Abstract
Background: The hematopoietic stem cell transplant affected the patients’ physical, mental, and spiritual well-being. Taking patients’ needs into account can improve the care experience and alleviate the impact of difficulties during the transplant period. According to the Swedish Patient Act (2014: 821), patients have the right to be involved in their care
Purpose: To describe patients’ subjective experiences, reported in a study specific questionnaire with open-ended questions, when being treated and cared for during autologous hematopoietic stem cell transplantation and to further discuss the importance of person-centred care in a clinical context.
Methods: Sixty-four patients were asked to participate in the study and chose to take part. Fifty-two patients fulfilled the study specific questionnaire (81%). A thematic analysis, was performed with the support of Braun and Clarke, including both inductive and semantic approaches. This is secondary data, part of a larger project evaluating patient experience of safety and security in care during autologous hematopoietic stem cell transplantation regardless of inpatient or outpatient care. The study has a qualitative, pragmatic, comparative design.
Results: Three themes emerged from the analysed data: subjectively perceived positive information and support; subjectively perceived negative information and support; subjective desired increased possibility of person-centred care.
Conclusions: The results of the upcoming study can design new functional tools to support person-centred care in the care of patients undergoing hematopoietic stem cell transplantation or cared for in the haematology department. The results revealed, despite unequally distributed groups, similar subjective experiences of care.
Keywords
Patient, Hematopoietic stem cell transplantation, Person-centred care, Subjective experiences
Introduction
Illnesses requiring hematopoietic stem cell transplantation (hSCT) such as myeloma or lymphoma, require a long-lasting relationship with caregivers. Until now, most high-dose therapy and supportive care while awaiting hematopoietic recovery has been performed entirely in hospital, with a stay of approximately 14 days for autologous hSCT and 30 days for allogeneic hSCT. This can cause a reduction in the patient’s functional capacity and an increased risk of nosocomial infections, particularly relevant for allogeneic transplant patients when they are immunosuppressed [1,2].
Background
The hematopoietic stem cell transplant affected the patients’ physical, mental, and spiritual well-being. Transplantation also had an impact on the patients’ outlook on life and way of thinking. Taking patients’ needs into account can improve the care experience and alleviate the impact of difficulties during the transplant period, thereby improving the experience [3]. Evidence is found on improved health outcomes and quality of life, on enhanced safety and effectiveness and on reduced overall costs and hospital stays, with similar results on overall survival rates comparing both models for autologous and allogeneic patients. It is also stated that the outpatient Hematopoietic Stem Cell Transplantation is a safe practice as well as less costly, it requires fewer days of hospital stay both for autologous and allogeneic transplantations. Incorporating outpatient models could improve the quality of care for people requiring Hematopoietic Stem Cell Transplantation programs [4]. A study showed that most patients treated in hospital in connection with stem cell transplantation were alone during the period of care, no relatives or friends stayed with them, compared to patients who were at home in connection with stem cell transplantation where the majority lived together with close relatives or friends. Almost all patients who were cared for in hospital and who responded to the study-specific questionnaire experienced anxiety during the care period compared to patients who were cared for in the home environment, where the vast majority did not experience any anxiety during the care period [5]. According to the Swedish Patient Act (2014: 821) [6], patients have the right to be involved in their care. Autologous and allogeneic HCT patients are usually grouped in studies, but patients’ experiences and recovery abilities are different [7-10]. Deficiencies in caregivers to focus on patients’ specific psychological, social, and emotional concerns has emerged [11-14].
In a Swedish context, person-centred care is defined as a partnership between patients/relatives and professionals in health care. The starting point is to listen to the patient’s stories, which together with other examinations form the basis for a health plan (https://www.gu.se/gpcc) [15]. In 2020, a European standard for person-centred care was added to ensure patient participation in quality indicators and improvement work in all operational and strategic levels within healthcare (BS EN 17398) [16]. To facilitate and understand the use of person-centred care in a clinical context, the eight principles of patient-centred care is highlighted in research conducted by the Picker Institute and Harvard Medical School (Institute of Medicine (US) Committee on Quality of Health Care in America) [17].
The aim of this study was to describe patients’ subjective experiences, reported in a study specific questionnaire with open-ended questions, when being treated and cared for during SCT and to further discuss the importance of PCC in a clinical context.
Methods
Design
This secondary analysis is part of a larger study [5] and regards patient’s perceived experience of care during autologous hematopoietic stem cell transplantation (SCT) regardless of inpatient (IP) care or outpatient (OP) care. The study has a pragmatic, comparative design.
Theoretical Framework
The practice of caring for patients and their families, Patient-centered care (PCC), includes listening to, informing and involving patients in their care, in ways that are meaningful and valuable to the individual patient. The Institute of Medicine (IOM) defines PCC as: “Providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions” (Institute of Medicine (US) Committee on Quality of Health Care in America) [17].
With the support of focus groups (patients, family members, physicians, and health professionals) and relevant literature, researchers defined eight principles of PCC. Based on the eight principles, the researchers developed the instrument, Picker’s Eight Principles of Patient-Centered care to help and support in care to apply PCC (Institute of Medicine (US) Committee on Quality of Health Care in America) [17] (Figure 1).
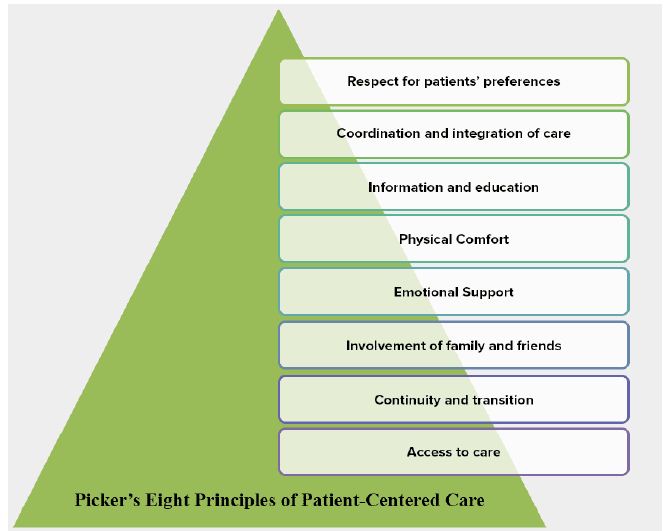
Figure 1: Picker`s Eight Principles of Patient-Centered Care
How to Practise Person-centred Care (PCC)?
A useful framework for how to practise person-centred care (PCC) is Ekman’s conceptual framework, including the three domains of initiate, integrate and safeguard to establish PCC in daily clinical practice to ensure that PCC is systematically and consistently practiced [18]. The framework in this article will be used for a discussion of the study’s results, and therefore further explained here. Initiate – initiating the partnership: patient narratives which means that the patient’s story is the sick one the person’s personal account of his/her illness, symptoms, and its impact on her/his life. It captures the person’s suffering in an everyday context, as opposed to medical narratives such as reflects the process of diagnosing and treating the disease. Our experience is that the patient story is the start for PCC and lays the foundation for a partnership in healthcare. Integrate – Considering the nature of the diseases and the need for overall disease management, it is important that the profession and patients (often also relatives) develop a collaboration to reach jointly agreed goals. At the time of diagnosis, the care team, including the patient, should present and evaluate all aspects of care, considering treatment options tailored to the patient’s lifestyle, preference, beliefs, values, and health concerns. Safeguard – Documenting the patient’s preferences, beliefs, and values as well as his involvement in care and treatment decisions in patient records gives strong legitimacy to the patient perspective. Makes the interaction between patient and caregiver transparent and facilitates continuity of care. Documenting such information must be considered as mandatory as clinical and laboratory findings [18].
Study Setting and Recruitment
Patients diagnosed with myeloma or lymphoma, scheduled for autologous hSCT at a University Hospital in Sweden between February 2017 and February 2019, were consecutively asked to participate. Sixty-four patients were asked to participate in the study and chose to take part. Fifty-two patients fulfilled the study specific questionnaire (81%) (Table 1).
Table 1: Patient characteristics, diagnosis, outpatient and inpatient care
|
Diagnosis |
Myeloma |
Lymphoma |
Total (n=64) |
| Women |
14 |
8 |
22 |
| Men |
30 |
12 |
42 |
| Age, under 60 yrs of age (range 44-60) |
15 |
12 |
27 |
| Age, over 50 yrs of (range 61-71) |
29 |
8 |
37 |
| Outpatient care |
32 |
10 |
42 |
| Inpatient care |
12 |
10 |
22 |
Inclusion and-or Exclusion
Inclusion criteria were age ≥18 years and diagnosed with myeloma or lymphoma and planned for hSCT. The patients would also understand the Swedish language in speech, reading and writing. Exclusion criteria were whether the patient did not meet the requirements for OP care during hSCT.
Data Collection
Data were collected from a previous study published in Journal of Nursing & Care. An invitation to participate in the study was given to the patients when they were enrolled in the University hospital in Sweden, for autologous hSCT during the period February 2017 to February 2019. Information about the study was received at enrollment and the patients had the opportunity to ask questions about the content of the study. The patients who chose to join the study gave their consent in writing. The patients answered the study specific questionnaire at discharge [5].
Data Analysis
For demographic data descriptive statistics were used (Table 1). The answers from the open-ended questions were transcribed verbatim by the two authors. Guided by the aim of the study, the authors independently read all the material several times. A thematic analysis, was performed with the support of Braun and Clarke, including both inductive and semantic approaches [19]. First, with the support of the study’s aim the authors independently read all the study questionnaires several times. Second, all substantial features in the text were assigned a code, with all relevant data collected under the same code. Third, codes were deployed into tentative themes. Before entering the fourth step, data from questionnaires were added into the analysis by performing steps 1 to 3. Fourth, themes were evaluated by going back to the codes and the transcribed text. A thematic map was produced to visualise the analysis. Fifth, themes were defined and labelled, i.e. continued analysis and refinement of the specific content and definitions of each theme (Figure 1). Finally, the result report was written, with quotes exemplifying the raw data (Figure 2).
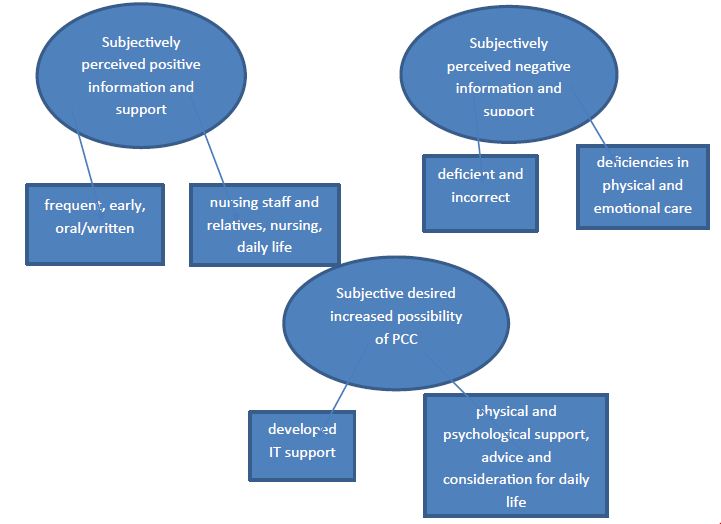
Figure 2: Final thematic map, showing final three themes and six subthemes
Ethical Consideration
The study rests on the ethical principles; World medical association declaration of Helsinki [20]. The study was approved by the regional Research Ethics Committee, Uppsala, D no; 2016/521.
Results
Three themes emerged from the analysed data: subjectively perceived positive information and support; subjectively perceived negative information and support; subjective desired increased possibility of PCC.
Subjectively Perceived Positive Information and Support
Patients (IP and OP) reported that they were satisfied with information in connection with their planned hSCT. The information was given early and frequently both orally and in writing. Patients expressed it important to have time to understand and prepare any accompanying relatives for a long-term stay in an apartment if the care environment was outside the hospital. The perceived support of caring by nursing staff and relatives regarding daily life, for example nutrition and activity, was assessed as safe and secure.
“Positive experience of information by post with the summons and upon admission”. (IP)
“Good with both oral and written information because you forget a lot with oral information” (IP)
“Good to have time to understand the information and prepare any accompanying relatives for a long-term stay in an apartment” (OP)
“I had close relatives with me who cooked and made sure I ate even when it was problematic” (OP)
“I received all the support I needed by nurses, but the illness meant I couldn’t eat. Absolutely nothing wrong with the food”. (IP)
Subjectively Perceived Negative Information and Support
Patients (IP and OP) reported that they were unsatisfied with information in connection with their planned hSCT. The information was sometimes incomplete and incorrect. The patient’s subjective experience of support from healthcare professionals and relatives was sometimes perceived as unsatisfactory both with reference to healthcare hygiene and psychosocial support.
“Got some different information in the written booklet. Got 2 different ones” (OP)
“However, information was lacking” (IP)
“Some nurse was a little too busy. If you can’t eat, you can’t” (IP)
“During the three weeks I was in the ward, no one asked how I was feeling mentally, which is an important part of care. It must not be forgotten” (IP)
“The hardest thing when you were alone was shopping and cooking when you felt sick and nothing tasted good. Then there was no support from the nursing staff” (OP)
Subjective Desired Increased Possibility of Person Centered Care (PCC)
Several wishes regarding care during hSCT were expressed by both patients in IP and OP care to increase the possibility of PCC. Patients indicate that they wish to be listened to and to be informed and involved in their care, in ways that are meaningful and valuable to them. To be able to achieve optimal PCC, there was a request for developed IT support. The patients raised requests for increased physical and psychological support as well as nutrition and physical activity advice about daily life.
“Above all, support from the care staff when walking – a shorter turn – as I was unsure how much I could handle” (IP)
“Opportunity to control wishes around food. For example, change lunch/dinner to yogurt or sour milk” (IP)
“When the needle in the port à cat was to be inserted, no one asked if I wanted pain patches first. I had to tell the nurses all the time”. (IP)
“Using modern technology for communication is great “a department xxx channel” on TV with the possibility to see the person you are talking to can partly replace visits” (OP)
“Better information about how I handle food and exercise when I’m discharged and have to fend for myself” (OP)
“I lacked proper information about how weak and tired you would become after the stem cell transplant” (OP)
Discussion
The themes emerged from the analysed data: perceived information and support; desired increased possibility of PCC is in accordance with the Swedish Patient Act (2014: 821) [6] that highlights patients right to be involved in their care. The patients in this study have experienced deficiencies in psychological, social, and emotional concerns, which is in line with previous studies [11-14].
Shared decision-making is based on the trust of the partnership between patient and caregiver. The patient story is the first step in establishing a partnership with the patient. Documentation in patient records not only highlights the value of this story, but also contributes to the continuity and transparency of the partnership between provider and patient [18]. The results show that patients regardless IP or OP care felt a need for developed PCC. It was highlighted that information about diet and activity such as PCC was not paid attention to in hSCT care and that support to independently exercise in daily physical activities and communication around food and drink is not prioritized.
The three domains of initiate, integrate and safeguard to establish PCC in daily clinical practice [18] could be a help to establish PCC in the care of patients undergoing hSCT. This initially requires an effort by nursing staff and care planners, which in the long run can give the patient an experience of security and to feel supported by the care staff in being at home during a large part of the care period. Initiation captures the patient’s own story about the perceived condition and the subjective suffering in an everyday context, unlike the medical story that describes the diagnosis and treatment of illness The patients’ subjective experiences differ on certain points between IP and OP care environments. There is, however, very little difference in how they experience some shortcomings in the desired support from the health care staff. Integration means developing cooperation between the patient and care to achieve jointly agreed goals. The care team should, in collaboration with the patient and any relatives, describe all aspects of the care, considering treatment options adapted to the patient’s lifestyle, preferences, beliefs, values and health problems. It can be a challenge for healthcare to find instruments to facilitate the practice of PCC and a support for patients and healthcare practitioners to follow a thought pattern within PCC. Safeguard includes documenting the patient’s story in the patient record as the beginning of a good PCC and describes the patient’s participation in care and treatment decisions, which gives strong legitimacy to the patient’s own will. This leads to transparency between patient and care provider and facilitates continuity of care. The Institute of Medicine (IOM) defines PCC as: “Providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions” (Institute of Medicine (US) Committee on Quality of Health Care in America) [17]. As patients today are often alone when staying in the care unit during hSCT and some patients in home care, planning for PCC is needed to strengthen the patient’s self-care possibilities. To facilitate the introduction and maintenance of PCC by healthcare professionals, the instrument, Picker’s eight principles of patient-centered care to help and support in care, can be used. With respect to quality-of-life results, in the autologous studies, the psychological, physical, social, and financial well-being has been reported with higher scores in the outpatient model [21]. This is in accordance with the previously published study [5] regarding anxiety. It was estimated lower in patients treated in hospital (IP). Thru the introduction of PCC, patients can experience increased security in care regardless of the form of care, which can also lead to improved health economics.
Strength and Limitations of the Work
This is a study where the patient’s own voice comes to the fore. Response participation in the study was high, which may indicate patients’ need to be able to express subjective experiences about care. The study is easy to apply as there is a study-specific questionnaire prepared for the specific patient group undergoing hSCT. The results of the study may be helpful in developing PCC in the care of patients undergoing hSCT
A limitation with this study could be the small sample size and the uneven distribution of the groups where patients treated in hospital (IP) were fewer than in the outpatient group (OP). Another limitation is that only one university hospital out of a possible six was involved in the study.
However, patients in this study shared both positive and negative experiences about their period of care, which may indicate that they provided honest and reflective written input in the study-specific questionnaire. The results can be of importance as it gives an insight into patients’ subjective experience of care.
Recommendations for Further Research
More participating university hospitals is needed for a larger base of patients which may lead to improved PCC for patients undergoing hSCT. Complement the study-specific questionnaires with in-depth interviews to capture more subjective experiences to help strengthen PCC. Interview healthcare professionals to strengthen transparency in conversations when caring for patients undergoing hSCT. Overall, the results of the present study may form the basis for the design of new functional tools to support PCC in the care of patients undergoing hSCT or cared for in the hematology department.
Conclusion
Taken together, the results of the upcoming study can design new functional tools to support PCC in the care of patients undergoing hSCT or cared for in the hematology department. The results revealed, despite unequally distributed groups (IP and OP), generally similar subjective experiences of the care context the patient was in. Patients indicate that they want to be listened to and informed and involved in their care, in a way that is meaningful and valuable to them. To achieve optimal PCC, there was, for example, a desire for developed IT support. Previous experiences of PCC in hSCT care have not been exposed within a care context, which together with the desire for developed transparency between patient and care provider should benefit health care leaders.
Relevance to Clinical Practice
To maintain and ensure the patient’s rights according to the Swedish Patient Act (2014: 821), patients have the right to be involved in their care. Therefore, the results from this study can be a help for health care professionals to gain an insight into how patients subjectively describe experiences of care today when they undergo hSCT at a university hospital in Sweden. This might promote the healthcare provider’s intention to introduce PCC based on the patient’s own qualifications. As a routine during patient enrolment, patient-nurse-physician conversations should include Ekman’s conceptual framework, including the three domains of initiate, integrate, and ensure, to guarantee that PCC is practiced systematically and consistently. Caring for patients undergoing hSCT is and should be a team effort in which dietitians and physiotherapists have an obvious place. Using an instrument such as Picker’s eight principles of patient-centered care can facilitate the team.
Statements and Declarations
Authorship
Design: ACS, AEW; Data collection and drafting the manuscript: ACS, AEW; Data analysis: ACS, AEW; Critical reviewing the manuscript: ACS, AEW. All authors approved the final version of the manuscript.
Funding
The authors declare that no funds, grants, or other supports were received during the preparation of this manuscript.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical Consideration
The study rests on the ethical principles; World medical association declaration of Helsinki [20]. The study was approved by the regional Research Ethics Committee, Uppsala, D no; 2016/521
Consent to Participate
Written informed consent was obtained from all individual participants included in the study.
Consent to Publish
A statement confirming that consent to publish has been received from all participants.
Conflict of Interest
The authors declare no conflict of interest.
References
- Owattanapanich W, Suphadirekkul K, Kunacheewa C, Ungprasert P, et al. (2018) Risk of febrile neutropenia among patients with multiple myeloma or lymphoma who undergo inpatient versus outpatient autologous stem cell transplantation: a systematic review and meta-analysis. BMC Cancer 18: 1126. [crossref]
- Svahn BM, Ringde´n O, Remberger M (2005) Long-term follow-up of patients treated at home during the pancytopenic phase after allogeneic haematopoietic stem cell transplantation. Bone Marrow Transplant 36: 511-516. [crossref]
- Alnasser Q, Abu Kharmah SD, Attia M, Aljafari A, et al. (2018) The lived experience of autologous stem cell-transplanted patients: Posttransplantation and before discharge. J Clin Nurs 27: e1508-e1518. [crossref]
- Gonza´lez MJ, Urizar E, Urtaran-Laresgoiti M, Nuño-Solinı´s R, et al. (2021) Hospital and outpatient models for Hematopoietic Stem Cell Transplantation: A systematic review of comparative studies for health outcomes, experience of care and costs. PLoS ONE 16: e0254135. [crossref]
- Svanberg, Anncarin,Alexandra Eilegård Wallin (2022) Patients’ Subjective Experiences of Outpatient- and Inpatient Care during Autologous Hematopoietic Stem Cell Transplantation – A Quantitative Questionnaire Study. J Nurs Care 11: 562.
- Patient Act, SFS 2014: 821 (2015)
- Pidala J, Anasetti C, Jim H (2009) Quality of life after allogeneic hematopoietic cell transplantation. Blood 114: 7-19.
- Luebbert K, Dahme B, Hasenbring M (2001) The effectiveness of relaxation training in reducing treatment-related symptoms and improving emotional adjustment in acute non-surgical cancer treatment: a metaanalytical review. Psychooncology10: 490-502. [crossref]
- Packman W, Weber S, Wallace J, Bugescu N (2010) Psychological effects of hematopoietic SCT on pediatric patients, siblings, and parents: a review. Bone Marrow Transplant 45: 1134-1146. [crossref]
- Baliousis M, Rennoldson M, Snowden JA (2016) Psychological interventions for distress in adults undergoing haematopoietic stem cell transplantation: a systematic review with meta-analysis. Psychooncology 25: 400- 411. [crossref]
- Beattie S, Lebel S (2011) The experience of caregivers of hematologic cancer patients undergoing a hematopoietic stem cell transplant: a comprehensive literature review. Psychooncology 20: 1137-1150. [crossref]
- Gemmill R, Cooke L, Williams AC, Grant M (2011) Informal caregivers of hematopoietic cell transplant patients: a review and recommendations for interventions and research. Cancer Nurs 34: E13-E21.[crossref]
- Bevans M, Wehrlen L, Castro K, Prince P, et al. (2014) A problem-solving education intervention in caregivers and patients during allogeneic hematopoietic stem cell transplantation. J Health Psychol 19: 602-617. [crossref]
- Laudenslager ML, Simoneau TL, Kilbourn K, Natvig C, et al. (2015) A randomized control trial of a psychosocial intervention for caregivers of allogeneic hematopoietic stem cell transplant patients: effects on distress. Bone Marrow Transplant 50: 1110-1118. [crossref]
- https: //www.gu.se/gpcc
- Patient involvement in healthcare – Minimum requirements for person-centred care (CEN/TC 450)
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001. PMID: 25057539)
- Ekman I, Swedberg K, Taft C, Lindseth A, et al. (2011) Person-Centered Care — Ready for Prime Time. European Journal of Cardiovascular Nursing 10: 248-251.
- Braun V, Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3: 77-101.
- World Medical A (2013) World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. JAMA 310: 2191-4. [crossref]
- Ferna´ndez-Avile´s F, Carreras E, Urbano-Ispizua A, Rovira M, et al. (2006) Case-Control Comparison of At-Home to Total Hospital Care for Autologous Stem-Cell Transplantation for Hematologic Malignancies. J Clin Oncol 24: 4855-4861. [crossref]