DOI: 10.31038/PEP.2022311
Abstract
Background: The magnitude of asthma in developing countries increased in 50% per decade for the last 40 years and approximately 250,000 deaths occur in each year. It was the common conditions that affected 5-10% of the population during the past 20 years.
Objectives: The aim of this study was to assess the Prevalence and associated factors of bronchial asthma among adult patients in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali Region, Ethiopia 2020.
Methods: Hospital based cross sectional study design was conducted at Sultan Hassan yabare referral hospital during May-June 2020. Three hundred fifty two (352) patients who visited adult OPD over two months period were included in the study using simple random sampling. The data was checked for completeness, cleaned and then entered into Epi-data version 3.1 then exported to SPSS version 23 for analysis. Bivariate & multivariate binary logistic regression analysis was used to see the associations between bronchial asthma and factors. Adjusted odd ratios were measured at 95% confidence level and P-Value of less than 0.05 was considered significant.
Result: Prevalence of bronchial asthma among adult patients was 9.4%. Being an urban resident (AOR: 3.425:95% CI 1.036-11.319), having family history of asthma (AOR: 5.796: 95% CI 2.31-, 14.540), and presence of vermin in the house (AOR: 2.999: 95% CI 1.106-8.129) were significantly associated with bronchial asthma. The authors concluded that the prevalence of bronchial asthma among adult patients was high. Therefore, educational program about the risk factors and preventive measures of asthma are highly recommended.
Keywords
Adult patient, Bronchial asthma, Shiekh Hassan Yabere Referral Hospital, Jigjiga, Ethiopia
Introduction
Asthma is defined as a “chronic inflammatory disease of the airways” that can cause any or all of the following symptoms: -shortness of breath, tightness in the chest, coughing and wheezing [1]. The chronic inflammation is associated with airway hyper responsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread, but variable airflow obstruction within the lung that is often reversible either spontaneously or with treatment [2].
Asthma imposes a large burden on the individual and on health care systems. Currently, asthma prevalence is approximately 10%-13%globaly. Unexplained temporal and geographic variations in asthma prevalence have been reported with asthma prevalence increasing over the past few decades [3].
In Africa, problems including those arising from the over-utilization of health services, lack of trained staff and diagnostic apparatus, and non-availability and unaffordability of inhaled medications have hindered efforts to improve the management of asthma. The lack of organized health promotion programs, such as effective control strategies for environmental triggers, air pollutants, and occupational dusts have also contributed to the growing burden [4].
WHO has reported that the levels of asthma control and health responses in the continent have been below recommended standards, and that have contributed to the size of the disease burden [4]. In addition, though many African countries have national guidelines for the management of asthma and other CRDs, these guidelines has not been implemented in most rural areas . Economic analyses in many African settings have shown that direct costs from asthma are usually greater than the indirect costs. It has been suggested that education of health care providers and the public is a vital element of the response to the challenge posed by asthma in Africa [4].
The prevalence of asthma in developing countries increased in 50% per decade for the last 40 years and approximately 250,000 deaths occur in each year. It was the common conditions that affect 5-10% of the population during the past 20 years [5].
Bronchial asthma is one of the most common public health problems in Ethiopia. Its prevalence increased over the last few decades with different contributing factor such as cigarette smoking [6], household economic status [7], occupational condition of the patients [7], residence of the patients [8], presence of vermin at household [7] and family history of asthma [9]. It is coming another burden for the country next to those communicable diseases [10]. In one study conducted, in south west Ethiopia, asthma accounted for 2% of outpatient and 5.4% of medical admission [10], and different risk factors are responsible for this problem like poor compliance for the drugs, lack of awareness about the disease, low socio economic status and hyper sensitivity [3].
There is significant physical and socio-economic burden with asthma related health cost. It results is an estimated 420,000 deaths every year [11]. In developing countries, where poverty and non-communicable respiratory disease have long been linked Bronchial asthma is often diagnosed after a long time because of the patients low medical seeking behavior. This may be an important factor for increasing morbidity and mortality as a result of asthma [12,13]. It represents a substantial economic and social burden throughout the world [14]. In developing countries, an additional problem is that health planners have limited resources hence it is one of the factors for emergency department visit [15,16].
The global initiative for asthma (GINA) estimates that the global prevalence of asthma ranges from 1 to 18% [17]. In study conducted in Portugal Prevalence of diagnosed asthma was 5.0% and the ‗Lifetime asthma ‘prevalence was 10.5%. The prevalence was similar in men and women and in all age [18], and another study done In the Kingdom of Saudi Arabia in 2001, the prevalence of asthma was 12% [19]. In Malaysia, it was estimated that there is 1.6 to 2 million asthmatics in 1996 and was leader cause for outpatient visit [20].
Factors that contribute to the bronchial asthma and associated factors among adult patients has not been studied earlier in Somali region. So, the aim of this study was to determine the prevalence and associated factors of bronchial asthma among adult patients in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital.
Methods and Materials
Study Area and Study Period
The study was conducted in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, which is the only referral hospital in the region found in Jigjiga town capital of Somali region. It is located 636 km eastern of Addis Ababa (the capital city of Ethiopia). According to 2007 Central Statistical Agency census report, the projected population of Jigjiga town in 2019 is 166,664 of whom 5267 (3.16%) and 16833 (10%) pregnant women and children aged 6-59 months respectively. The study was conducted from May to June 2020.
Study Design
Institution based cross sectional study design was employed.
Source and Study Population
Source Population
All adult patients who visited adult OPD and adult emergency department of Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital during the study period were source population.
Study population
Randomly selected adult patients who visited adult emergency department and adult OPD of Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital during the study period were study population.
Inclusion and Exclusion Criteria
Inclusion criteria
Adult patients who were visited adult OPD and adult emergency were included in the study.
Exclusion criteria
Patients that were unable to respond or serious illness were excluded from the study.
Sample Size Determination
The sample size was determined using single population formula Assumptions: 95% confidence interval, 5% margin of error and proportion prevalence of bronchial asthma (29.6%) from Debre Berhan ,Ethiopia [7].
![]()
Where: n= the minimum sample size required for the study
Z= standard normal distribution (Z=1.96) with 95% confidence interval
P= prevalence of bronchial asthma (0.296) .(7)
d=is a tolerable margin of error (d=5%=0.05)
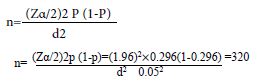
Then by adding 10% (0.1) non-response rate, the total sample size (n) is n=320+ (320×0.1) =320+32=352. Final Sample size is to be 352.
Sampling Techniques and Procedures
Systematic sampling technique was used to select study participants. Jigjiga University Sultan Sheikh Yabere Referral Hospital was selected purposefully. First the average monthly adult patient visiting emergency department calculated which was 1052 adult patient visited Emergency. So eligible patients were recruited using systematic sampling technique. Every K interval calculated i.e. K= 1052 /352=3, so that every third patient was included until the required sample size was achieved. The first patient was taken using lottery method.
Data Collection Tools and Methods
The data was collected using structured questionnaires by interviewing the respondents. The questionnaires was initially prepared in English and then translated into Somali and then back translated into English to check for any inconsistencies or distortion in the meaning of words and concepts. Five Nurse Data collectors and two supervisors were recruited and training was provided on the tools, data collection procedures, the objectives, questionnaires and ways of conducting interview by the principal investigator for two days before the actual data collection time.
Study Variables
Dependent Variable
Bronchial asthma in Adult Patients.
Independent Variables
Socio-demographic factors
- Age,
- Sex,
- Income,
- occupational,
- Family literacy status,
- Residence,
- cost,
Individual behavior and health‑ related condition
- Smoking status
- Co -morbid disease (COPD, Pneumonia, other chronic disease, recurrent URTI
Environmental and housing characteristics of the study participants
- Vermin
Data Quality Control
Data quality was assured through training of data collectors, the questionnaire was evaluated by experts to assess its relevance, and their comments were taken in consideration then questionnaire had pretested on another facility before beginning the actual data collection process and continuous supervision at the time of data collection was conducted. Supervisors together with principal investigator discussed findings of pretest questionnaires checked and modified before the actual data collection. The collected questionnaire was checked in each day on the actual data collection time for completeness and consistency by supervisors and principal investigator. Code was given for completed questionnaire. Double data entry was done to make comparisons of two data clerks and resolve if there was being some difference,
Data Processing and Analyses
The data was coded and entered using Epi-data version 7.2.3.1 then exported, processing and analyzing were done using SPSS version 23. Descriptive statistics of different variables were done by cross tabulation. Binary logistic regression models using bivariate [crude odds ratio, [COR] and multivariable analysis [adjusted odds ratio, AOR] with 95% Confidence interval [CI] were used. From the bivariate analysis, variables that has with a significance level of p<0.25 was being retained for inclusion into the multivariable analysis in the final model. Variables with p<0.05 with being considered as statistically significant and independently associated with bronchial asthma.
Ethical Consideration
An ethical clearance was obtained from Ethics Review Committee of Jigjiga University School of Graduate studies. Written and verbal consent was obtained from each participant after explaining the purpose and nature of the research. Participation in the study was on a voluntary basis and participants were informed their right to quit their participation at any stage of the study if they did not want to continue. Moreover, confidentiality of the information was assured by using an anonymous questionnaire.
Results
Socio-Demographic Characteristics of the Study Participants
Three hundred fifty-two study participants primarily sampled for the study, 340 have participated in the study they made a response rate of 96.7%. The reason for non-response was not willing to participate in the study. The mean age of the study participants was 28.08 with SD of +6.139. The age range of the study participants were 15 and 47 years respectively. One hundred seventy-one (50.3%) males and 169 (49.7%) females were participated in the study. Major ethnic group of this study participant 313 (92.1%) were Somali. About 296 (87.1%) were living in urban and 258(75.9%) were married by their marital status. Most of the study participants 277 (81.7%) were categorized under middle income (Table 1).
Table 1: Distribution of Socio-Demographic Characteristics of the Study Participants in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali region, Ethiopia 2020 G.C.
|
Variable |
Category | Frequency
(No) |
Percentages (%) |
| Age of the patient | 15-24 |
77 |
22.7 |
| 25-34 |
83 |
24.6 |
|
| 35-44 |
78 |
23.1 |
|
| 45-54 |
55 |
16.1 |
|
| >=55 |
46 |
13.6 |
|
| Marital status | 1. Single |
72 |
21.2 |
| 2. Married |
258 |
75.9 |
|
| 3. Divorced |
6 |
1.8 |
|
| 4. Widowed |
4 |
1.2 |
|
| Sex | 1. Male |
171 |
50.3 |
| 2. Female |
169 |
49.7 |
|
| Residence | 1. Urban |
296 |
87.1 |
| 2. Rural |
44 |
12.9 |
|
| Ethnicity
|
1. Somali |
313 |
92.1 |
| 2. Amhara |
17 |
5.0 |
|
| 3. Gurage |
4 |
1.2 |
|
| 4. Others |
6 |
1.8 |
|
| Occupational status | 1. Government employee |
30 |
8.8 |
| 2. Farmer |
57 |
16.8 |
|
| 3. Daily laborer |
61 |
17.9 |
|
| 4. Marchant |
20 |
5.9 |
|
| 5. Others |
172 |
50.6 |
|
| Family income | 1. High |
55 |
16.2 |
| 2. Middle |
277 |
81.5 |
|
| 3. Low |
8 |
2.4 |
Presenting Symptoms
Most of the study participants the commonest presenting asthma symptom was cough reported by 24.4 % of the patients. The second common symptoms were also rhinitis and sinusitis reported by 18.5% and 17.4% of the patients respectively while the least presenting symptoms were atopic dermatitis 13.5% reported by the patients (Table 2).
Table 2: Distribution of presenting symptoms of the Study Participants in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali region, Ethiopia 2020 G.C.
|
Variable |
Category | Frequency (No) |
Percentages (%) |
| Wheezing | 1. Yes |
55 |
16.2 |
| 2. No |
285 |
83.8 |
|
| Cough | 1. Yes |
83 |
24.4 |
| 2. No |
257 |
75.6 |
|
| Dyspnea (shortness of breath) | 1. Yes |
37 |
10.9 |
| 2. No |
303 |
89.1 |
|
| Rhinitis |
1. Yes |
63 |
18.5 |
| 2. No |
277 |
81.5 |
|
| Sinusitis | 1. Yes |
59 |
17.4 |
|
2. No |
281 |
82.6 |
|
| Atopic dermatitis | 1. Yes |
46 |
13.5 |
| 2. No |
294 |
86.5 |
|
| Cyanosis | 1. Yes |
55 |
16.2 |
| 2. No |
285 |
83.8 |
Health Related Characteristics
Among the participants, 37.7% had family history of asthma. Fifty-six (21.8%) of the study participants had an experience of pneumonia in the last 12 months (Table 3).
Table 3: Distribution of health related characteristics of the Study Participants in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali region, Ethiopia 2020 G.C.
|
Variable |
Category | Frequency
(No) |
Percentages (%) |
| Does a patient diagnosis for asthma For now or before? | 1. Yes |
32 |
9.4 |
| 2. No |
308 |
90.6 |
|
| Family history of asthma?
|
1. Yes |
178 |
52.4 |
| 2. No |
162 |
47.6 |
|
| 3. don’t know | |||
| Do you think that is there anything that triggers your asthma?
|
1. Yes |
32 |
9.4 |
| 2. No |
308 |
90.6 |
|
| 3. don’t know | |||
| If yes to Q.no 303, what are your trigger factors that exacerbate your asthma?
|
1. Dust |
4 |
1.2 |
| 2. Smoke |
12 |
3.5 |
|
| 3. Cold weather |
14 |
4.1 |
|
| 4. Strong smell |
2 |
0.6 |
|
|
5. Other (s) |
4 |
1.2 |
|
| Have you ever faced any asthma exacerbation symptoms in the last 12 month | 1. Yes |
32 |
9.4 |
| 2. No |
308 |
90.6 |
|
| 3. don’t know | |||
| Bronchodilators drug utilization |
1. Yes |
155 |
45.6 |
| 2. No |
185 |
54.4 |
|
| Experienced of drug discontinuation | 1. Yes |
15 |
4.4 |
| 2. No |
325 |
95.6 |
|
| History of Chronic diseases like CHD | 1. Yes |
37 |
10.9 |
| 2. No |
303 |
89.1 |
|
| Presence of pneumonia in the last 12 months | 1. Yes |
37 |
10.9 |
| 2. No |
303 |
89.1 |
Individual Behavior
Fifty-four (15.9%) of the study participants were ever smoke cigarette while 38(11.2%) were currently smokers. Among the participants, 24(7.4%) had habit of frequent utilization of perfume and 55(16.2%) had no habit of exercise (Table 4).
Table 4: Distribution of individual behavior of the Study Participants in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali region, Ethiopia 2020 G.C.
|
Variable |
Category | Frequency
(No) |
Percentages (%) |
| Do you ever smoke cigarette?
|
1. Yes |
54 |
15.9 |
| 2. No |
286 |
84.1 |
|
| Are you currently a smoker?
|
1. Yes |
38 |
11.2 |
|
2. No |
302 |
88.8 |
|
| Do you think that is there anything that limits your daily activities?
|
1. Yes |
55 |
16.2 |
| 2. No |
285 |
83.8 |
|
| Is your habit of frequent usage of perfume | 1. Yes |
25 |
7.4 |
| 2. No |
315 |
92.6 |
Environmental Factors
More than half of the study participants 188(55.3%) their house have vermin/dust. Three hundred-ten (91.2%) households used charcoal as source of energy, followed by electricity 6.2%, kerosene 1.5% and wood only 1.2%. Almost all of the study participants 340(100%) reported that did not use biomass fuel (Table 5).
Table 5: Distribution of environmental factors of the Study Participants in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali region, Ethiopia 2020 G.C.
|
Variable |
Category | Frequency
(No) |
Percentages (%) |
| Is there presence of vermin/dust in the home?
|
1. Yes |
188 |
55.3 |
| 2. No |
152 |
44.7 |
|
| How many rooms are there in your house (Including the sitting room)? | 1.>4 rooms |
262 |
77.1 |
| 2.<4 rooms |
78 |
22.9 |
|
| Number of windows in the house | 1. Yes |
119 |
35.0 |
| 2. No |
221 |
65.0 |
|
| With what type of fuel source do you cook at home? | 1. Charcoal |
310 |
91.2 |
| 2. Wood |
4 |
1.2 |
|
|
3. Electricity |
21 |
6.2 |
|
| 4. Kerosene |
5 |
1.5 |
|
| Did you use biomass fuel for work or home? | 1. Yes |
0.00 |
0.00% |
|
2. No |
340 |
100% |
Prevalence of Bronchial Asthma
In this study the overall prevalence of bronchial asthma among adult patients in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital Somali region was found 9.4%with (95%CI: 6.5, 12.9) (Figure 1).
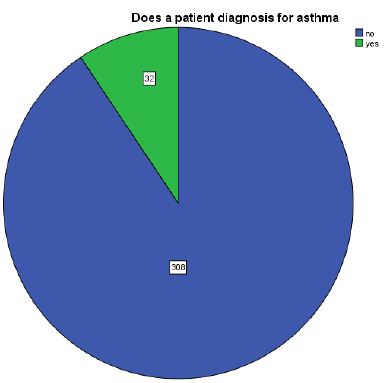
Figure 1: Prevalence of bronchial asthma in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali region, Ethiopia 2020.
Factors Associated with Bronchial Asthma
Bi-variable Analyses on Factors Associated with Bronchial asthma
In the variables included in Bivariate analyses were: Residence, Wheezing, Cough, Dyspnea (shortness of breath), Rhinitis, Sinusitis, atopic dermatitis, Family history of asthma and Presence of vermin/dust in the home.
This study revealed that urban residents were 3.726 times [COR=3.726; 95%CI: (1.274, 10.903)] more likely to develop bronchial asthma than rural residents.
This study indicated that patients who come from the family history of asthma were 6.625 times [COR=6.625; 95%CI: (2.872, 15.280)] more likely to develop bronchial asthma than from non-asthmatic family.
In this study, presence of vermin at household level were 2.694 times [COR=2.694; 95%CI: (1.072, 6.768)] increased the probability of developing asthma among adult patients (Table 6).
Table 6: Bi-variable Analyses for Factors affecting Bronchial asthma among Adult Patients in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali region, Ethiopia 2020.
|
Variable |
Category | Bronchial asthma | COR (95%CI) | P-value | |
| Yes
No (%) |
No No (%) |
||||
| Residence | 1. Urban |
28 (12.2) |
201 (87.8) | 3.726 (1.274, 10.903) | 0.016 |
|
2. Rural |
4 (3.6) | 107 (96.4) |
1.00 |
||
| Wheezing | 1. Yes |
8 (14.0) |
49 (86.0) | 1.762 (0.748, 4.149) | 0.195 |
|
2. No |
24 (8.5) | 259 (91.5) |
1.00 |
||
| Cough | 1. Yes |
11 (13.3) |
72 (86.7) | 1.717 (0.790, 3.730) | 0.172 |
|
2. No |
21 (8.2) | 236 (91.8) |
1.00 |
||
| Dyspnea (shortness of breath) | 1. Yes |
6 (5.2) |
31 (83.8) | 2.062 (0.788, 5.397) | 0.140 |
|
2. No |
26 (8.6) | 277 (91.4) |
1 |
||
| Rhinitis | 1. Yes |
12 (19.0) |
51 (81.0) | 3.024 (1.391, 6.571) | 0.005 |
|
2. No |
20 (7.2) | 257 (92.8) |
1 |
||
| Sinusitis | 1. Yes |
14 (24.7) |
45 (76.3) | 4.546 (2.112, 9.785) | 0.000 |
|
2. No |
18 (5.4) | 263 (93.6) |
1 |
||
| Atopic dermatitis | 1. Yes |
7 (15.2) |
39 (84.8) | 1.931 (0.783, 4.764) | 0.153 |
|
2. No |
25 (8.5) | 269 (91.5) |
1. |
||
| Family history of asthma | 1. Yes |
24 (20.0) |
96 (80.0) | 6.625 (2.872, 15.280) | 0.000 |
|
2. No |
8 (3.6) | 212 (96.4) |
1.00 |
||
| Is your habit of frequent usage of perfume | 1. Yes |
7 (19.4) |
29 (80.6) | 3.756 (1.503, 9.381) | 0.035 |
|
2. No |
25 (7.2) | 279 (91.8) |
1.00 |
||
| Presence of vermin/dust in the home | 1. Yes |
26 (13.6) |
165 (86.4) | 2.694 (1.072, 6.768) | 0.005 |
|
2. No |
6 (4.0) | 143 (96.0) |
1.00 |
||
Multivariable Analyses on Factors Associated with Bronchial asthma
Those variable which had association during bivariate analysis and other candidate variables with P<0.25 in the bivariate analysis were included in the final model of multivariate analysis in order to control all possible confounders. In multivariable analyses, in multivariable logistic regression analysis revealed that sinusitis, residence, family history and vermin/dust were risk factors significantly associated with bronchial asthma.
This study revealed that urban residents were 3.425 times [AOR=3.425; 95%CI: (1.036, 11.319)] more likely to develop bronchial asthma than rural residents.
This study indicated that patients who come from the family history of asthma were 5.796 times [AOR=5.796; 95%CI: (2.311, 14.540)] more likely to develop bronchial asthma than from non-asthmatic family.
In this study, present of vermin at household level were 2.999 times [COR=2.999; 95%CI: (1.106, 8.129)] increased the probability of developing asthma among adult patients.
This study indicated that patients who have sinusitis were 2.971 times [AOR=2.971; 95%CI: (1.193, 7.397)] more likely to develop bronchial asthma than from non-sinusitis (Table 7).
Table 7: Multivariable Logistic Regression Analyses for Factors Bronchial asthma among Adult patients in Jigjiga University Sultan Sheikh Hassan Yabere Referral Hospital, Jigjiga, Somali region, Ethiopia 2020 G.C.
|
Variable |
Category | Dx of Bronchial asthma | COR (95%CI) | AOR (95%CI) | |
| Yes
No (%) |
NO No (%) |
||||
| Residence | 1. Urban |
28 (12.2) |
201 (87.8) | 3.726 (1.274, 10.903) | 3.425 (1.036, 11.319) |
|
2. Rural |
4 (3.6) | 107 (96.4) | 1.00 |
1.00 |
|
| Wheezing | 1. Yes |
8 (14.0) |
49 (86.0) | 1.762 (0.748, 4.149) | 2.240 (0.822, 6.104) |
|
2. No |
24 (8.5) | 259 (91.5) | 1.00 |
1.00 |
|
| Cough | 1. Yes |
11 (13.3) |
72 (86.7) | 1.717 (0.790, 3.730) | 1.597 (0.597, 4.273) |
|
2. No |
21 (8.2) | 236 (91.8) | 1.00 |
1.00 |
|
| Dyspnea (shortness of breath) | 1. Yes |
6 (5.2) |
31 (83.8) | 2.062 (0.788, 5.397) | 1.924 (0.578, 6.400) |
|
2. No |
26 (8.6) | 277 (91.4) | 1 |
1.00 |
|
| Rhinitis | 1. Yes |
12 (19.0) |
51 (81.0) | 3.024 (1.391, 6.571) | 1.847 (0.690, 4.949) |
|
2. No |
20 (7.2) | 257 (92.8) | 1 |
1.00 |
|
| Sinusitis | 1. Yes |
14 (24.7) |
45 (76.3) | 4.546 (2.112, 9.785) | 2.971 (1.193, 7.397) |
|
2. No |
18 (5.4) | 263 (93.6) | 1 |
1.00 |
|
| Atopic dermatitis | 1. Yes |
7 (15.2) |
39 (84.8) | 1.931 (0.783, 4.764) | 1.387 (0.481, 4.002) |
|
2. No |
25 (8.5) | 269 (91.5) | 1 |
1.00 |
|
| Family history of asthma | 1. Yes |
24 (20.0) |
96 (80.0) | 6.625 (2.872, 15.280) | 5.796 (2.311, 14.540) |
|
2. No |
8 (3.6) | 212 (96.4) | 1.00 |
1.00 |
|
| Is your habit of frequent usage of perfume | 1. Yes |
7 (19.4) |
29 (80.6) | 3.756 (1.503, 9.381) | 2.180 (0.724, 6.570) |
|
2. No |
25 (7.2) | 279 (91.8) | 1.00 |
1.00 |
|
| Presence of vermin/dust in the home | 1. Yes |
26 (13.6) |
165 (86.4) | 2.694 (1.072, 6.768) | 2.999 (1.106, 8.129) |
|
2. No |
6 (4.0) | 143 (96.0) | 1.00 |
1.00 |
|
Discussion
In this study the prevalence of Bronchial asthma was 9.4% (95%CI: 6.5, 12.9). This finding is comparable with study conducted in the Kingdom of Saudi Arabia in 2001; the prevalence of asthma was 12 % [19]. This also in line with study done in Africa estimated that a prevalence of 11.7% for asthma, totaling over 74 million people in 1990, and 2010 prevalence was 12.8%, about 120 million people (4). This also in line with study done In Africa the prevalence of asthma was estimated 9.6% in Swaziland, 7.8 in Comoros, 7.54% in Mauritania and in range of 0-10% in Ethiopia [21]. This may be due to similarity of study design and sample size.
This finding is higher than study done in Portugal on Prevalence of asthma which states that the prevalence of diagnosed asthma was 5.0%. This finding is higher than another study done in Addis Ababa which was the prevalence of asthma and factors that lead patients to visit adult emergency room of Zewditu Memorial Hospital, Ethiopia was revealed that the prevalence of bronchial asthma was 1.5% [14].
This finding is lower than study done in Malaysia, 73% out-patient clinic attendants are treated for respiratory symptoms and asthma is one and major cases. It is estimated that there is 1.6 to 2 million asthmatics in Malaysia [20]. This finding is lower than another study done in Addis Ababa which was the prevalence of asthma and factors that lead patients to visit adult emergency room of Zewditu Memorial Hospital, Ethiopia was revealed that the prevalence of bronchial asthma was 1.5% [14]. This finding is also lower than another studies mentioned that (cumulative prevalence of asthma) was highest in South Africa (53%, 5-12 years) in 1997,followed by Egypt (26.5%, 11-15 years) in 2005, Nigeria (18.4%, 15-35 years) in 1995, and Ethiopia(16.3%, >20 years) in 1997.
This study revealed that urban residents were 3.425times [AOR=3.425; 95%CI: (1.036, 11.319)] more likely to develop bronchial asthma than rural residents. It was consistent with the report in Brazil and Ethiopia [15,16]. This might be explained outdoor air of urban area is highly polluted due to high levels of traffic and industry related emissions that could increase the risk of asthma. In contrast, study done in India [17] showed that being a rural resident was significantly higher the odds of having asthma. Research conducted in Ethiopia [18] revealed that no association between asthma and residence of the patients. These variations might be due to the difference in the characteristics of the study population, geographical distribution and case definitions used to ascertain asthma.
Patients having sinusitis were 4.546 times [AOR=2.971; 95%CI: (1.193, 7.397)] more like to encounter bronchial asthma compared to those who have not yet faced this co-morbid. This might be due to the fact that large number of the study subjects live in urban area and in this place there are many chemicals, gases and the like that will worsen the sinusitis status then end up with acute attack. Both seasonal and viral chronic sinusitis are among the most common triggers of acute severe exacerbations and may invade epithelial cells of the lower as well as the upper airways and there is an increase in airway inflammation with increased numbers of eosinophil and neutrophils along with nasal congestion as well as airway tract edema in addition to increment in airway hyper-responsiveness [19,20].
This study indicated that patients who come from the family history of asthma were 5.796 times [AOR=5.796; 95%CI: (2.311, 14.540)] more likely to develop bronchial asthma than from non-asthmatic family. Similar findings have been reported by other studies in developed and developing countries that showed a significant association between family history of asthma and asthma occurrence among adult patients [20,21]. This association could be either due to genetic factors or a shared environment by the family members.
In this study, present of vermin at household level were 2.999 times [AOR=2.999; 95%CI: (1.106, 8.129)] increased the probability of developing bronchial asthma among adult patients. The world health organization report in 2008 report also showed that evidence for a relationship between asthma and domestic exposure to cockroaches, mice and dust mites is strong. This could be explained by house which have vermin’s concerns with the use of insecticides prays at home, with more frequent use being associated with bronchial asthma. Similar results can be found in the literature regarding the link between the use of home aerosolized cleaning products and asthma.
Conclusion
This finding the prevalence of Bronchial asthma was 9.4% (95%CI: 6.5, 12.9). However, Bronchial asthma was significantly associated Type of Residence, Wheezing, Cough, and Rhinitis, Family history of asthma and Presence of vermin/dust in the home was identified as the most important risk factor for Bronchial asthma.
Recommendation
Based on the findings of the study the following recommendations could be mentioned
For Health Professionals
- Health care providers should work on improving patients’ awareness on their medications adherence, avoidance of asthma triggering factors for decreasing the progression of the disease and better asthma controls.
For the Hospital
- Staffs should teach about asthma triggering factors.
References
- Adams JY, Sutter ME (2012) The patient with asthma in the emergency department. Bronchial Asthma: Springer 179-202. [crossref]
- Kirenga J, Okot-Nwang MJAhs (2012) The proportion of asthma and patterns of asthma medications prescriptions among adult patients in the chest, accident and emergency units of a tertiary health care facility in Uganda 12(1): 48-53. [crossref]
- Lawson JA, Janssen I, Bruner MW, Hossain A, Pickett WJBpm (2014) Asthma incidence and risk factors in a national longitudinal sample of adolescent Canadians: a prospective cohort study; 14(1): 51. [crossref]
- Adeloye D, Chan KY, Rudan I, Campbell HJCmj (2013) An estimate of asthma prevalence in Africa: a systematic analysis 54(6): 519-31. [crossref]
- Gupta RS, Weiss KBJP (2009) The 2007 National Asthma Education and Prevention Program asthma guidelines: accelerating their implementation and facilitating their impact on children with asthma. 123(Supplement 3): S193-S8. [crossref]
- Tefereedgn E, Ayana AJOJA (2018) Prevalence of asthma and its association with daily habits in Jimma Town, Ethiopia 2(1): 011-7.
- Shine S, Muhamud S, Demelash AJBrn (2019) Prevalence and associated factors of bronchial asthma among adult patients in Debre Berhan Referral Hospital, Ethiopia 2018: a cross-sectional study. 12(1): 608. [crossref]
- Sharma S, Sood M, Sood AJCPR (2011) Environmental risk factors in relation to childhood asthma in rural area 15(1): 29-32.
- Elfaki N, Shiby AJJCRDC (2017) Risk factors associated with asthma among Saudi adults in Najran 3(133): 2472-1247.1000133.
- Mekonnen D, Andualem MJEjohs (2010) Clinical Effects of Yoga on Asthmatic Patients: A Preliminary Clinical Trial, Jimma, Southwest Ethiopia 20(2). [crossref]
- Asthma GIf. 2018 GINA report, global strategy for asthma management and prevention.
- Aggarwal A, Chaudhry K, Chhabra S, D Souza G, Gupta D, Jindal S, et al. (2006) Prevalence and risk factors for bronchial asthma in Indian adults: a multicentre study 48(1): 13. [crossref]
- Mulat T (2015) Assesment of Prevalence and Pattern of Medication Prescription for Bronchial Asthma, at Adult Emergency Department of Tikur Anbesa Specialsed Hospital. Addis Ababa University.
- Fentahun S (2017) A Study on the Assessement of Prevalance of Asthma and Factors that Lead Patients to Visit Adult Emergency Room Of Zewditu Memmorial Hospital, Addis Ababa. Addis Ababa University.
- Aït-Khaled N, Enarson D, Bousquet JJBotWHO (2001) Chronic respiratory diseases in developing countries: the burden and strategies for prevention and management 79: 971-9. [crossref]
- Hamdan Al-Jahdali AAJB, PUL. MED (2012) Salim bathrooms, factors associated with patients visit to the emergency department for asthma therapy 12: 80. [crossref]
- Amoah AS, Forson AG, Boakye DAJGMJ (2012) A review of epidemiological studies of asthma in Ghana 46(2): 23-8. [crossref]
- Sa-Sousa A, Morais-Almeida M, Azevedo LF, Carvalho R, Jacinto T, Todo-Bom A, et al. (2012) Prevalence of asthma in Portugal-The Portuguese National Asthma Survey 2(1): 15. [crossref]
- Al-Mazam A, Mohamed AGJJof medicine c (2001) Risk factors of bronchial asthma in Bahrah, Saudi Arabia 8(1): 33. [crossref]
- Ngui R, Lim YAL, Chow S, de Bruyne J, Liam CJMJoM (2011) Prevalence of bronchial asthma among Orang Asli in Peninsular Malaysia 66(1): 27-31. [crossref]
- Barry A, Caesar J, Klein Tank A, Aguilar E, McSweeney C, Cyrille AM, et al. (2018) West Africa climate extremes and climate change indices 38: e921-e38. [crossref]