A preoperative evaluation typically includes laboratory testing, imaging studies such as X-ray, computed tomography (CT) scan, electrocardiogram, or echocardiogram to appropriately evaluate the extent of injury, and risk stratification tools such as the Revised Cardiac Risk Index; however, older adults, particularly those with chronic cardiac, pulmonary, or renal multimorbidities may require a more thorough assessment to improve their surgical outcomes [1]. Below is a summary of the different areas of interest in the age-friendly approach to preoperative evaluation organized using the 5M’s Geriatrics Framework, developed by specialists in 2017, to help optimize the care of older adults [1,2].
Mind
It is paramount to accurately establish a patient’s baseline mentation during the preoperative evaluation. By collecting collateral information from caregivers, concerns for underlying cognitive impairment can be more easily identified, which can help define the level of involvement of family members and caregivers needed in the medical decision-making process [3]. It is also important to recognize if a patient is experiencing delirium while conducting the initial interview. Knowing and evaluating a patient’s baseline cognition and screening for delirium informs the patient’s medical decision-making capacity at that point in time, which is vital for obtaining informed consent for surgical procedures [3]. Delirium is an acute and fluctuating state typified by inattention, disorganized thinking, and altered mental status that is classified as hyper- or hypoactive, or mixed [4]. Increased age and cognitive impairment are pre-existing risk factors for delirium. Hospital admission also increases the incidence of delirium, as does acute medical or metabolic issues, being in an unfamiliar environment, lack of sleep or familiar routine, exposure to procedures, diagnostic testing, and anesthesia, prolonged nothing by mouth (NPO) status, and tethering with foley catheters, sequential sleeves, and telemetry (Table 1). Delirium can also prolong hospital stays, increase the likelihood of discharge to nursing homes, and increase morbidity and mortality [1,4,5].
Table 1: List of predisposing and precipitating risk factors for delirium in older adults
| Predisposing Risk Factors for Delirium | Precipitating Risk Factors for Delirium |
| • Age 65 or older
• Male sex • History of delirium • History of cognitive impairment or dementia • Depression • Functional dependence • Immobility • Sedentary lifestyle • History of falls • Sensory impairment • Decreased oral intake • Dehydration • Malnutrition • Medications • Alcohol use • Multiple comorbidities • Chronic renal disease • Chronic hepatic disease • History of stroke • Neurologic disease • Metabolic derangements • Severe or terminal illness • Infection with human immunodeficiency virus |
• Sedative hypnotics
• Narcotics • Anticholinergic drugs • Polypharmacy • Alcohol withdrawal • Drug withdrawal • Stroke • Intracranial bleeding • Meningitis/encephalitis • Infection • Hypoxia • Shock • Fever or hypothermia • Anemia • Metabolic derangements • Surgery • ICU admission • Physical restraints • Foley catheter • Pain or stress • Sleep deprivation |
| Source: Inouye, S.K. Delirium in Older Persons. March 16, 2006. N Engl J Med 2006; 354:1157-1165. DOI: 10.1056/NEJMra052321 | |
The Confusion Assessment Method (CAM) Test is an effective screening tool for delirium. The CAM test evaluates attention using exercises such as reciting the days of the week backward, months of the year backward, or a series of numbers backward, known as the digit span. The UB- 2 Ultra-brief Delirium Screen (Figure 1) is sensitive and specific for diagnosing delirium and takes one minute to perform. If identified, steps should be taken to mitigate delirium, including a thorough review of home medications to identify commonly deliriogenic drugs, regulation and promotion of patient sleep/wake cycles and the implementation of supportive care measures that reiterate frequent reorientation and reassurance.
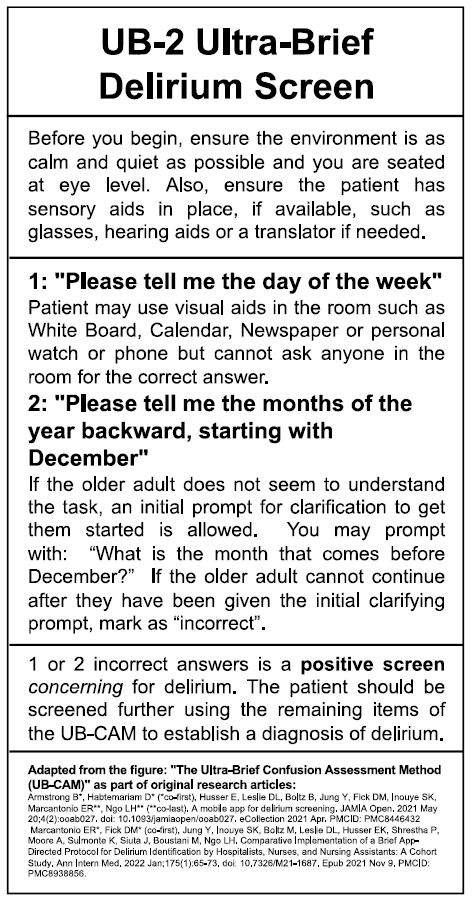
Figure 1: The UB-2 Ultra-Brief Delirium Screen with detailed instructions. The UB-2 Ultra-Brief Delirium Screen is a sensitive and specific screening tool for diagnosing delirium that takes one minute to perform. If the screen is positive, it should be followed by the remaining items of the Ultra-Brief Confusion Assessment Method (UB-CAM).
Because delirium is typically multifactorial in etiology, a multimodal strategy is most effective to mitigate the severity and shorten the duration of the course. Once recognized, patients should be medically optimized (evaluation for metabolic disturbances, infectious causes, and cardiopulmonary distress). Review current medications for not only those that are commonly deliriogenic, as mentioned above, but also for medications that cause withdrawal with abrupt discontinuation, such as gabapentin and benzodiazepines, and attempt to reduce medications when able. A bedside examination is vital to assess for potential stressors (i.e., peripheral intravenous lines, telemetry) and screen for urinary retention and constipation. While hyperactive delirium tends to receive more attention in the hospital, patients with hypoactive delirium tend to have poorer outcomes, and it is estimated that hypoactive delirium is three times more common [4,6]. Therefore, when delirium is identified, a multifaceted non-pharmacological approach should be implemented (Figure 2). Antipsychotic usage to manage the resulting symptoms of delirium, such as agitation, may still occur despite a non-pharmacological approach. Though the literature does not identify one specific antipsychotic that provides optimal treatment for delirium, the brief use of antipsychotics in older patients with delirium may markedly reduce the length of hospital stay and associated healthcare costs [4,6]. However, antipsychotics should be used only if the patient presents a risk of harm to themselves or others.
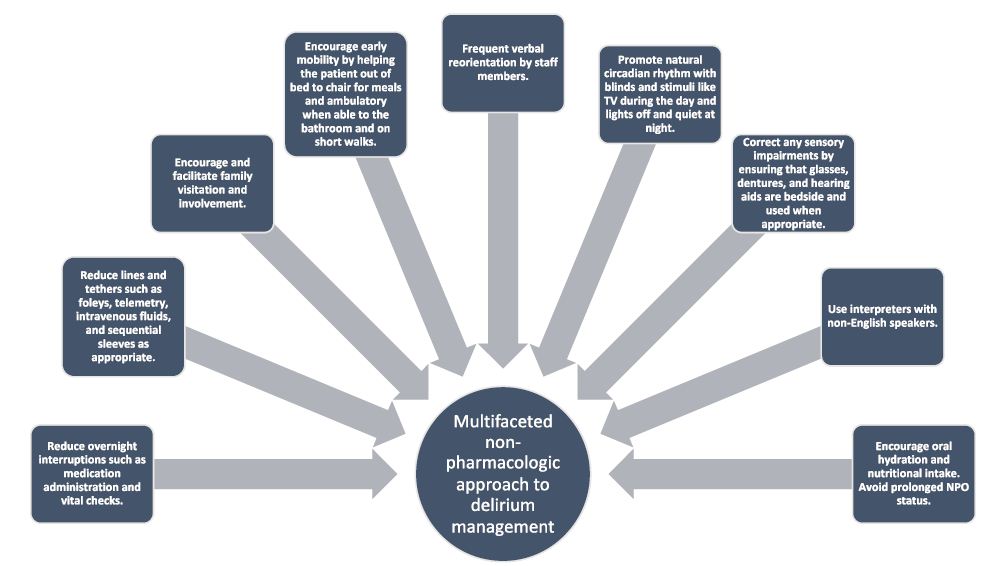
Figure 2: Infographic detailing the multifaceted non-pharmacological approach to older adults identified as having delirium during their hospital course.
Mobility
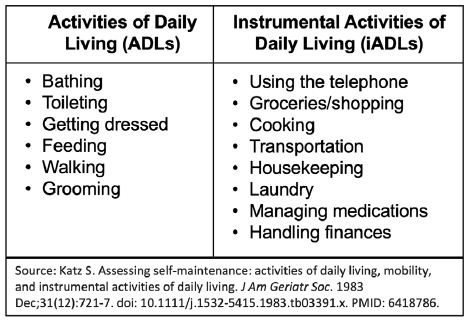
Describing a patient’s functional capacity with an inventory of the Activities of Daily Living (ADLs) and instrumental Activities of Daily Living (iADLs) (Table 2) is a foundational component of the preoperative assessment. In general, iADLs require more cognitive reserve as they require a degree of future planning, safety awareness, executive thinking, and a level of independence. Deficits in iADLs are typically seen before deficits in ADLs in normal aging. However, the rate of loss of function can exponentially increase when a patient has underlying progressive cognitive impairment. In addition to an ADL/iADL inventory, knowing the patient’s dependence on assistive devices (i.e., cane, walkers) and how their home environment is structured (stairs, safety devices such as chair lifts, modifications to bathrooms) help inform successful disposition planning and set realistic expectations with patients and family members regarding the trajectory of one’s recovery that may ultimately require more help or supervision in the home.
Table 2: List of the six (6) Activities of Daily Living (ADLs) and the eight (8) instrumental Activities of Daily Living (iADLs).
Medications and Medical Complexity
As adults age, changes in normal physiology cause the body and brain to be more susceptible to medication’s adverse side effects. Changes in liver and kidney function (Figure 3), specifically, affect the metabolism of medications that can cause reduced clearance, increasing the time a medication lingers in circulation [7,8]. For example, a patient may have poorly controlled hypertension for which they were prescribed two to three antihypertensives for decades – but with aging-driven changes – these dosages may become more potent and lead to hypotension or dizziness. An accurate and comprehensive medication reconciliation, including a list of all current and recently discontinued medications (both prescribed and over-the-counter) with dosing and frequency, when they were started and their indications, how they are taken, and a review of supplements, is integral to every pre-operative evaluation. Similarly, alcohol use and tobacco smoking history should be elicited to prevent alcohol withdrawal and contextualize concern for poor wound healing.
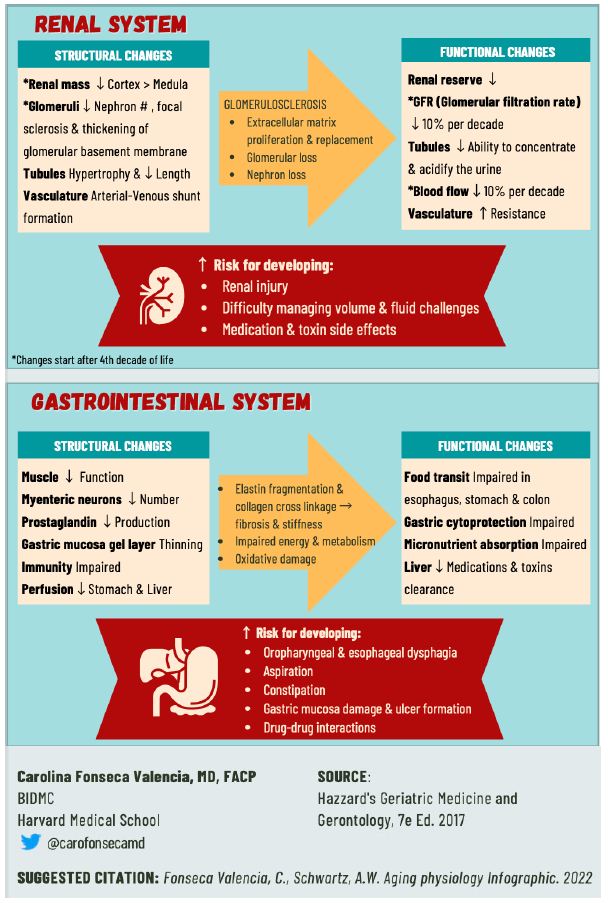
Figure 3: Infographics describing the natural aging of the renal and gastrointestinal systems and how the aging physiology predisposes older adults to medication side effects and drug-drug interactions.
Matters Most
Goals of care fall under the domain of Matters Most, and it encompasses much more than “Code status.” Still, engaging in a meaningful discussion about priorities can be challenging when the patient has suffered a sentinel event or is presented with the stressor of deciding to undergo surgery. Therefore, it is important to document conversations regarding goals of care to share with the care team, such as postoperative expectations and ideal living situation, and complete the necessary paperwork, such as Health Care Proxy forms and orders for life-sustaining treatments [9]. Many older adults may already have pre-existing Do Not Resuscitate (DNR) and/or Do Not Intubate (DNI) advanced directives. In these cases, the Code Status can be suspended perioperatively to ensure adequate support during surgery and acute postoperative care. It is also possible to reverse the Code Status to “Full Code” but avoid cardiac chest compressions, which some older adults and families prefer. SUMMARY A formulaic approach using the 5M’s Geriatric Framework when evaluating the biomedical, functional, mobility, cognitive, and psychosocial domains affecting our older adults can be incredibly useful in capturing all the elements necessary for a comprehensive preoperative assessment. When applied through the lens of aging physiology with the patient and their family’s goals of care in mind, this information can help increase patient safety during the hospital stay, improve surgical outcomes, and reduce the incidence of complications [10-12].
Keywords
Preoperative assessment, Preoperative management, Delirium, Geriatrics, 5M’s, Older adults, aging
References
- McDonald SR.(2022) Perioperative Care: Evaluation and Management. Hazzard’s Geriatric Medicine and Gerontology, 8e. McGraw Hill.
- Tinetti M, Huang A, Molnar F.(2017). The geriatrics 5M’s: a new way of communicating what we do. J Am Geriatr Soc. 65::2115.
- Drickamer MA, Stoneking S.(2022). Assessment of Decisional Capacity and Competencies. Hazzard’s Geriatric Medicine and Gerontology, 8e. McGraw Hill.
- Growdon ME, Mailhot T, Saczynski JS, Fong TG, Inouye SK.(2022). Delirium. Hazzard’s Geriatric Medicine and Gerontology, 8e. McGraw Hill.
- Singler K, Thomas C.(2017). HELP – Hospital Elder Life Program – multimodal delirium prevention in elderly patients. Internist (Berl). 58:125-131.
- Javedan H,Tulabaev S. (2014). Management of Common Postoperative Complications Delirium. Clinics in Geriatric Medicine, 30:271–278.
- Wiggins J, Naik AS, Patel SR.(2022). Aging of the Kidney. Hazzard’s Geriatric Medicine and Gerontology, 8e. McGraw Hill.
- Stanfield D, Benson M, Lucey MR.(2022). Hepatic, Pancreatic, and Biliary Diseases. Hazzard’s Geriatric Medicine and Gerontology, 8e. McGraw Hill.
- Matlock DD, Lum HD.(2022) Decision Making and Advance Care Planning: What Matters Most. Hazzard’s Geriatric Medicine and Gerontology, 8e. McGraw Hill.
- Braithewaite R S, Col NF, Wong JB.(2003). Estimating Hip Fracture Morbidity, Mortality and Costs. J Am Geriatr Soc. 2003;51:364-370.[crossref]
- Grigoryan KV, Javedan H, Rudolph J L.(2014) Orthogeriatric Care Models and Outcomes in Hip Fracture Patients: A Systemic Review and Meta-analysis. J Orthop Trauma. 28: e49-e55.
- Marcantonio E R, Flacker J M, Wright R J, Resnick N M.(2001). Reducing Delirium After Hip Fracture: A Randomized Trial. JAGS. 49:516-522.