Process mapping can be described as an “entire approach that leads to a holistic understanding of the process under review” [1] Although it has its roots outside lean thinking, process mapping has become part and parcel of the lean “toolkit”, and is used with lean practice given its strengths in data collection and process re-design by identifying value add and non-value add processes [2-4]. It involves documenting activities of a process in a detailed graphical format. Process mapping has long been an important technique in service assessment and improvement [5]. It has the advantage of communicating roles and responsibilities to team members, providing a useful “what-if” tool and improving all round efficiency [1]. In recent years, it has become a key component of popular techniques such as Six Sigma and lean thinking [6,7]. Figure 1 is an example of a process map from a project examining discharge of high risk patients [8].
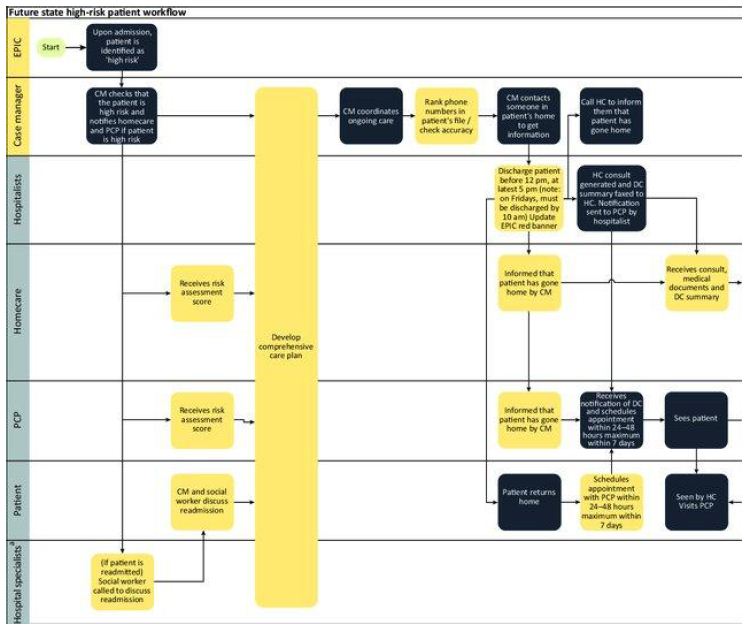
Figure 1: Swim lane diagram outlining steps within the discharge process.
Process Mapping in Healthcare
Process mapping has recently been used to examine and improve healthcare processes. It may also allow health policy decision makers to view the management of a medical condition in the form of sequential events, and by doing so gaining an insight into both the patient and staff experience [9]. Process Mapping has demonstrated clinical benefit in improving efficiency and reducing unnecessary or ineffective care [10].
A recent review of the literature by Antonacci et al. examined the findings of eight quality improvement projects from different healthcare settings within the NHS [11]. Inductive analysis on interviews of partcipants experience of using process mapping was carried out. There were eight key benefits related to process mapping reported by the participants;
(i) Gathering a shared understanding of the reality.
(ii) Identifying improvement opportunities.
(iii) Engaging stakeholders in the project.
(iv) Defining the project’s objectives.
(v) Monitoring project progress.
(vi) Learning
(vii) Increased empathy.
(viii) The simplicity of the exercise.
Five factors related to a successful process mapping exercise were identified;
(i) Simple and appropriate visual representation.
(ii) Information gathered from multiple stakeholders.
(iii) Facilitator’s experience and soft skills.
(iv) Basic training.
(v) Iterative use of process mapping throughout the project.
There are limitations to process mapping. It can be a costly and lengthy exercise. Manual process mapping takes resources in the form of money and time. There is a team directly responsible for producing the map, as well as the employees who are brought away from their work to be contribute their knowledge to the project [12], Process mapping often relies on the memory of the person describing the process, and any gap in that recollection can lead to a gap or error in the process map [12]. One way of remedying this is the “walk the journey” method of data collection, where the entire process is observed by the mapping team. This technique has been recommended for use in process mapping exercises in healthcare, with the added advantage of experiencing the patient journey and improving patient empathy [13].
Time Driven Activity Based Costing
Another use of Process Mapping is that of a costing approach, where the sequential events derived from process mapping can be used in time-driven activity-based costing (TDABC). TDABC uses two parameters [14];
(i) The unit cost supplying capacity and
(ii) The time required to perform the activity.
In 2011, Kaplan and Porter set out a seven step approach to TDABC in healthcare settings [15], presented in Table 1 below. TDABC model has been shown to be successful in process assessment and costing activities across a variety of disciplines, including emergency medicine, paediatrics, neurology and oncology [16-19]. In the systematic review of TDABC studies in the literature, Keel et al. found TDABC to be used in both operational improvement and also to inform reimbursement policy [20]. TDABC was found to be a simple procedure, yet more accurate than traditional activity-based costing. They noted that other than defining the medical condition and care delivery value chain, all other steps set out by Kaplan and Porter are mandatory for a proper TDABC analysis. The emerging theme was that TDABC is a growing discipline and should be slowly incorporated into existing systems to provide the best cost assessments possible [20].
Table 1: Seven steps of TDABC in healthcare.
|
Step |
Process |
| Step 1 |
Select the medical condition. |
|
Step 2 |
Define the care delivery value chain. |
| Step 3 |
Develop process maps of each activity in patient care delivery. |
| Step 4 |
Obtain time estimates for each process. |
| Step 5 |
Estimate the cost of supplying patient care resources. |
| Step 6 |
Estimate the capacity of each resource, and calculate the capacity cost rate. |
| Step 7 |
Calculate the total cost of patient care. |
Footnote: Steps 2 and 3 of this model are delivered by the use of Process Mapping. In order for a precise costing model to be achieved, each event in the process must be detailed and a cost allocated.
Conclusion
Process mapping has long been a valuable tool in industrial engineering. It is beginning to find its way into healthcare settings and this should be welcomed, both for service improvement and of more general service evaluation, with a notable example being time-driven activity based costing. This methodology provides an easy-to-follow and accurate cost evaluation of healthcare services where staff time is the main driver of cost.
References
- Jacka JM, Keller P.J (2009) Business Process Mapping: Improving Customer Satisfaction.
- Rahani AR, AL-Ashraf M (2012) Production flow analysis through value stream mapping: a lean manufacturing process case study. Procedia Engineering 41: 1727-1734.
- Klotz L, Horman M, BI HH, Bechtel J (2008) The impact of process mapping on transparency. International Journal of Productivity and Performance Management 57: 623-636.
- King DL, Ben‐tovim DI, Bassham J (2006) Redesigning emergency department patient flows: application of lean thinking to health care. Emergency Medicine Australasia 18: 391-397. [crossref]
- Hunt VD (1996) Process mapping: how to reengineer your business processes, John Wiley & Sons.
- Schroeder RG, Linderman K, Liedtke C, Choo AS (2008) Six Sigma: Definition and underlying theory. Journal of Operations Management 26: 536-554.
- Womack JP, Jones, DT (1997) Lean thinking—banish waste and create wealth in your corporation. Journal of the Operational Research Society 48: 1148-1148.
- Das P, Benneyan J, Powers L, Carmody M, Kerwin J, Singer S (2018) Engineering safer care coordination from hospital to home: lessons from the USA. Future Healthcare Journal 5: 164-170. [crossref]
- Kim CS, Spahlinger DA, Kin JM, Billi JE (2006) Lean health care: what can hospitals learn from a world‐class automaker?. Journal of Hospital Medicine: an official publication of the Society of Hospital Medicine 1: 191-199. [crossref]
- Susan Oliver, Ailsa Bosworth, Mara Airoldi, Helen Bunyan, Audrey Callum (2008) Exploring the healthcare journey of patients with rheumatoid arthritis: a mapping project–implications for practice. Musculoskeletal Care 6: 247-266. [crossref]
- Antonacci G, Reed JE, Lennox L, Barlow J (2018) The use of process mapping in healthcare quality improvement projects. Health services management research 31: 74-84. [crossref]
- BIAZZO S (2002) Process mapping techniques and organisational analysis. Business Process Management Journal.
- Trebble TM, Hansi N, Hydes T, Smith MA, BAKER M (2010) Process mapping the patient journey: an introduction. BMJ.
- KAPLAN RS, Anderson SR (2003) Time-driven activity-based costing. Available at SSRN 485443.
- Kaplan RS, Porter ME (2011) How to solve the cost crisis in health care. Harv Bus Rev 89: 46-52. [crossref]
- MClaughlin N, Burke MA, Setlur NP, Niedzwiecki DR, Kaplan AL, et al. (2014) Time-driven activity-based costing: a driver for provider engagement in costing activities and redesign initiatives. Neurosurgical Focus
- Yun BJ, Prabhakar AM, Warsh J, Kaplan R, Brennan J, et al. (2016) Time-driven activity-based costing in emergency medicine. Annals of Emergency Medicine 67: 765-772. [crossref]
- Yangyang RY, Abbas PI, Smith CM, Carberry KE., Ren H, et al. (2016) Time-driven activity-based costing to identify opportunities for cost reduction in pediatric appendectomy. Journal of Pediatric Surgery 51: 1962-1966. [crossref]
- Laviana AA, Ilg AM, Veruttipong D, Tan HJ, Burke MA, et al. (2016) Utilizing time‐driven activity‐based costing to understand the short‐and long‐term costs of treating localized, low‐risk prostate cancer. Cancer 122: 447-455. [crossref]
- Keel G, Savage C, Rafiq M, Mazzocato P (2017) Time-driven activity-based costing in health care: a systematic review of the literature. Health Policy 121: 755-763. [crossref]