Abstract
Background and Aim: Temporomandibular joint ankylosis (TMJA) is a fusion of the head of the mandibular condyle to the glenoid fossa of temporal bone at the skull base. This fusion is either fibrous, osseous, or fibro-osseous. The objective of this study is to determine the prevalence of TMJ ankylosis.
Material and Methods: This retrospective cross-sectional study was carried out in all patients who admitted in maxillofacial departments in the period January 2018 to September 2022 in Al-Thawra, Al-Gumhouri, 21 September, Al-Kuwait, Modern European Hospital, and University of Science and Technology Hospital, all these hospitals in Sana’a city. This study was based on data taken from patients’s files that include: age, gender, date of operation, etiology, side of ankylosis, type of radiograph, type of ankylosis, and type of treatment.
Results: Among the 55 patients, 63.6% were male and 36.4% were female. The mean (SD) age of patients was 15.27 <0x7E> 10.02 years (age range 4 to 55 years). Trauma was the most common cause of TMJ ankylosis (85.5%). Unilateral ankylosis was more common than bilateral; in unilateral right and left sides of TMJ, ankylosis was in equal frequency (14,50%).. A CT scan was the most radiographic x-ray used for the diagnosis of TMJ ankylosis (74.5%). Osseous ankylosis (34.5%) was the most frequent type, followed by fibroosseous (32.7%) and fibrous (21.8%). Gap arthroplasty was the most common type of treatment (29.1%).
Conclusions: In this study we revealed that the ankylosis was more prominent in males because males were more susceptible to trauma, which was the most common cause of TMJ ankylosis. A CT scan was the most radiographic x-ray used for the diagnosis. Cases of unilateral ankylosis were more than bilateral. Osseous ankylosis was the most frequent type. Gap arthroplasty was the most common type of treatment.
Keywords
Temporomandibular joint ankylosis (TMJA), Prevalence, Sana’a, Yemen
Introduction
The fusing of the mandibular bone’s condyle to the temporal bone’s glenoid fossa at the base of the skull is known as temporomandibular joint (TMJ) ankylosis [1]. It can develop at any age, but it is more frequent in children under the age of ten [2,3]. TMJ is regarded as the cornerstone of craniofacial integrity, so ankylosis in children causes mandibular disturbances because malocclusion from growth period results in distressing conditions like poor oral hygiene, impaired speech, difficulty chewing, facial disfigurement, compromised airway, and psychological stress [4]. Clinical manifestations of TMJA depend on the age at which ankylosis onset, the period of TMJA persistence, and whether the ankylosis is unilateral or bilateral. When it affects children before their growth has stopped, it causes severe problems in mastication, digestion, speech, and oral hygiene [5,6]. Clinical manifestations in unilateral ankylosis: facial asymmetry, the mandible and chin deviated to the affected side, the face on the affected side is roundness and fullness, and the lower border of the mandible on the affected side has a concavity that ends in a well-defined antegonial notch. Whereas in bilateral ankylosis, the mandible is symmetrical but small in size (retrognathic/micrognathic), there is an inability to open the mouth progresses by a gradual decrease in interincisal opening, “bird face” deformity with receding chin and the patient has a convex profile, the neck-chin angle may be reduced or almost completely absent, the antegonial notch is well defined bilaterally, and class II malocclusion can be noticed [7].
Additionally, in severe cases of TMJA, it can move the tongue posteriorly and reduce the size of the oropharyngeal airway, which can eventually cause upper airway obstruction and obstructive sleep apnea syndrome (OSAS). As a result, growing children often present a triad of symptoms, as follows: TMJ ankylosis, micrognathia, and OSAS [8]. TMJ ankylosis can be intraarticular or true and extraarticular or false. Most commonly, intraarticular ankylosis appears after trauma or infection, whereas in extraarticular type it occurs by a large variety of other disorders, including myogenic, neurogenic, and inflammatory processes, as well as bone and soft tissue tumors [9]. TMJ ankylosis has several etiological causes, including trauma, local and systemic inflammatory conditions, neoplasm, and TMJ infection. Trauma and infection are the most frequent causes [10].
Under general anesthesia, surgery is the preferred method of treating TMJ ankylosis, and there are many techniques for intubation of ankylosis patients, such as blind awake intubation, retrograde intubation, fiberoptic intubation, and tracheostomy intubation [11]. The management objectives in TMJA are the removal of the ankylotic mass, restoring the shape and function of the joint, allowing mouth opening, relief of upper airway obstruction, and prevention of recurrence [1]. Regarding the ideal treatment for TMJA, there are different procedures between surgeons, and there is no specific treatment. Recurrence still represents the main challenge in the management of TMJ ankylosis, as has been explored and developed by many authors [12]. A variety of operative procedures are used to treat TMJA, but none have been universally accepted. The operative procedures include gap arthroplasty, interpositional arthroplasty, and resection of the ankylotic mass, followed by reconstruction of the ramus-condyle unit with autogenous or alloplastic grafts [13]. This fusion is either fibrous, osseous, or fibro-osseous. The objective of this study is to determine the prevalence of TMJ ankylosis.
Methodology
Study Design
A retrospective cross-sectional study was conducted in Sana’a city in Yemen.
Study area
The study was conducted in Al-Thawra, Al-Gumhouri, 21 September, Al-Kuwait, University of Science and Technology, Modern European Hospital, in Sana’a city. These hospitals are the main referral hospitals in Yemen; they are three public, one military, and two private. Most maxillofacial surgeons are worked in these hospitals, and most TMJ ankylosis cases are referred to these hospitals.
Study Population
This study was carried out in all patients who admitted in maxillofacial departments in the period January 2018 to September 2022 and who were diagnosed with TMJ ankylosis and underwent surgical treatment. Patients associated with other facial fractures, patients who had TMJ disorder other than ankylosis, and patients that had files with incomplete data were excluded.
Data Collection
In this study, information was obtained from the patient’s archives or/and soft copies who were admitted for TMJ ankylosis in the oral and maxillofacial surgery departments of the targeted hospitals and reviewed and collected for the last five years. In Al Kuwait hospital, and after completing the entry procedures to the statistics departments, we found that there is no special section for the maxillofacial surgery. It was necessary to search in all departments of surgery, and about 1200 files for the maxillofacial surgery were obtained. The result was to get 15 cases of TMJ ankylosis. The same was in all government hospitals that were investigated, because there is no data stored in the electronic system. Also, we found 30 cases of TMJ ankylosis in Al Thawra Hospital, 4 cases in September 21 hospitals, and 6 cases in Modern European Hospital. In some patients’s files, the relatives don’t know about the cause of TMJ ankylosis, so they are added as unknown in the result and discussion. In the University of Science and Technology Hospital, there was no data about TMJ ankylosis because of an error in the system, and in Al-Gumhouri Hospital, there are no cases of TMJ ankylosis.
Data Processing and Analysis
Data was coded, entered into the computer, processed, edited, and analyzed using Excel 2010 and the Statistical Package for Social Science (SPSS) version 25, which was used to conduct the appropriate tests for the study, as the following tests were used: frequencies and percentages, chi-square test to measure the relationship between the variables of the study.
Ethical Committee
Ethical approval was obtained from the Medical Ethics Committee of the Faculty of Dentistry, Sana’a University.
Results
The study reveals that the majority of respondents were male, accounting for 30.9% of the total. The age distribution was dominated by those aged 10-15, followed by those aged 16-20, 12.7% over 25, and the least common age group (ages 21-25). Hospitals were the most frequent, with Al-Thawra Hospital having the highest number of respondents (54.5%). The most common etiology of ankylosis was trauma (85.5%), followed by bipolar and unilateral (49.1%). The most common type of radiography was CT scan (74.5%), followed by panoramic and CT scan (18.2%), and panoramic (7.3%). The most common type of ankylosis was osseous (34.5%), followed by fibrous (32.7%), and the least common type was unknown (10.9%). The study also revealed that the majority of respondents had a type of ankylosis, with the majority of respondents having a fibrous type (Tables 1-15).
Table 1: Frequency Distribution–Age of Respondents
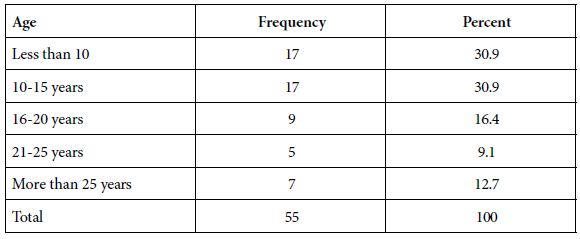
Table 2: Frequency Distribution–Gender of Respondents
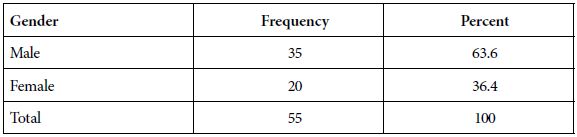
Table 3: Frequency Distribution– Hospital
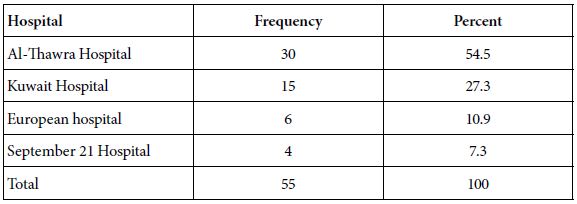
Table 4: Frequency Distribution– Etiology of ankylosis
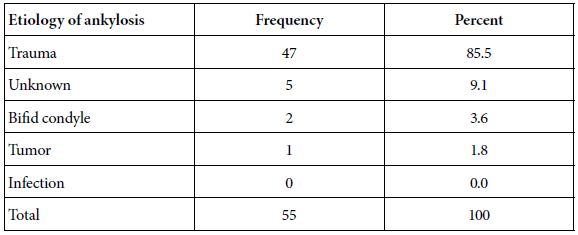
Table 5: Frequency Distribution– Side of ankylosis
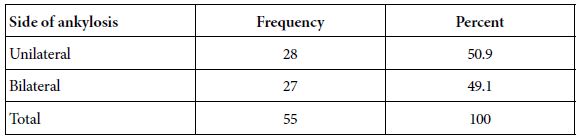
Table 6: Frequency Distribution– Side of unilateral
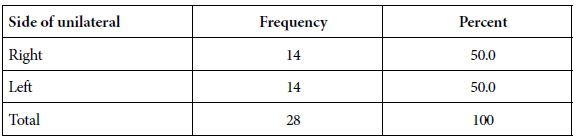
Table 7: Frequency Distribution – Type of radiography
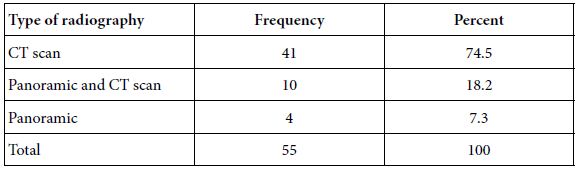
Table 8: Frequency Distribution– Type of ankylosis
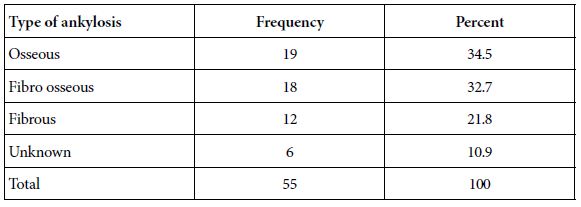
Table 9: Frequency Distribution– Type of treatment
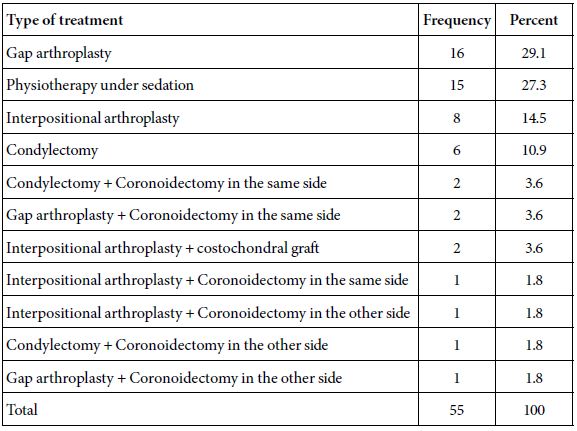
Table 10: Relationship between side of ankylosis and gender
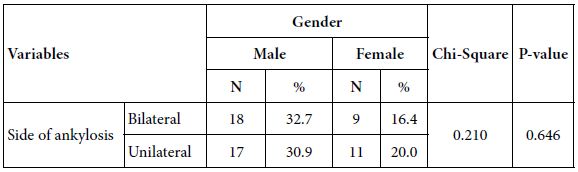
Table 11: Relationship between side of unilateral and gender
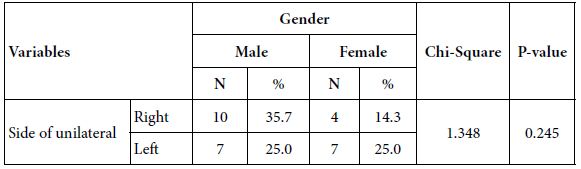
Table 12: Relationship between type of ankylosis and gender
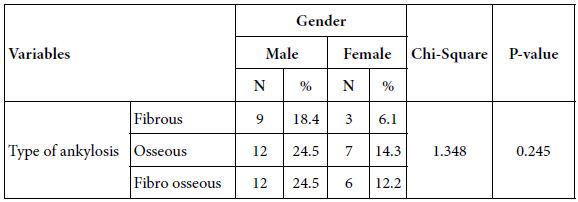
Table 13: Relationship between side of ankylosis and age
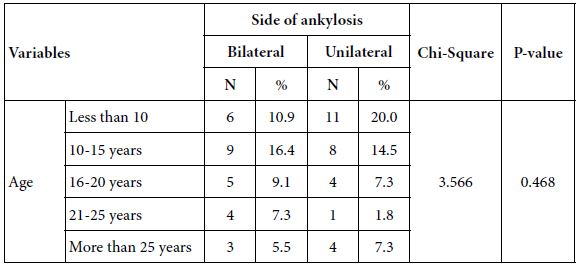
Table 14: Relationship between side of unilateral and age
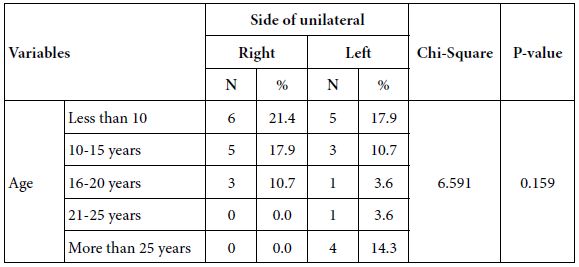
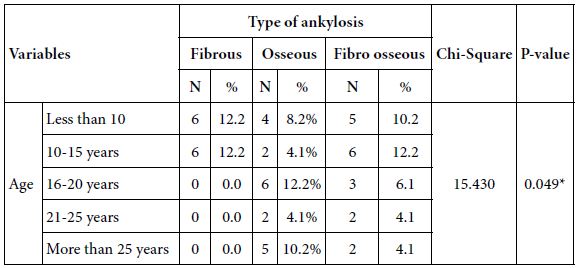
Table 15: Relationship between type of ankylosis and age
Discussion
In this study, the age of the patients ranged from 4-55 years with a mean age of 15.27 <0x7E> 10.02, and the frequency of TMJ ankylosis was highest in the second decade (47.3%), followed by the first decade (30.9%). The finding of the most frequently occurring age group was the same with the studies conducted in Pakistan [6], Egypt [14], and Ethiopia [15]. In contrast, a study in Sudan revealed that most of the cases were in the first decade of the age [1]. The majority of patients in this study were male, 35 (63.6%), and this is similar to studies in Nigeria [2], Ethiopia [16], and Brazil [10], where male cases were predominant. This result can be explained by the fact the fact that the males are more likely to be injured than the females because of their high-risk activities and are more susceptible to trauma.
This study shows that the greatest number of cases were in Al Thawra 30 (54.5%) because it’s considered the largest hospital in receiving cases in Sana’a city, followed by Al-Kuwait Hospital 15 (27.3%).
The current study revealed that trauma was the most common cause of TMJ ankylosis, representing (85%) of all cases, and these resemble previous studies in Pakistan [6], India [17,18], and South Africa [19], in which trauma was the most common cause of TMJ ankylosis. In the current study, there were no ankylosis cases due to infection. This was in contrast to many studies that revealed the infection is one of the most common causes of ankylosis among children and adult patients [20,21].
In this study, the frequency of unilateral (right or left) ankylosis (50.9%) was slightly higher than bilateral, and this resembles result findings in studies from China [22], Pakistan [6], Brazil [10], and India [23], while the current study found the right side TMJ ankylosis was equal to the left side TMJ ankylosis 14 (50%).
The current study showed that CT scan was the most radiographic x-ray used for diagnosis of TMJ ankylosis (74.5%), and this was similar to the results of other studies [24,25]. Followed by a panoramic and CT scan (18.2%), and a panoramic x-ray was the least used x-ray for the diagnosis TMJ ankylosis (7.3%).
About a type of ankylosis frequency in this study, three different types of ankylosis were identified: osseous 19 (34.5%) and represent the greatest number of cases due to most patients presented late probably because of ignorance, poverty, and lack of easy access to treatment, followed by fibroosseous ankylosis (32.7%) and fibrous ankylosis (21.8%). These results were similar to previous studies done in Delta Nile, Egypt [26]. In the current study, there is an association between the type of ankylosis and age, in which all cases of fibrous ankylosis were found in children under the age 15 (p = 0.049).
In the current study, the gap arthroplasty was the most commonly done procedure (29.1%), and this agrees with many of the previous studies in India [27], Ethiopia [28], and South Africa [19]. Gap arthroplasty is the most commonly done procedure due to its simplicity, low surgical cost, and short operating time, but it has disadvantages of short ramus height, pseudoarticulation, anterior open bite in bilateral cases, premature occlusion on the affected side and open bite on the contralateral side in unilateral cases, decreased postoperative range of motion, and increased risk of reankylosis [28], followed by physiotherapy under sedation (15.3%), and this type of treatment is found in cases of fibrous ankylosis in Al Tharwa hospital. Interpositional arthroplasty cases were 8 (14.5%); this procedure is preferred by a lot of surgeons due to reducing the risk of recurrence of ankylosis, restoring the vertical height of the ramus, and preventing open bites when using interpositional arthroplasty in treatment cases of bilateral TMJ ankylosis [29]. In the cases of coronoidectomy for the same side of ankylosis, there were 2 cases in the condylectomy procedure and also 2 cases in the gap arthroplasty procedure, which represents 3.6% in each type of treatment, and this agrees with [10]. The type of treatment group with coronoidectomy on the other side that is used in condylectomy, gap arthroplasty, and interpositional arthroplasty procedures. The number of cases was 1 in each procedure and represented (1.8%) in each procedure, respectively; this resembles a previous study in Brazil [10]. Also, there was only 1 case of interpositional arthroplasty with coronoidectomy on the same side (1.8%). The last type of treatment group was interpositional arthroplasty with costochondral graft or total joint replacement with costochondral graft, which was 2 cases and represents (3.6%); this is similar to that reported by Mabongo and Karriem (2014) [19]. The costochondral graft is the optimal method for reconsteruction of TMJ, especially in children due to a chance for growth of a mandible.
Conclusion
The study explores the demographics, etiology, radiographic diagnosis, types of ankylosis, and surgical treatments of TMJ ankylosis in Yemen. It reveals a high incidence of trauma, with the second decade being the most common age group. The most common type is osseous ankylosis, followed by fibroosseous and fibrous ankylosis. The study also highlights the need for further research to develop more effective treatments. Thefindings underscore the need for improved diagnosis and treatment of this challenging condition.
Recommendation
The text emphasizes the importance of raising awareness about TMJ ankylosis among healthcare professionals and the public, implementing preventive measures, encouraging early diagnosis and treatment, and implementing standardized protocols. It also calls for increased availability of specialized healthcare facilities, further research for more effective treatments, and improved patient data archiving methods.
Limitations
The current study’s limitations include the scarcity of data in patient files, the unwillingness of certain hospitals to collaborate with us in order to meet the study’s objectives, and the challenges associated with gathering data from old hospital archives.
Data Availability
The accompanying author can provide the empirical data that were utilized to support the study’s conclusions upon request.
Acknowledgments
The authors would like to thank Yemen and the Faculty of Dentistry at Sana’a University for their kind cooperation.
Dispute of Interest
There are no conflicts of interest in regard to this project.
Author’s Contributions
Dr. Basheer Saeed Mohammed Khalid: Formal analysis, conceptualization, data organization, and clinical and laboratory examinations to obtain a master’s degree in Oral and Maxillofacial Surgery. Professor Sam Abd Alkarem Da’er: Methodology, formal analysis, visualization. Other authors supervised the clinical part of the work. All authors reviewed the article and approved the final version.
References
- ELTOHAMI Y, ABUAFFAN A, ALSAGH R, MOHAMED H, ALI A (2017) Temporomandibular joint ankylosis pattern, causes, and management among a sample of Sudanese children. Den Craniofac Res 2: 1.
- BELLO SA, OLOKUN BA, OLAITAN AA, AJIKE SO (2012) Aetiology and presentation of ankylosis of the temporomandibular joint: report of 23 cases from Abuja, Nigeria. British Journal of Oral and Maxillofacial Surgery 50: 80-84. [crossref]
- KUMAR N, SARDANA R, KAUR R, JAIN A (2016) Intraoperative mandibular nerve block with peripheral nerve stimulator for temporomandibular joint ankylosis. Journal of Clinical Anesthesia 35: 207-209. [crossref]
- ANYANECHI C, OSUNDE O, BASSEY G (2015) Use of oral mucoperiosteal and pterygo-masseteric muscle flaps as interposition material in surgery of temporomandibular joint ankylosis: A comparative study. Annals of Medical and Health Sciences Research 5: 30-35. [crossref]
- TANRIKULU R, EROL B, GöRGUN, B., SöKER M (2005) The contribution to success of various methods of treatment of temporomandibular joint ankylosis (a statistical study containing 24 cases) Turk J pediatr 47: 261-265. [crossref]
- HOSSAIN MA, SHAH SAA, BISWAS R S R (2014) Frequency of temporomandibular joint ankylosis in various age groups with reference to etiology. Chattagram Maa-O-Shishu Hospital Medical College Journal 13: 17-20.
- DE LEEUW R, KLASSER G D (2018) Orofacial pain: guidelines for assessment, diagnosis, and management, Quintessence Publishing Company, Incorporated Hanover Park, IL, USA.
- ANDRADE N, KALRA R, SHETYE S (2012) New protocol to prevent TMJ reankylosis and potentially life threatening complications in triad patients. International journal of oral and maxillofacial surgery 41: 1495-1500. [crossref]
- SU-GWAN K (20010. Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flap. International Journal of Oral and Maxillofacial Surgery 30: 189-193. [crossref]
- VASCONCELOS BCDE, PORTO GG, BESSA-NOGUEIRA RV (2008) Temporo mandibular joint ankylosis. Revista Brasileira de Otorrinolaringologia 74: 34-38. [crossref]
- ENTERLEIN G, BYHAHN C (2013) Practice guidelines for management of the difficult airway: update by the American Society of Anesthesiologists task force. Der Anaesthesist 62: 832-835.
- MANGANELLO-SOUZA L, MARIANI P (2003) Temporomandibular joint ankylosis: report of 14 cases. International Journal of Oral and Maxillofacial Surgery 32: 24-29. [crossref]
- MEHROTRA D, PRADHAN R, MOHAMMAD S, JAISWARA C (2008) Random control trial of dermis-fat graft and interposition of temporalis fascia in the management of temporomandibular ankylosis in children. British Journal of Oral and Maxillofacial Surgery 46: 521-526. [crossref]
- ELGAZZAR R, ABDELHADY A, SAAD K, ELSHAAL M, HUSSAIN M.et al (2010a) Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. International Journal of Oral and Maxillofacial Surgery 39: 333-342. [crossref]
- GAROMA G, DEJENE D, UMA G (2022) Temporomandibular joint ankylosis; aetiology, pattern and treatment. J Dent Health Oral Disord Ther 13: 33-37.
- TEFERA T (2019) Incidence, clinical presentation and surgical management of Temporomandibular Joint ankylosis: A 5 year retrospective study. Scientific Archives of Dental Sciences 2: 2-14.
- MISHRA N, SHARMA NK, DHIMAN N K, JAISWARA C, TIWARI P. et al (2021) Temporomandibular joint ankylosis: A tertiary center-based epidemiological study. National Journal of Maxillofacial Surgery 12: 392. [crossref]
- GUPTA VK, MEHROTRA D, MALHOTRA S, KUMAR S, AGARWAL G G et al (2012) An epidemiological study of temporomandibular joint ankylosis. National Journal of Maxillofacial Surgery 3: 25. [crossref]
- MABONGO M, KARRIEM G (2014) Temporomandibular joint ankylosis: evaluation of surgical outcomes. J Dent Med Sci 13: 60-66.
- KABAN LB, BOUCHARD C, TROULIS MJ (2009a) A protocol for management of temporomandibular joint ankylosis in children. Journal of Oral and Maxillofacial Surgery 67: 1966-1978. [crossref]
- MOVAHED R, MERCURI L G (2015b) Management of temporomandibular joint ankylosis. Oral and Maxillofacial Surgery Clinics 27: 27-35. [crossref]
- CHEN S, HE Y, AN JG, ZHANG Y (2019a) Recurrence-related factors of temporomandibular joint ankylosis: a 10-year experience. Journal of Oral and Maxillofacial Surgery 77: 2512-2521. [crossref]
- KALPANA T, LAM RM (2021) Clinical study of temporomandibular joint ankylosis & its management. International Journal of Surgery 5: 246-250.
- KAVIN T, JOHN R, VENKATARAMAN S S (2012) The role of three-dimensional computed tomography in the evaluation of temporomandibular joint ankylosis. Journal of Pharmacy & Bioallied Sciences 4: S217. [crossref]
- SHETTY P, THOMAS A, SOWMYA B (2014) Diagnosis of temporomandibular joint (TMJ) ankylosis in children. Journal of Indian Society of Pedodontics and Preventive Dentistry 32: 266-270. [crossref]
- ELGAZZAR RF, ABDELHADY AI, SAAD KA, ELSHAAL MA., HUSSAIN M M., et al (2010b) Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. Int J Oral Maxillofac Surg 39: 333-42. [crossref]
- JAIN G, KUMAR S, RANA AS, BANSAL V, SHARMA P. et al (2008) Temporomandibular joint ankylosis: a review of 44 cases. Oral and Maxillofacial Surgery 12: 61-66. [crossref]
- DANDA A.K, RAMKUMAR S, CHINNASWAMI R (2009) Comparison of gap arthroplasty with and without a temporalis muscle flap for the treatment of ankylosis. Journal of Oral and Maxillofacial Surgery 67: 1425-1431. [crossref]
- BANSAL S, VERMA DK, RAI M, SORAKE A, KAUR C (2019) Gap arthroplasty or interpositional arthroplasty for the management of TMJ ankylosis? A prospective randomized comparative multicenter clinical trial. Journal of Maxillofacial and Oral Surgery 18: 567-571. [crossref]