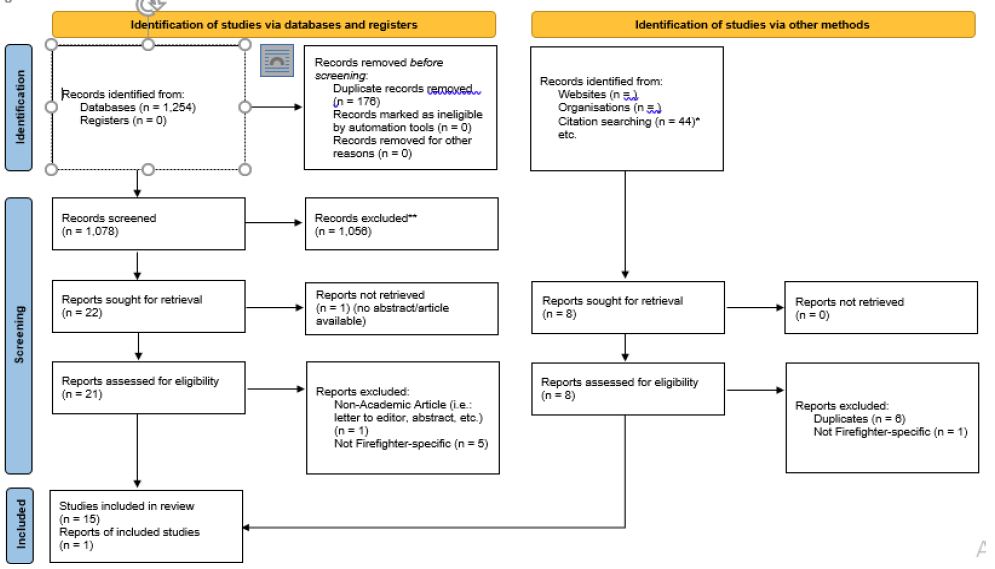
Figure 1: Evolution of mean VVA symptom scores for vaginal dryness, irritation, dyspareunia, itching, tenderness/tingling over the 90-day follow-up period.
* p <0.05 vs baseline; ** p <0.01 vs baseline
Table 1 analytically shows the per cent changes for all VVA symptoms over the study period. When questioned, the cohort women almost unanimously reported pain during intercourse as the most fastidious VVA symptom; only a few women reported itching as the most troubling. When considering the delicate area treated by injection, however minimally invasive, the women’s final judgements about general satisfaction and overall comfort and tolerability were satisfactory: 8.3 ± 8.0 and 6.9 ± 7.0, respectively.
Table 1: Per cent improvements of mean scores for the most representative VVA symptoms between the baseline assessment and treatment session (T0) and the last follow-up session (T90).
|
All VVA symptoms: per cent variations over the study vs baseline |
|||||
|
T21 (first treatment session) |
T35 (second treatment session) |
T50 (third treatment session) |
T70 (fourth treatment session) |
T90 (fifth treatment session) |
|
| Vaginal dryness |
–24.0* |
–41.3* |
–50.2 |
–57.7 |
–63.5** |
| Irritation |
–22.0 |
–41.1* |
–44.4 |
–52.1 |
–57.7** |
| Dyspareunia |
–24.7* |
–43.3** |
–51.2 |
–55.7 |
–59.4** |
| Itching |
–30.5* |
–48.7** |
–55.4 |
–66.0 |
–68.8** |
| Tenderness/tingling |
–22.7 |
–49.7** |
–57.6 |
–70.7 |
–70.0** |
* p <0.05 vs baseline, ** p <0.01 vs baseline
Figure 2 shows one example of what to expect as aesthetic outcomes on labial atrophy after the five-session PN-HPT®/HA/mannitol treatment cycle.
Figure 2: Labial aesthetic improvement at the final assessment session (T90, right photograph) compared to baseline (T0, left photograph).
The investigator and treated women consistently deemed the procedure easy with no unexpected technical difficulty, trouble or discomfort. The occasional, mild side effects at the injection site — local pain, oedema, ecchymosis, and erythema — were expected, of no clinical significance, and resolved rapidly. No other complication of the bio-revitalisation protocol occurred during the 90-day study period. Informally questioned over the study period, all women reported at least a good level of satisfaction with the vulvovaginal aesthetic outcomes.
Discussion
After Japan, Italy is the world’s most rapidly ageing country. An Italian epidemiological study of hospital outpatient services revealed an overall VVA prevalence in postmenopausal women of 79-81%, surging from 65% to 85% after, respectively, one and five years after menopause [1,14]. Regarding the phenotypic expressions of postmenopausal vulvar involution — depletion of labia majora adiposity, blundering of interlabial sulci, loss of pigmentation and hair, reduced density of sweat and sebaceous production, preputial retraction with clitoral exposure and chronic irritation, and overall dysfunction of the vaginal ecosystem — the symptoms are a burden on the woman’s self-confidence and self-image. Microscopically, the fragmentation and fusion of elastin fibres, collagen hyalinisation, and extracellular matrix depletion depict the VVA picture [1,14].
The hydrophilic PN-HPT® polymers reorganise in tissues into a three-dimensional gel that binds water with a moisturising and volume-increasing effect.7-9 Over the longer term, PN-HPT® facilitate the production of new collagen fibres—the rationale for exploring the PN-HPT®/HA option to antagonise the postmenopausal vulvar involution [7-9].
The PN-HPT® passive action develops by replenishing the fibroblast pool of nitrogen bases, nucleosides, and nucleotide precursors and supporting the dermal fibroblast viability.7 PN-HPT® are more potent on collagen production than hyaluronic acid (Figure 3); however, the two principles synergise in co-formulation [7].
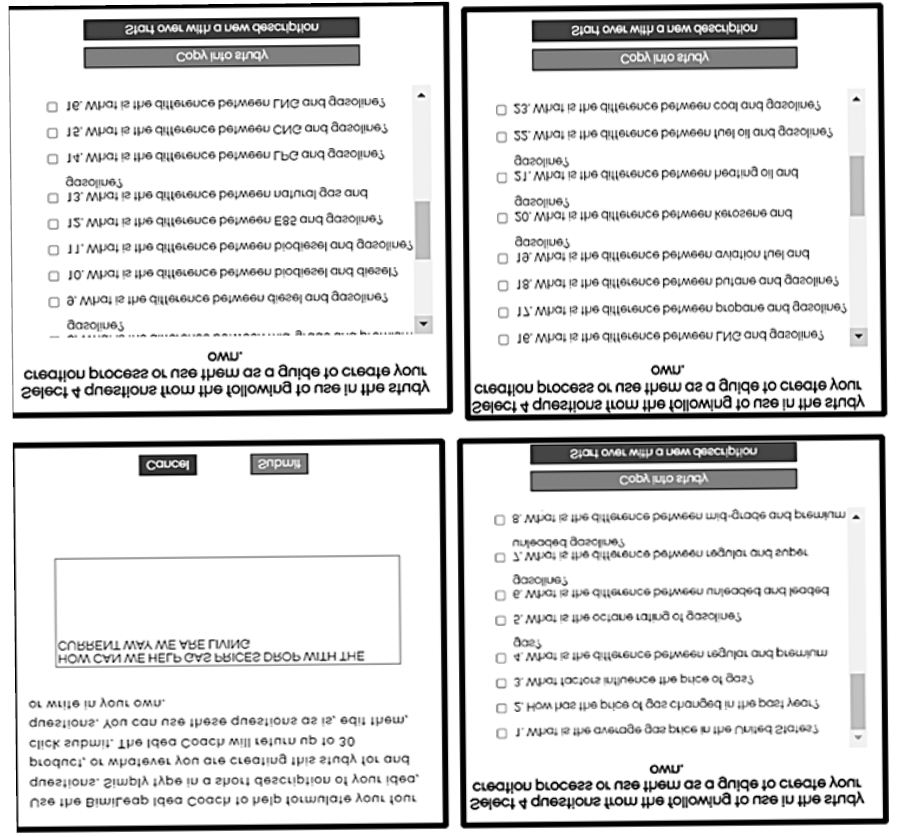
Figure 3: Assessment with transmitted and polarised light and Sirius Red staining for collagen (upper and lower microphotographs, respectively): in the PN-HPT® group, the repair is almost complete with well-organised mature collagen fibres and uniform extracellular matrix (ECM) deposition. Wound healing is incomplete in the hyaluronic acid group, with only sparse collagen fibres and ECM deposition. In contrast, the torpid wound still shows no new collagen fibres and ECM in the control group. Magnification= 4X [7].
Even if rejuvenation was only limited to the vulva, a simple and safe procedure, most cohort women experienced at least some appreciable restructuring of genital connectives and alleviation of atrophy, confirmed by the rapid relief from postmenopausal VVA symptoms afforded by the HPT®/HA/mannitol device. The first weeks of the follow-up period — until T35 and the two first intradermal injections — saw much of the overall improvement. Statistical significance vs baseline severity was attained between twenty-one and thirty-five days after the baseline session, with T35 scores falling between −40.7% for vaginal drying and −50% for tenderness/tingling compared with score improvements between −57.1% for dyspareunia and −66.7% for itching and tenderness/tingling at T90. These outcomes confirm those already perceived in the first exploratory study on VVA symptoms and a more recent study focused on sexual gratification [10,11]: a much shorter treatment course than that tested in those studies can already lead to excellent VVA symptom outcomes. Confirming the favourable impact on the often markedly disrupted sexual life, a derived study involving a subgroup of 47 women belonging to this study cohort demonstrated a significant improvement in personal sexual gratification and couple relationship with an internationally validated specific assessment instrument, the “Personal Assessment of Intimacy in Relationships” (PAIR) scale [11].
A series of maintenance treatment sessions should follow the suggested treatment course to preserve the VVA symptom and sexual gratification benefits-for instance, one maintenance session every two months or the whole three-session cycle twice yearly, according to how the clinical and morphological pictures might evolve over the following months.
The overall study cohort was not homogeneous regarding the menopause age (cohort range, 45 to 56 years old), meaning that the outcomes may have a universal value for all menopausal women. The lack of a control group is a bias; however, the bias impact may not be so severe because the study outcomes are pretty like those of the first exploratory study in menopausal VVA women treated with vulvar PN-HPT® injections [10].
The leading study bias is resorting to impromptu non-validated VAS scoring to assess atrophy-related symptoms. Still, the highly favourable outcomes, uniformly consistent for all investigated symptoms, might lessen the bias severity. Unfortunately, no Italian-language validated translation is available for validated English-language tools like the Vulvovaginal Symptoms Questionnaire (VSQ), the Vulvovaginal Atrophy Questionnaire (VVAQ), and similar questionnaires [15-17]. The single-arm design with a lack of controls, even only a no-treatment control group, and the lack of independent evaluators are other limitations of the study.
As a final summary, the study further supports the previously explored HPT®/HA/mannitol efficacy in restoring vulvar skin quality [18]. This is most likely the biological event underlying the VVA symptom improvement, including the disrupted female sexual life that is by now solidly established [10,11]. However, establishing the comparative effectiveness of HPT®/HA/mannitol and other anti-VVA options must wait for future, well-designed studies.
Acknowledgements
Mastelli S.r.l., Sanremo, Italy, is the patent holder of the PN-HPT® technology and the gel formulations of PN-HPT® injectable polynucleotides used in the study. The authors acknowledge the contribution of Mastelli S.r.l. for supporting the publication costs.
References
- NAMS Position Statement. The 2020 genitourinary syndrome of menopause position statement of The North American Menopause Society. Menopause 27: 976-992. [crossref]
- Labrie F (2010) DHEA, important source of sex steroids in men and even more in women. Prog Brain Res 182: 97-148. [crossref]
- Labrie F (2015) All sex steroids are made intracellularly in peripheral tissues by the mechanisms of intracrinology after menopause. J Steroid Biochem Mol Biol 145: 133-138. [crossref]
- Kagan R, Kellogg-Spadt S, Parish SJ (2019) Practical treatment considerations in the management of genitourinary syndrome of menopause. Drugs & Aging 36: 897-908. [crossref]
- Shifren JL, Zincavage R, Cho EL, Magnavita A, Portman DJ, et al. (2018) Women’s experience of vulvovaginal symptoms associated with menopause. Menopause 26: 341-349. [crossref]
- Nappi RE, Davis SR (2012) The use of hormone therapy for s urogynecological and sexual health post WHI. Climacteric 15: 267-274. [crossref]
- Colangelo MT, Govoni P, Belletti S, Squadrito F, Guizzardi S, et al. (2021) Polynucleotide biogel enhances tissue repair, matrix deposition and organisation. J Biol Regul Homeost Agents 35: 355-362. [crossref]
- Cavallini M, Bartoletti E, members of The Polynucleotides HPT™ Priming Board, Collegio Italiano delle Società Scientifiche di Medicina Estetica (Italian College of the Aesthetic Medicine Scientific Societies) — SIME, AGORÀ, SIES (2021) Consensus report on the use of PN-HPT™ (polynucleotides highly purified technology) in aesthetic medicine. J Cosmet Dermatol 20: 922-928. [crossref]
- Bartoletti E, Cavallini M, Maioli L, et al. (2020) Introduction to Polynucleotides Highly Purified Technology. Aesthetic Medicine 6: 43-47.
- Palmieri IP, Raichi M (2019) Biorevitalization of postmenopausal labia majora, the polynucleotide/hyaluronic acid option. Obstet Gynecol Rep 2019.
- Palmieri IP, Raichi M (2022) Vulvar rejuvenation with polynucleotides HPT® and benefits on postmenopausal sexual life disruption. Obstet Gynecol Rep 2022.
- Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 41: 1149-1160. [crossref]
- Statistical software downloaded from https://www.analystsoft.com/en/products/statplus/#statfeatures
- Cagnacci A, Gallo M, Lello S, Società Italiana della Menopausa (Italian Menopause Society, SIM) and Società Italiana di Ginecologia della Terza Età (Italian Society of the Third-Age Gynecology, SIGiTE) (2019) Joint recommendations for the diagnosis and treatment of vulvo-vaginal atrophy in women in the peri- and postmenopausal phases from the Società Italiana per la Menopausa (SIM) and the Società Italiana della Terza Età (SIGiTE). Minerva Ginecol 71: 345-352. [crossref]
- Erekson EA, Yip SO, Wedderburn TS, Martin DK, Li FY, et al. (2013) The VSQ: a questionnaire to measure vulvovaginal symptoms in postmenopausal women. Menopause 20: 973-979. [crossref]
- Williams RE, Levine KB, Kalilani L, et al. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas 2009, DOI: 10.1016/j.maturitas.2008.12.006.
- Shifren J, Portman D, Krychman M, et al. The Vulvovaginal Atrophy Questionnaire (VVAQ): a novel Patient-Reported Outcome (PRO) for assessing symptoms of vulvovaginal atrophy in menopausal women. Menopause 2017, http://www.menopause.org/docs/default-source/agm/2017-poster-prizer-winners.pdf.
- Goldie K, Kerscher M, et al. Skin Quality – A holistic 360° view: consensus results. Clin Cosmet Investig Dermatol 2021, DOI: 10.2147/CCID.S309374.