Commentary
Most studies focused on electronic health record (EHR) safety, specifically the ability of these systems to detect and prevent adverse drug events (ADEs), has been performed in the inpatient setting. To address this gap, the Ambulatory EHR Evaluation Tool was developed and piloted with seven clinics in 2019. Each of these clinics used one of the leading outpatient EHR systems, as identified by the Office of the National Coordinator (ONC) [1]. The tool consists of a medication safety test and a medication reconciliation module. For the medication safety test, it simulates a physician prescribing medications to their patients. The testing methodology closely follows the inpatient version of the tool, which is administered by the Leapfrog Group. For the medication reconciliation module, clinics were asked to electronically reconcile two medication lists.
To take the medication safety test, clinics downloaded a set of test patients and associated medication test orders to enter into their operational EHR using Computerized Physician Order Entry (CPOE). Included with these test patients were basic demographic details (e.g., age and weight), allergies, and relevant laboratory values. While entering these test orders, licensed prescribers recorded any advice or information they received (if any). The tool assesses basic and advanced decision support features [2]. Once finished with the test, clinics received an overall percentage score of unsafe orders detected, as well as individual order category scores. The test also included two subcategories: nuisance orders and fatal orders. Nuisance orders are low-priority medication combinations (i.e., drug-drug interactions and therapeutic duplications) that should be delivered un-interruptively, as they can contribute to alert fatigue [3]. These orders were reverse scored, in that clinics which alerted on these test orders were scored as “incorrect”. For fatal orders, these were high-priority medication interactions that if prescribed, can lead to serious injury and even death. Lastly, for the medication reconciliation module, we provided clinics with a test patient that was recently discharged from the hospital and is returning to their outpatient clinic for a follow-up visit. Clinics were provided with two medication lists: one from the recent hospitalization, and the most recent ambulatory medication list. These medication lists had the following discrepancies: removal and addition of a medication, and a change in the dose of a medication.
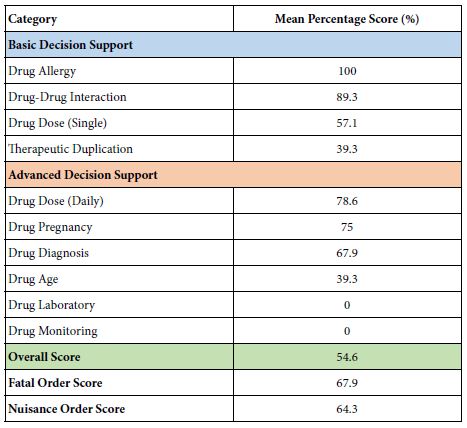
The mean overall score for the medication safety test was 54.6% (Table 1). The range was 42.5%, the minimum score was 37.5%, and the maximum score was 80%. Generally, clinics performed well in areas of basic decision support such as drug allergy (100%), drug-drug interaction (89.3%), drug dose (daily) (78.6%), and drug pregnancy (75%). In contrary, clinics performed poorly in areas of advanced decision support areas like drug age (39.3%). Most alarmingly, none of the clinics in the study had drug laboratory or drug monitoring alerts implemented. In terms of fatal order performance, the mean score was 67.9%. Only one clinic alerted on all the fatal orders in their test. For the nuisance orders, the mean score was 64.3%.
Table 1: Mean percentage scores for each order category
For the medication reconciliation module, three clinics (43%) had an EHR-based medication reconciliation functionality. However, only one clinic (14%) could demonstrate it during the pilot. In addition, none of the clinics’ EHR systems provided CDS during this process. Instead of electronic processes for medication reconciliation, most clinics compared medication lists manually, which was usually performed by a nurse or medical assistant.
The results from the initial pilot of the Ambulatory EHR Evaluation Tool revealed that while basic CDS features like drug allergy and drug interaction checking were widely implemented, areas of more advanced decision support were not implemented. A major commonality between all the clinics was that certain types of alerts were turned off completely. This occurred mostly in advanced decision support areas like drug laboratory, drug monitoring, and drug age; all of which are critical areas for patient safety. In addition, the mean fatal order score was only 68%, which is considered low given the severity of these medication orders. We expected all clinics to score a 100% in this subcategory. In terms of the results of the medication reconciliation module, only one clinic could demonstrate this functionality even though all the clinics were certified through Meaningful Use. Moreover, although most of the clinics understood the importance of medication reconciliation, the electronic processes at their individual facilities were poorly understood and thus unused.
In a broader context, the results from this pilot reveal significant gaps in the implementation of advanced CDS features in the outpatient setting. This is further magnified by the fact that commercial outpatient pharmacies are no longer routinely checking prescriptions for common medication errors, thus leaving the only effective medication safety net at the ambulatory clinic level. This leaves an enormous medication safety gap in the outpatient setting, where most medications are prescribed in the healthcare system. Hopefully, as this tool becomes more widely used, outpatient clinics will use it as a quality improvement tool to assess and identify gaps in the implementation of their medication related CDS, which as of now, is the only critical safety net for outpatient medication use.
References
- Office of the National Coordinator for Health Information Technology. Office-based Physician Electronic Health Record Adoption. Published 2016. Accessed January 11, 2019. https://dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php
- Kuperman GJ, Bobb A, Payne TH, Avery AJ, Gandhi TK, et al. (2007) Medication-related Clinical Decision Support in Computerized Provider Order Entry Systems: A Review. J Am Med Informatics Assoc 14: 29-40. [crossref]
- Phansalkar S, van der Sijs H, Tucker AD, Desai AA, Bell DS, et al. (2013) Drug-drug interactions that should be non-interruptive in order to reduce alert fatigue in electronic health records. J Am Med Informatics Assoc 20: 489-493. [crossref]