Abstract
Haemorrhoids commonly known as piles are among the common anus disorders. It causes the swollen and inflammation of the vein tissues in the anal area. It may be internal haemorrhoids which are characterized with defecation covered with red blood or a painless bleeding during bowel movement. It may also be external haemorrhoids which are characterized by a painful swelling or a hard lump around the anus a condition known as thromboses. It is caused by an increased pressure in the lower rectum due to straining during bowel movement, prolong sitting on toilet, constipation, pregnancy, obesity, low fibre diets, heavy lifting, anal intercourse among others. Effective options are available in the treatment of haemorrhoids, although prescription of conventional drugs may reduce the pain and swelling but they cannot address the cause. Herbs and other botanical medicine can help strengthen and tone the blood vessels, decrease inflammation and stop bleeding. The paper aimed to review both the conventional forms as well as the herbal alternative in the treatment of haemorrhoids.
Keywords
Haemorrhoids, Constipation, Thrombosis, Inflammation, Bleeding, Herbs
Introduction
Haemorrhoids are swollen and inflamed vein in the anal area which is extremely common. It is commonly known as piles and affects most people over the age of 50 and sometimes young people can get them as well. Haemorrhoid is the most common disorder affecting the rectum (last part of the large intestine) and the anus (the opening of the rectum). Haemorrhoids occur as result of a prolong local pressure such as that caused by a pregnancy or a job requiring long hours of sitting which result into swollen and irritation of haemorrhoidal vein [1]. Haemorrhoids may cause irritation and pain especially during defecation. The condition is aggravated by constipation and straining during defecation. In some cases, hemorrhoids may bleed and occasionally clots form in the swollen vein, leading to a severe pain, a condition called thrombosed haemorrhoids [2]. Sometimes haemorrhoids may be associated with painful cracks in the anus (a condition called anal fissure) and itching around the anus, a condition known as pruritus ani [3,4]. Haemorrhoids may be divided into two types; external haemorrhoids and internal haemorrhoids based on their location and symptoms. The external haemorrhoids originate below the dentate line and covered by anoderm. They are characterized by painful swelling and hard lump around the anus that result with the formation of blood clot [5]. On the other hand internal haemorrhoids originate above the dentate line and covered by the anal mucosa. They are characterized by red blood covering feces (a condition called haematochezia), protruding of the anus with pain and itching [5,6]. Figure 1 below showed the pictures of both internal and external haemorrhoids.
People who suffer from haemorrhoids are advised to include in their diet the fibre rich foods such as fresh fruits, vegetables, whole grains product and equally to take plenty of fluids. A mild bulk formatting or softening laxative may also be recommended.
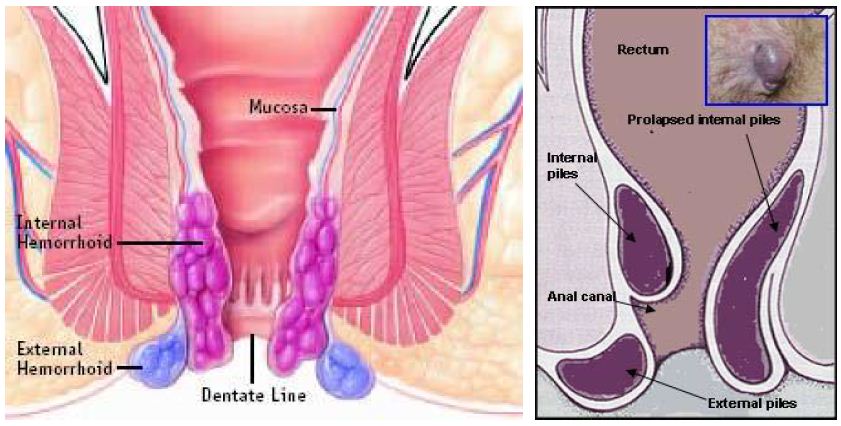
Figure 1: Internal and External Haemorrhoids [7]
Sign and Symptoms
Typical sign and symptoms of haemorrhoids include; anal pain, burning or itching, bright red blood seen on toilet paper, in the toilet bowl or on the surface of the stool after defecation. Round swellings or protrusions in the anal area may also be present.
Causes of Haemorrhoids
Haemorrhoids are caused by genetic weakness of the veins in the rectal area, ageing, setting or standing for a long period of time, anything that causes increased pressure in the veins such as pregnancy, heavy lifting, frequent straining during elimination, obesity, abdominal obesity, anal intercourse among others [1,4]. Some times food and life style such as low fibre diets with resulting constipation, spicy foods, alcohol intake was reported to be linked with the development of haemorrhoids and the aggravation of the acute haemorrhoids symptoms [7,8]. Intolerable pain, severe bleeding or swelling severe enough to prevent normal defecation necessitate the reason why to seek medical attention.
Diagnosis
Haemorrhoids are diagnose through precise history and thorough physical examination through digital rectal examination or anoscopy [9]. Unless bright red blood is clearly seen from haemorrhoids, any patient with rectal bleeding should undergo flexible sigmodoscopy or colonoscopy especially those at the risk of colorectal cancer [10]. The internal haemorrhoids are diagnosed based on appearance and the degree of prolapsed as follows;
Grade I
Haemorrhoids congested/bleeding without prolapsing (that is non-prolapsing haemorrhoids).
Grade II
Haemorrhoids prolapsing during defecation but reduce spontaneously afterward (that is prolapsing haemorrhoids on straining).
Grade III
Haemorrhoids prolapsing during defecation only manually reducible (that is prolapsing haemorrhoids requiring manual reduction), and
Grade IV
Haemorrhoids prolapsed, irreducible (that is non-reducible prolapsing haemorrhoids which include acutely thrombosed, incarcerated haemorrhoids (Clinical Practice Committee, 2004) [11].
Complicated haemorrhoids are often diagnosed as acutely thrombosed external haemorrhoids as well as the strangulated internal haemorrhoids (Figure 2) [10].

Figure 2: (A) Strangulated internal haemorrhoids and (B) Acute thrombosed external haemorrhoids
Treatment
Although prescription of cortisone and anaesthetic product may reduce the pain and swelling of haemorrhoids but they cannot address the causes. Preparations for the relieve haemorrhoids and anal discomfort fall into two main groups; the first group includes the creams and suppositories that act locally to relieve inflammation and irritation. The second group includes the ones that relieve constipation which contribute to the formation of and the discomfort from haemorrhoids and the anal fissure (White and Fooster, 2000). Preparations from the first group often contain a soothing agent with antiseptic, astringent, or vasoconstrictor properties. Ingredients of this group include zinc oxides, bismuth, hamamelis (witch hazel), Peru balsam and ephedrine. Others include a mild anaesthetic such as lignocaine. In some cases ointment containing corticosteroids are recommended [12]. Anti-inflammatory: Cortisone, anaesthetic such as benzocaine (lanacane cream) and lignocaine (Anodesyn, germoloids, boots haemorrhoids ointment) reduces pain and swelling. Ointment and creams such as anacal and anusol cream also reduces pain and swelling (BMA, 2004) [13]. Taking bath with warm water containing soothing herbs inform of essential oil provide a relief to haemorrhoids. Good candidate here includes calendula, comprey, camomile, lavenda and St John’s wort (White and Fooster, 2000). Severe and persistently painful haemorrhoids that continue to be troublesome in spite of all measures may need to be remove surgically (White and Fooster, 2000).
Prevention
Dietary and lifestyle modifications were among the most preventive measures for haemorrhoids [14]. Food rich in fibre and in proanthocyanins and anthocyanidin (two compounds that improve the health of blood vessels) can help to prevent haemorrhoids and can also help in healing the current ones. Also taking multivitamins nutrients improve blood vessels healings and hence help in reducing the risk of haemorrhoids. Similarly, oral fluids, regular exercise, refraining from straining and reading on the toilet, avoiding drugs causing constipation or diarrhea reduce the risk of haemorrhoids [15]. However, dairy foods, meat, fatty foods tend to be constipating, so it is a good idea to minimize or cut back the use of these products.
Contraindication
Most people experience no adverse effect, however sometimes preparations containing local anaesthetic may cause irritation or even a rash in the anal area. The main risk is that self-treatment of haemorrhoids may delay diagnosis of bowel cancer (White and Fooster, 2000). Anti-inflammatory drugs cause allergic reactions, rashes, thinning of the skin and mucous membrane.
Conventional Drugs Used in the Treatment of Haemorrhoids
Several modern drugs and traditional medicine in variety of formats such as pill, suppository, cream and wipes were available. Generally most of the drugs contains phebotonic agent which helps to increase vascular tone, reduce venous capacity, decrease capillary permeability, facilitate lymphatic drainage and has anti-inflammatory effects [16]. They can be categorized into the following:
Soothing and Astringent Agents
This group helps to sooth and makes the skin less oily and stops the wound from bleeding. These include the following:
Aluminium acetate, Bismuth, Peru balsam, Zinc oxides, etc.
Vasoconstrictors
This group helps for veins constriction and strengthens the blood vessels. Example is ephedrine.
Topical Corticosteroids
Examples are hydrocortisone, budesonide, prednisolone.
Local Anaesthetics
These are pain killers, it affect a small part of the body. Examples are Laxatives: bisacodyl, co-danthramer, co-danthrusate, docusate, glycerol, senna, sodium picosulfate, etc.
Herbal Remedies
Herbs and other botanical medicines can help strengthen and tone blood vessels, decrease inflammation and stop bleeding. Herbs applied directly to haemorrhoids can ease symptoms, stop bleeding and speed healing [17]. They can also help reduce the constipation that often accompanies haemorrhoids. Therefore it is recommended to use creams, salves or suppositories that contain combinations of soothing, anti-inflammatory and astringent herbs such as calendula, comfrey, chamomile, lavender, St John’s wart and plantain. Distilled witch hazel is also an excellent astringent that shrinks swollen haemorrhoids and control bleeding. Cypress essential oil may help shrink swollen veins and reduce bleeding. Blend combine soothing herbs that foster wound healing with cooling astringent witch hazel. The following formulation was found to be effective in the treatment of haemorrhoids (White and Fooster, 2000). Dosage: Four (4) table spoons of distilled witch hazel, half (1/2) table spoon of comfrey tincture, half (1/2) table spoon of horse chestnut tincture, 50 drops of lavender essential oil and 50 drops of cypress essential oil. Combine all the ingredient and store in an airtight amber bottle away from heat and light and to be use twice a day using cotton-wool ball deep into the bottle and applied direct on to the haemorrhoids. It can be inserted into the anal opening if internal haemorrhoids are present [18].
Horse Chestnut (Aesculus hippocastanum)
Traditionally it is used for strengthening and toning of veins. It is an anti-inflammatory and therefore decreases swelling. It is also an astringent and tends to reduce bleeding. The herb can be used for treating both the external and internal haemorrhoids.
Dosage
One cup of tea three times a day. The tea is prepared by adding one teaspoon of the dried seeds in 250 ml of hot water. Externally, it is used by soaking a clean flannel in the tea, ring out and then apply to the swollen tissues as often as needed.
Ginkgo (Ginkgo biloba)
Traditionally Ginkgo leaf extracts help in strengthening the blood vessels. It is also an anti-inflammatory as it relieves pain and itching.
Dosage
A quarter to one teaspoon of its tincture two to three times per day or 40 – 60 mg of capsules two to three times per day.
Butcher’s Broom (Ruscus aculeatus)
Traditionally used as anti-inflammatory and it strengthens the blood vessels.
Dosage
One cup of tea three times per day prepared from one to two teaspoon of the dried leaf in 250 ml hot water or half to one teaspoon of the tincture two to three times per day in an empty stomach.
Witch Hazel (Hamamelis virginiana)
This is a strong astringent herb. It stops bleeding and shrinks swollen tissues.
Dosage
The extract product is applied to the swollen tissue three times per day. Caution; never use the product internally.
Dandelion (Taraxacum officinale) and Yellow Dock (Rumex crispus)
These two plants share some common characteristics. Both are considered as weeds, the young green leaves of both can be eating and the roots of both plants are mild, gentle laxatives. The roots are used for treating constipation that comes with haemorrhoids.
Dosage
One to three cups per day prepared from two teaspoon of the dried chopped root in 250 ml hot water or half to three teaspoon of its tincture per day.
Mint (Mentha piperita)
It is also called peppermint, is a herb with downy leaves with purple white flowers. Its seeds contain pungent oil used as flavouring agent. It is used to relief pain and reduced itching of haemorrhoids.
White Dammar (Vateria indica):
It is used traditionally to heal haemorrhoids. It exerts anti-inflammatory action and hastens healing [19-21].
Conclusion
Many people get relief with home treatment but the main reason to seek medical attention are intolerable pain, severe bleeding or swelling severe enough to prevent normal defecation. There are several available home treatments (both conventional and herbal) which can be an alternative to the present day surgical methods. Conventional drugs were accompanied with many side effects while herbal alternatives are characterized with less contraindication, low cost and commonly available as such herbal alternatives are categorized as the best home treatment solutions for haemorrhoids.
References
- Azeemuddin M, Gollaplle LV, Mohammed R, Agadi HT, Mirza RB, et al. (2014) An Improved Experimental Heamorrhoids in Rats: Evaluation of Antiheamorrhoidal Activity of a Herbal formulation. Pharmacology 1: 1-7. [crossref]
- Lee JH, Kim HE, Kang JH, Shin JY, Song YM (2014) Factors associated with hemorrhoids in korean adults: korean national health and nutrition examination survey. Korean J Fam Med 35: 227-236. [crossref]
- Lin JK (1989) Anal manometric studies in hemorrhoids and anal fissures. DisColon Rectum. 32: 839-842. [crossref]
- Thomson WH (1975) The nature and cause of haemorrhoids. Proc R SocMed 68: 574-575. [crossref]
- Hindustan AA, Chitta SK, Kishore KRB, Kranthi G, Krishna MCH, et al. (2010) Herbal Treatment for Heamarrhoids. JITPS 1: 236-244.
- Hosking SW and Johnson AG (1988) Bleeding anorectal varices–a misunderstood condition. Surgery 104: 70-73. [crossref]
- Shivani T, Vijayabhaskar K, Srinivasa PR, Anil Kumar B, Yadav K (2019) Anti-Hemorrhoidal Activity of Leaf Butanol Fraction Portulaca Oleracea , Belonging To the Family Portulacaceae. Journal of Pharmacy and Biological Sciences 14: 16-20.
- Pigot F, Siproudhis L, Allaert FA (2005), Risk factors associated with hemorrhoidal symptoms in specialized consultation. Gastroenterol Clin Biol 29: 1270-1274. [crossref]
- Lohsiriwat V (2013) Approach to hemorrhoids. Curr Gastroenterol Rep 15. [crossref]
- Lohsiriwat V (2012) Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol 18: 2009-2017. [crossref]
- Clinical Practice Committee (2004) American Gastroenterological Association. American Gastroenterological Association medical position statement: Diagnosis and treatment of hemorrhoids. Gastroenterology 126: 1461-1462.
- Bouskela E, Cyrino FZ, Marcele G (1994) Possible Mechanism for the Inhibitory effect of Ruscus Extracts on Increased Microvascular Permiability Induced by Histamine in Hamster Cheek Pouch. Cardiovasc Pharmacol. 24: 281-285. [crossref]
- BMA 6th Pg: 114-115.
- Alonso-Coello P, Mills E, Heels-Ansdell D, López-Yarto M, Zhou Q, Johanson JF, et al. (2006) Fiber for the treatment of hemorrhoids complications: a systematic review and meta-analysis. Am J Gastroenterol 101: 181-188. [crossref]
- Lohsiriwat V (2014) Update on common anorectal diseases. Tech Coloproctol 18: 87-88.
- Misra MC (2005) Drug treatment of haemorrhoids. Drugs 65: 1481-1491. [crossref]
- Brinkhaus B, M. Lindner DS, Hahn EG (2000) Chemical, pharmacological and clinical profile of the East Asian medical plant Centella asiatica. Phytomedicine 7: 427-448. [crossref]
- Salvati EP (1990) Management of acute hemorrhoidial disease. Perspect Colon Rectal Surg. 3: 309-314. [crossref]
- Linda BW, Steven F (2000) The Herbal Drugstore. Herbs Companion Press pg: 282-284.
- Lohsiriwat V (2009) Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol 18: 2009-2017. [crossref]
- John AH (2004) New Guide to Medicine and Drugs, British Medical Association.