DOI: 10.31038/CST.2018345
Abstract
The paper introduces a case study aiming to answer the question of what concerns healthy people about the prospect of cancer? The results suggest two distinct mind-sets. The mind-set is Life-Quality Pursuers, who are concerned the result is temporary and think cancer is chronic disease. The second mind-set is Outcome-Worriers, who fear the outcome, and worry about no recovery. The Outcome-Worriers are concerned a lot about physical pains and symptoms like nausea and joint pain. Incorporating the results of Mind Genomics and the mind-sets into a short, online personal viewpoint identifier, permits the use of these scientific results to assign a new patient to one of the two mind-sets. The benefit is the ability to better communicate information and instructions to the patients, based on the nature of the messages to which they are like to be most receptive.
Keywords
Mind Genomics; segmentation; regression analysis; hospitalization; hospital services
Introduction
Fields of services have been quickly adopting personalization, recognizing the power behind personal messages. Hospital services offer a great possibility to personalize patient experience, in turn increasing hospital satisfaction and personal experience. Mapping patients’ needs and finding the best messages for different groups (or mind-sets) might seem a complex and difficult task, but has been made much simpler and quicker through a technology, Mind Genomics, originally designed for consumer products and services. Mind Genomics uses experimental design of ideas to map the mind of a given population and identify profoundly different mind-sets, requiring different messaging and person-to-person interactions.
The patient experience is becoming a focus of medical science [1]. The world of evidence-based research is a fact of life, but the medical establishment is beginning to acknowledge what individual practitioners have known from time immemorial. That knowing the patient’s value, preferences, emotional pre-disposition (i.e. mind-set) are important for patient collaboration leading to improved clinical outcomes [2, 3].
Interacting with patients in today’s medical environment presents challenges to both well- seasoned and inexperienced physicians. Unlike the previous generation, there exists a new paradigm of the patient-physician relationship which involves parties that very often have not established a history with each other. For the most part, the days of “knowing” your patient intimately have passed. Physicians in the primary care environment have limited time resources to interact with their patients. In the usual 15 minute time slot the practitioner must address the patients concerns, which may turn out to be different and even more important than why the visit was scheduled in the first place. The practitioner needs to become a negotiator, prioritizing the issues and making sure that issues the patient values are addressed, not only to meet the patient’s expectations but also to integrate the relationship paradigm within the comfort zone of the physician’s practice philosophy.
Unlike other chronic health concerns, the issues surrounding receiving a diagnosis of cancer compound the physician/patient interaction and bring it to the highest level, involving both the emotional and technical aspects of medicine. No physician wants to deliver the news that their patient has cancer. As mentioned above, the construct of today’s environment adds to the stress on both sides of the issue. In the historic, Marcus Welby, model of care the physician intimately knows his patient and has the advantage of knowing how they may react to the news. They may know how to break the news in a personalized way. In today’s more impersonal medicine, the interaction may be taking place between relative strangers.
The Contribution of Mind Genomics
One of the emerging issues is to understand the mind of the patient. Beyond this understanding of the patient who has the disease is to understand the mind of a patient anticipating a disease, or anticipating a new treatment. What do people think about when they are entering a course of treatment, or when they are contemplating the results of a test, or even of a doctor’s visit? Can science help understand the mind of patients and what to say and what not to say to the patient?
Mind Genomics, addresses how a particular mindset thinks thereby adding finesse to the situation. The doctor may not know his patient very well, but he now has a glimpse into how that patient thinks, into what is important to that patient and into what the patient fears from. Bad news can now be broken to the patient in a tailored manner allowing a balanced presentation that addresses biological concerns and psychosocial concerns.
Recent developments using principles of experimental psychology and marketing science suggest that one ought to consider approaches that are used to understand how people make decisions. Decision making in life consists of looking at a composition of messages, a compound message, and from this compound identify what is important, and respond to that which is important [4]. In other words, the newly emerging science posits that the traditional scientific method of isolating one variable, and exploring that one variable, simply will not work. The person exposed to this one-at-a-time test can change the response criterion, either in a conscious way to be politically correct, or in an unconscious way to avoid painful or embarrassing responses.
The results reported here are part of a larger effort to understand how to communicate with individuals, either before they become cancer patients, while they are patients, or after they have been patients. The research effort is modeled after the method of experimental design of ideas, so-called Mind Genomics. The ingoing premise is that one can understand the mind of the patient, and avoid politically correct ratings, by presenting the patients with combinations of messages, doing so quickly in order to prevent the respondent from responding in a considered, so-called rational fashion, but a fashion which may have little or nothing to do with the honest feelings. The Nobel Laureate in economics, Daniel Kahneman of Princeton University calls the intuitive approach ‘System 1 Thinking,’ to be distinguished from the more rational, more analytical way of thinking, which he calls ‘System 2 Thinking’ [5].
Cancer has long inspired fear as it is viewed as an unpredictable and external threat [6]. Despite advances in early diagnosis and treatment a third to half of the general population in the United States and United Kingdom say they fear cancer more than they fear any other disease [7]. Many people report experiencing significant cancer worry [8]. In a British study, participants worried about the threat to life and the emotional upset that a diagnosis would cause. Half of participants would worry about surgery, radiotherapy, chemotherapy, and loss of control over life. Worries about the social consequences were less common but about a half thought they would worry about financial problems or their social roles, and a quarter would be worried about effects on identity, important relationships, gender role, and sexuality. Women and younger people reported they would be more worried about the emotional, physical, and social consequences of a cancer diagnosis [9]. Cancer fears related to perceptions of proximity; strategies to keep the enemy at bay; the emotional, physical, and social implications of disease; and dying [10]. Thus, cancer fear consists of various interrelated fears. Cancer illness may be perceived as incapacitation and death resulting in different fears of cancer.
To date, there is no comprehensive understanding of the various fears and which messages to use with people when diagnosed with cancer. This study is in response to calls to understand what evokes fear of cancer in order to measure cancer fear, to allay counterproductive fears, or to encourage adaptive behaviors in those who may be deterred by their fears [10]
Usually researchers design a single question type of survey when collecting respondent’s point of view about a certain problem. This traditional scientific method of isolating one variable, and exploring that one variable, may not give us the right results, particularly when studying attitudes towards cancer.
The underlying rationale of Mind Genomics is based on conjoint analysis. Conjoint analysis enjoys a history with cancer studies, and so the world-view of testing compound messages should not be strange in research. The reader is referred to previously work using conjoint measurement to study responses to cancer: [11–20].
Mind-Genomics is based in part upon the notion that it is better to use the type of information presented to people in their daily lives. This information comprises a compound, incorporating many different types of messages which communicate different, but related information about a topic. Mind Genomics works with these ‘compound messages.’ These compound messages, also called vignettes, can be thought of as comprising a series of answers to unwritten but guiding questions. When used properly by researchers and even by younger students, the Mind Genomics exercise becomes, in turn, an extremely powerful way to teach critical thinking.
Mind Genomics features a number of statistical properties which allow it to uncover the mind of people in an efficient manner, hard-to-fake. The experimental design ensures that the elements appear in a manner making them statistically independent of each other. The independence of the components of the vignette, the individual messages or elements, allows for the deconstruction of the responses by statistical methods such as ordinary least-squares regression. Regression uncovers the contributory power of each element. Each test stimulus comprises a number of different messages, with the test stimulus, the vignette, presenting stimuli that must be reacted to at an ‘emotional and ‘intuitive’ level. It is simply impossible to ‘select the correct answer’ since so many parts of the vignette are varying simultaneously.
The experimental design used by Mind Genomics comprises a basic or ‘kernel’ design. The structure of the design is fixed. The underlying mathematical structure of the experimental design is maintained from respondent to respondent. The only thing which changes is the particular combination that the respondent evaluated. The change is effected by a permutation scheme, a method which allows the different sets of vignettes to cover a very wide range of combinations [18, 19]
Our goal is to collect responses to vignettes, with the responses reflecting their feelings about the problem in question. The design of Mind Genomics studies focuses on both feeling and thinking, incorporating the ways we process information [5]. Feeling, the real focus of Mind Genomics, is part of what Kahnemann calls System 1 (brain’s fast, automatic, intuitive approach) that is influential, guiding and steering System 2 (mind slower, analytical mode where reason dominates).
Method
The study was designed as a preliminary evaluation of the types of messages which might be relevant to, or appeal to, people who had not yet been diagnosed with a disease, but people who were aware of the disease. We used the Mind Genomics to quantify the impact of each element, and to test the possibility that there would exist different mind-sets about the disease within a group of randomly chosen individuals, not necessarily suffering from a disease. This approach differs from the more conventional research method, which works with targeted populations, those who already suffer from the condition or disease. We were trying to look at the general population ahead of such a situation.
Mind Genomics works by presenting respondents with different messages. The messages are simple, easy-to-understand combinations of words, painting a word picture. Mind Genomics begins by creating the raw material, silos or questions, which are general categories of messages dealing with different aspects of the patient, the lifestyle, the disease, and the treatment, respectively. In this study we created six such silos, or six questions which ‘tell a story.’ Each silo or question then requires six alternative answers or ‘elements,’ which paint a word picture. Table 1 presents the six different silos (questions), and the six elements (answers, messages) for each silo. [4, 19]
Table 1. The six silos (questions) and the six elements (answers) for each silo.
|
|
Silo (Question) A – What aspect of daily living do you worry that you will lose? |
|
A1 |
Be able to perform daily routine physical activity… walking…sleeping…eating… |
|
A2 |
Be able to cook for yourself and family |
|
A3 |
Be able to take the moderate physical work |
|
A4 |
Be able to spend time with family and friends |
|
A5 |
Be able to play and enjoy physical activity… gardening…bicycling… |
|
A6 |
Be able to fall to sleep fast |
|
|
Silo (Question) B – What aspects of your social life do you worry that you will lose? |
|
B1 |
Enjoy cultural activity…sharing ideas…maintain social life. |
|
B2 |
Enjoy the time interacting with friends |
|
B3 |
Keep the sense of well-being |
|
B4 |
Perceived self-independence in daily life |
|
B5 |
Feel emotional balance… |
|
B6 |
Perceived autonomy in daily life…go shopping without assistance… |
|
|
Silo (Question) C – What physical aspect of yourself do you want to maintain? |
|
C1 |
Your hair keeps same amount as before intaking the medicine |
|
C2 |
Your skin looks flushing |
|
C3 |
Your weight is in the balanced range |
|
C4 |
Your finger nails color looks better |
|
C5 |
Your new hair starts to come back |
|
C6 |
Special tattoo marked survival… |
|
|
Silo (Question) D – What health issues do you think about or worry about? |
|
D1 |
Worry about no recovery |
|
D2 |
Expect full recovery |
|
D3 |
Remission might happen |
|
D4 |
Feel you are borrowing time by taking the medicine |
|
D5 |
Knowing the result is temporary |
|
D6 |
Thinking cancer is a chronic disease… |
|
|
Silo (Question) E – What discomforts do you think about or worry about? |
|
E1 |
Experience HEADACHE after intaking the medicine and treatment |
|
E2 |
Experience NAUSEA after intaking the medicine and treatment |
|
E3 |
Experience FATIGUE after intaking the medicine and treatment |
|
E4 |
Experience JOINT PAIN after intaking the medicine and treatment |
|
E5 |
Experience STOMACH ACHE after intaking the medicine and treatment |
|
E6 |
Experience MUSCLE PAIN after intaking the medicine and treatment |
|
|
Silo (Question) F – What aspects do you think about with respect to your family? |
|
F1 |
Bring the Sadness to family |
|
F2 |
Fear of the outcome |
|
F3 |
Seek Compassion from family members |
|
F4 |
Seek Empathy from family members |
|
F5 |
Ask family members’ help with chores, such as cooking… cleaning…shopping… yard work… |
|
F6 |
Attached to family emotional support |
The actual experiment takes place with the respondent interacting with a computer screen. The screen introduces the topic, and instructs to read the each of 48 screens, and rate the screen as a totality on a rating scale shown below the screen. The 48 screens comprise different combinations of the elements, combined according to an experimental design. The design specifies the combinations, ensuring that the elements are statistically independent of each other, and that each element appears five times in the set of 48, and is absent 43 times. The experimental design creates 36 combinations, vignettes, comprising four elements from different silos, and 12 combinations comprising three elements from different silos. A silo could either be absent from a vignette, by design, or contribute at most one element. Finally, each respondent evaluated a unique set of 48 vignettes, allowing the set of elements to cover a wide ‘space’ (space-filling) in the set of alternative combinations. Figure 1 presents an example of a 4-element vignette.
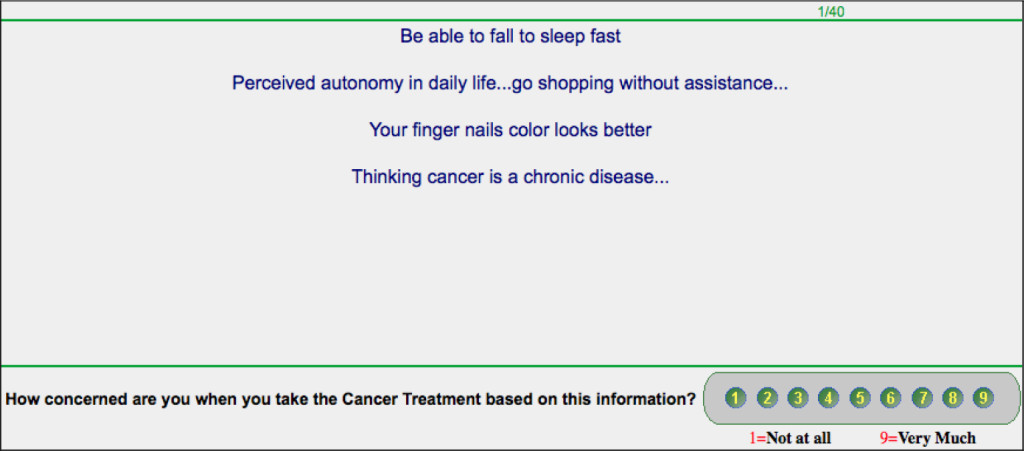
Figure 1. An example of a 4-element vignette. The respondent was instructed to read the entire vignette or combination of elements as a single entity, and rate the combination as a single entity.
The study was conducted with Amazon’s Turk, a service which allows respondents to participate, and keeps the cost of the research low [13, 20]. Amazon Turk has been used extensively for research of this type, where there is no physical intervention.
The respondents who agreed to participate clicked the embedded link in their invitation email. The respondent was the led to the experiment, which begin with the following text on their screen:
Being diagnosed with cancer will most likely have an effect, physically and emotionally. We understand these challenges, and are dedicated to providing a holis tic treatment to help people who face cancer. We need you help to understand what concerns you during your cancer experiences.
You will be presented with short descriptions of things which might happen during the cancer treatment, and will be asked to rate the description on the basis of your concern:
1 = Not at all … 9 = Very much
Each description is unique, although it may appear similar to another one. Just rate each one and move on to the next. After you complete rating the descriptions, you will be asked questions for analysis purposes. Your answers are confidential, and they will not identify you in any way. They will not be used for any purpose or shared.
Thank you for participating in our study of cancer treatment. Your answers will help us better understand your physical and emotional concerns. Your answers are anonymous, and will not be used for any other purpose.
Analysis of the ratings
The data from the study comprises 41 sets of 48 rows of numbers. Each set of 48 rows, one set of 48 per respondent, comprises the respondent’s identification number, then 36 columns corresponding to the coding of the 36 elements as either absent (the number 0 in the cell), or present (the number 1 in the cell). The final column is the rating assigned by the respondent to the particular vignette or combination of elements.
Managers have a difficult time understanding the ‘meaning’ of a rating scale, often asking ‘where on the scale is the most important region?’ In order to accommodate their concerns for understanding, we transform the ratings, with ratings of 1–6 transformed to the number ‘0’ and ratings of 7–9 transformed to the number ‘100.’ This transformation loses some of the granular information, but in the end, the transformation of the 9-point Likert scale into a binary scale makes the interpretation of the results far easier for the user, and thus promotes the use of structured experiments to answer problems. The final transformation simply adds a very small random number (<10–5) to the transformed numbers, so that the binary scale of 0/100 is really a distribution of numbers near 0 and 100, respectively. This transformation has no effect on the results after modeling, but ensures that the OLS (ordinary least-squares) regression will always work.
We run OLS regressions for each respondent. We can do that because the up-front experimental design created the combinations or vignettes for each respondent. The data can be analyzed at the level of each respondent. Furthermore, the systematic permutation of the basic design ensure that we are not simply testing the same set of 48 combinations, but really taking different ‘snapshots’ from various angles. The appropriate simile here is the different ‘pictures’ taken by the MRI.
The model generated by OLS regression is expressed by the simple linear equation:
Binary Response = k0 + k1(A1) + k2(A2)…k36(F6)
The additive constant, k0, tells us the conditional probability of the respondent being concerned (rating the vignette 7–9) in the absence of elements. By the ingoing design, all the vignettes comprised 3–4 elements. The additive constant is an estimated value. It gives us a sense of the probability that a respondent would be concerned about cancer, even in the absence of elements.
Each element has a coefficient. The coefficient tells us the additive probability value that a combination would enjoy were the element to be inserted into the combination or vignette. The coefficient adds to the additive constant to produce a sum. Thus, a coefficient of +7 tells us that when the element is inserted into a vignette, the vignette will enjoy an additional 7% of the respondents rating it 7–9. Thus, were we to begin with the additive constant of 35 (35% probability of worrying), and then insert an element with a coefficient of +5 (e.g., Be able to perform daily routine physical activity… walking…sleeping…eating...), we would expect the percent of respondents who worry to increase from 35% to 40% (35 + 5). We can add or in some cases subtract with negative coefficients, for a total of four unrelated elements in a vignette.
Table 2 shows the data for the total panel sorted by the coefficient. Respondents clearly show a range of concerns.
Table 2. Performance of the 36 elements by total panel. The elements are ranked in terms of the size of the coefficient.
|
|
|
Total Sample |
|
|
Base size |
41 |
|
|
Additive constant |
35 |
|
D1 |
Worry about no recovery |
16 |
|
E2 |
Experience NAUSEA after intaking the medicine and treatment |
15 |
|
F2 |
Fear of the outcome |
14 |
|
F5 |
Ask family members’ help with chores, such as cooking… cleaning…shopping… yard work… |
13 |
|
D5 |
Knowing the result is temporary |
11 |
|
D4 |
Feel you are borrowing time by taking the medicine |
11 |
|
F1 |
Bring the Sadness to family |
10 |
|
E1 |
Experience HEADACHE after intaking the medicine and treatment |
10 |
|
E4 |
Experience JOINT PAIN after intaking the medicine and treatment |
8 |
|
E6 |
Experience MUSCLE PAIN after intaking the medicine and treatment |
8 |
|
D6 |
Thinking cancer is a chronic disease… |
7 |
|
E3 |
Experience FATIGUE after intaking the medicine and treatment |
7 |
|
F3 |
Seek Compassion from family members |
6 |
|
E5 |
Experience STOMACH ACHE after intaking the medicine and treatment |
5 |
|
D2 |
Expect full recovery |
5 |
|
A1 |
Be able to perform daily routine physical activity… walking…sleeping…eating… |
5 |
|
F6 |
Attached to family emotional support |
5 |
|
B2 |
Enjoy the time interacting with friends |
4 |
|
C5 |
Your new hair starts to come back |
4 |
|
C2 |
Your skin looks flushing |
4 |
|
B1 |
Enjoy cultural activity…sharing ideas…maintain social life. |
3 |
|
C1 |
Your hair keeps same amount as before intaking the medicine |
3 |
|
D3 |
Remission might happen |
3 |
|
A2 |
Be able to cook for yourself and family |
2 |
|
C4 |
Your finger nails color looks better |
2 |
|
A4 |
Be able to spend time with family and friends |
2 |
|
B5 |
Feel emotional balance… |
1 |
|
B6 |
Perceive autonomy in daily life…go shopping without assistance… |
1 |
|
A5 |
Be able to play and enjoy physical activity… gardening…bicycling… |
0 |
|
B3 |
Keep the sense of well-being |
0 |
|
B4 |
Perceived self-Independence in daily life |
0 |
|
F4 |
Seek Empathy from family members |
–1 |
|
A3 |
Be able to take the moderate physical work |
–1 |
|
C3 |
Your weight is in the balanced range |
–1 |
|
A6 |
Be able to fall to sleep fast |
–3 |
|
C6 |
Special tattoo marked survival… |
–3 |
- The additive constant is 35. This means that in the absence of specific elements which add ‘meaning’ to the vignette, the likelihood is about a 1/3 of the respondents will say that they are concerned. In fact, simply saying the word ‘cancer’ does not immediately result in ‘concern.’ It is the specifics which drive the rating beyond the low starting value of 35.
- The nature of the issue, i.e., the ‘meaning’ of the message is what is important.
- The most dramatic issue, understandably, is that the respondent feels that there will be no recovery.
- The other key fears involve nausea (dealing with one’s own discomfort), having to ask the family to help (dealing with one’s independence, and being at the mercy of others.)
- Phrasing the concerns in terms of specifics (e.g. asking family members’ help with chores..) is more anxiety provoking in terms of concerns than phrasing the same concern, but without painting a ‘word picture’ (e.g., seek empathy from family members.)
- We conclude that it is both topic and language. We further conclude that it is specifics rather than generalities. Painting a word picture is more effective in driving concern than using general language. This is an important result to keep in mind when working with patients, to understand and to ameliorate their concerns.
Mind-sets
Table 2 reveals that some elements are more effective in driving concern, whereas other elements are less effective in driving concern. Table 2 also reveals that even among the strong-performing elements, there are differences in the nature of the elements which drive concern, namely those elements with high coefficients, e.g., +10 or higher. Previous efforts using Mind Genomics to study responses to meaningful issues suggest that across a wide spectrum of issues those elements with coefficients around 10 or more are likely to correspond to relevant aspects of one’s actual experiences. This value 10 is not fixed in stone, but rather a region of coefficients which covary with other measured behaviors. In some other studies, the region of important may begin with coefficients around 8 or higher.
One of the tenets of Mind Genomics is that there exist in the population different groups of ideas which are held by individuals. These are equivalent, at least metaphorically, to gene alleles. The ideas move together, and are held by a single individual. Through experiments such as the one reported here, we can get a sense of which ideas co-vary. Furthermore, a person is likely to have one set of ideas, or one mind genome, and not have another.
The mind genomes, here called mind-sets, are extracted from the array of data using the standard statistical methods known as cluster analysis. Each respondent generates 36 coefficients, one coefficient for each of the 36 elements. We estimate these 36 coefficients because the 48 combinations, the vignettes for each respondent, were created according to an experimental design, allowing us to the estimate the individual coefficients.
Keep in mind that the clustering is a heuristic. There are many variants of clustering, and no ‘right answer.’ Rather, the objective is to divide a set of objects into two or more groups which are more homogeneous than the original complete set. Our criteria for arriving at the final group of mind-sets for a single data source is to extract as few clusters or mind-sets as possible (parsimony), while at the same time making sure that the strongest performing elements in each cluster or mind-set ‘tell a story’ (interpretability.)
The clustering algorithm defines a distance between each pair of respondents, (1 – Pearson R). The Pearson R or correlation coefficient varies from a high of +1 when two variables are perfectly related (and thus distance = 0), to a low of -1 when two variables are perfectly, but inversely related (and thus the distance = 2.)
The clustering suggested that we need only two mind-sets, i.e., two clusters, to account for the strong performing elements. Table 3 shows these strong performers for each group, and the elements which fail to perform well, i.e., are of no concern to either mind-set.
Table 3. Performance of the elements for mind-sets 1 (Life-Quality Pursuer) and mind-set 2 (Outcome-Worrier).
|
|
|
Total Sample |
Life- Quality Pursuer |
Outcome-Worrier |
|
|
Base size |
41 |
22 |
19 |
|
|
Additive constant |
35 |
37 |
33 |
|
|
Mind-Set 1 – Life-Quality Pursuer |
|
|
|
|
D5 |
Knowing the result is temporary |
11 |
13 |
8 |
|
F1 |
Bring the Sadness to family |
10 |
13 |
8 |
|
D6 |
Thinking cancer is a chronic disease… |
7 |
11 |
4 |
|
B2 |
Enjoy the time interacting with friends |
4 |
10 |
–3 |
|
F2 |
Fear of the outcome |
14 |
10 |
18 |
|
F5 |
Ask family members’ help with chores, such as cooking… cleaning…shopping… yard work… |
13 |
10 |
16 |
|
|
Mind-Set 2 – Outcome Worrier |
|
|
|
|
D1 |
Worry about no recovery |
16 |
9 |
25 |
|
E2 |
Experience NAUSEA after intaking the medicine and treatment |
15 |
8 |
24 |
|
E4 |
Experience JOINT PAIN after intaking the medicine and treatment |
8 |
–2 |
20 |
|
F2 |
Fear of the outcome |
14 |
10 |
18 |
|
F5 |
Ask family members’ help with chores, such as cooking… cleaning…shopping… yard work… |
13 |
10 |
16 |
|
E1 |
Experience HEADACHE after intaking the medicine and treatment |
10 |
5 |
17 |
|
E3 |
Experience FATIGUE after intaking the medicine and treatment |
7 |
–2 |
17 |
|
E6 |
Experience MUSCLE PAIN after intaking the medicine and treatment |
8 |
2 |
14 |
|
D4 |
Feel you are borrowing time by taking the medicine |
11 |
9 |
13 |
|
E5 |
Experience STOMACH ACHE after intaking the medicine and treatment |
5 |
–1 |
11 |
|
|
Not strong for either mind-set |
|
|
|
|
F3 |
Seek Compassion from family members |
6 |
5 |
7 |
|
D2 |
Expect full recovery |
5 |
1 |
8 |
|
A1 |
Be able to perform daily routine physical activity… walking…sleeping…eating… |
5 |
4 |
5 |
|
F6 |
Attached to family emotional support |
5 |
6 |
3 |
|
C5 |
Your new hair starts to come back |
4 |
1 |
8 |
|
C2 |
Your skin looks flushing |
4 |
6 |
2 |
|
B1 |
Enjoy cultural activity…sharing ideas…maintain social life. |
3 |
5 |
1 |
|
C1 |
Your hair keeps same amount as before intaking the medicine |
3 |
4 |
1 |
|
D3 |
Remission might happen |
3 |
6 |
–1 |
|
A2 |
Be able to cook for yourself and family |
2 |
1 |
3 |
|
C4 |
Your finger nails color looks better |
2 |
2 |
2 |
|
A4 |
Be able to spend time with family and friends |
2 |
2 |
1 |
|
B5 |
Feel emotional balance… |
1 |
2 |
–1 |
|
B6 |
Perceive autonomy in daily life…go shopping without assistance… |
1 |
7 |
–5 |
|
A5 |
Be able to play and enjoy physical activity… gardening…bicycling… |
0 |
2 |
–4 |
|
B3 |
Keep the sense of well-being |
0 |
4 |
–5 |
|
B4 |
Perceive self-Independence in daily life |
0 |
4 |
–5 |
|
F4 |
Seek Empathy from family members |
–1 |
2 |
–4 |
|
A3 |
Be able to take the moderate physical work |
–1 |
1 |
–4 |
|
C3 |
Your weight is in the balanced range |
–1 |
3 |
–5 |
|
A6 |
Be able to fall to sleep fast |
–3 |
–1 |
–4 |
|
C6 |
Special tattoo marked survival… |
–3 |
0 |
–6 |
Mind Set 1 – Life-Quality Pursuer: They are concerned the result is temporary, and think cancer is chronic disease. They care about their family’s feelings and worry about bringing sadness to their family. More important is that with the understanding cancer is a chronic disease, they still want to preserve quality of life in the long-term treatment process. They are concerned about being able to maintain the sense of well-being, and the ability to enjoy the time with friends. To perceive autonomy in daily life is still important to them; they want to be able to go shopping without assistance. They care whether they are betrayed by appearance; e.g., their faces look flushed. They are less concerned about the pains and other symptoms during the treatment.
Mind-Set 2 – Outcome-Worrier: They worry about no recovery and fear the outcome. They are concerned a lot about physical pains and symptoms like nausea and joint pain. They also have some concerns of coping with family when ask for help. But they care less about perceived autonomy in daily life. They do not care about appearance and self-independence. It is not their concern whether or not they are still able to preserve the quality of life and keep the sense of well-being when they take the cancer treatment
Understanding the ‘new patient’ – Personal Viewpoint Identification
The foregoing material establishes the science. We now imagine the very common situation of a person presenting symptoms, who is diagnosed with cancer. How might the communication be improved beyond the sterile clinical information, and perhaps beyond the standard information conveyed to patients about what might be expected? We might imagine that were we to know the mind-set to which the presenting patient belongs, the communications can be fine-tuned in light of what we believe to most concern the person. The person who can be identified as to membership in a mind-set can receive the information to allay the fears.
One way to use the information about mind-sets creates a personal viewpoint identifier, a short questionnaire, perhaps comprising 4–8 simple questions, answered with an easy-to-use scale (disagree versus agree.) The pattern of responses to this short questionnaire can be scored to assign the person to one of the two mind-sets. The scoring can be done quickly at the time of the initial testing, or can be done as part of an annual patient checkup, by a doctor or a health plan / health insurer.
The rest of this section shows the application of the PVI, the personal viewpoint identifier.
The obtained coefficients express the extent of concerns with an element. This information enables us to find the most discriminating elements, e.g. those which differ the most between the mind-sets. After transforming the difference between the coefficients to a binary scale (e.g. not concerned and very concerned), we created a short, online-based system in order assign new respondents to one of the two mind-sets previously discovered.
Note: The PVI for this study is available online at the following link http://162.243.165.37:3838/TT01/
The welcome screen introduces the project, and the task, furthermore any kind of identification option can also be inserted (Figure 2). In order to avoid order effect, the order of the questions is randomly assigned for each participant. In this given case, e-mail address is used but any other identification number, code or character string can also be used depending on the institution using the system. After answering all five question, the classification is done by pressing the Submit button.
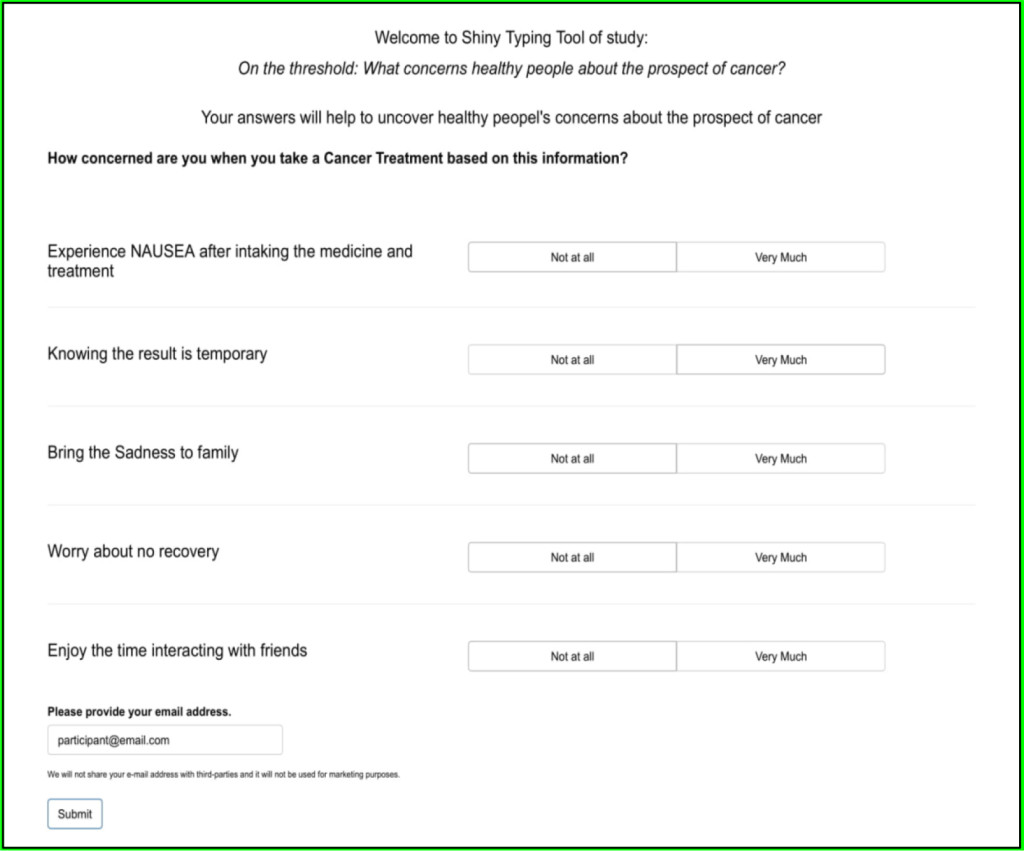
Figure 2. Welcome screen of the 5-question personal viewpoint identification tool. Participants are instructed to answer the binary questions and to add their e-mail address.
In the next step (Figures 3A and 3B), the medical staff and/or participants see a result screen, showing their mind-set membership and a short introduction of the given mind-set. This screen can also be changed, e.g. mind-set membership may be presented only to the doctor, with the participant simply receiving a thank-you message. The system records the chosen options and final mind-set membership. Applying the PVI to patients in the hospital or to health group members reveals the nature of memberships in the general population, and can be correlated with outcomes and with patient ratings of their experience.
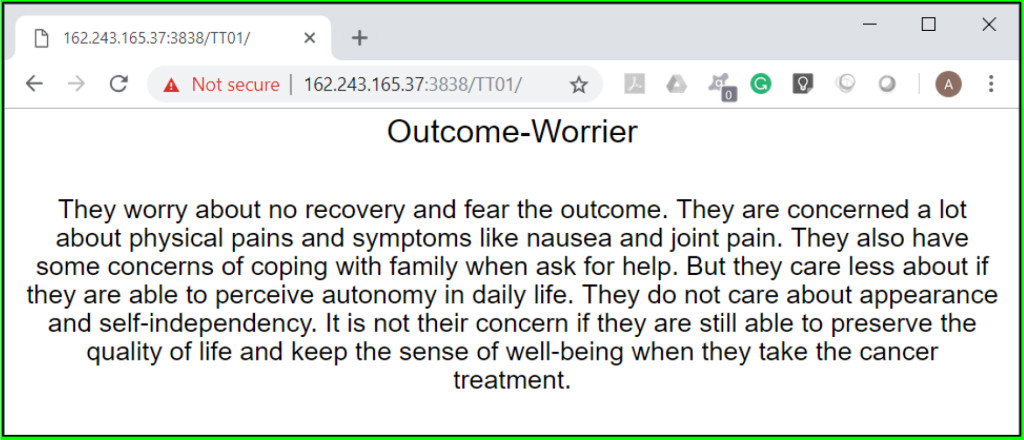
Figure 3A. Result screen of the personal viewpoint identification for a respondent whose ratings on the PVI assign the respondent to the Outcome-Worrier mind-set.
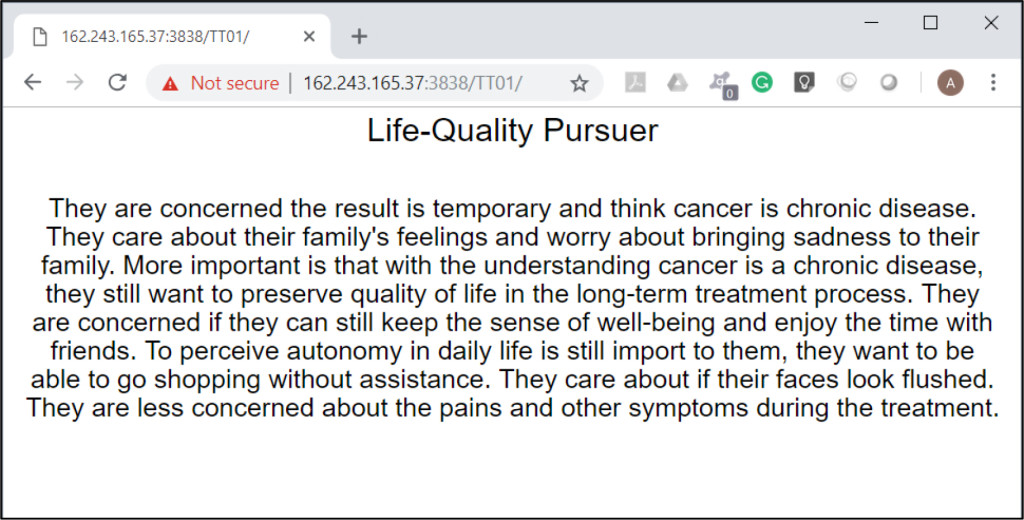
Figure 3B. Result screen of the personal viewpoint identification for a respondent whose ratings on the PVI assign the respondent to the Life-Quality-Pursuer mind-set.
Discussion
In this study we introduced a case study aiming to answer the question of what healthy people fear about the prospect of cancer? We used the conjoint based science of Mind-Genomics to identify psychographic mindsets. We uncovered two distinct mind-sets. One mindset comprises life-quality pursuers, who are concerned the consequences of cancer are temporary, they perceive cancer as a chronic disease. The second mindset comprises outcome-worriers who worry about no recovery and fear the outcome of death. They are concerned with physical pains and symptoms like nausea and joint pain.
Findings answer a lingering question regarding fears of cancer which to date was conceptualized as consisting of various interrelated fears. This study contributes to closing this gap by establishing an understanding of various fears by mindset segments, and outlining messages clinicians may use while communicating with people in each segment throughout the diagnosis process or when diagnosed with cancer.
The ‘bottom-line’ is that Mind Genomics allows clinicians to target the right messages with each person concerned regarding cancer by person’s belonging to one of the mindsets. Knowing the right psychographic messages before saying a word gives an undoubtedly huge advantage to doctors shaping effective communication and improving outcomes and well-being [3, 21]
Conclusions
Effective communication enhances patient collaboration, enhances patient adherence and promotes outcomes, life quality and well-being. Using the right communicative behavior, clinicians may be able to deter patient fears, build trust and encourage adaptive behaviors throughout the treatment process. Our findings may assist oncologists to easily provide patients with a balanced presentation that addresses both the System 1 concerns and the System 2 concerns garnered from the information gathered from the patient’s Viewpoint Identifier (VPI).
Acknowledgements
Author Attila Gere thanks the support of the Premium Postdoctoral Research Program of the Hungarian Academy of Sciences
References
- Ryan M, Kinghorn P, Entwistle VA, *Francis JJ (2014) Valuing patients’ experiences of healthcare processes: towards broader applications of existing methods. Social Science & Medicine 106: 194–203.
- Gabay G (2015) Perceived control over health, communication and patient-physician trust. Patient Educ Couns . S0738-3991: 30007–0 [crossref]
- Arbuthnott A, Sharpe D (2009) The effect of physician–patient collaboration on patient adherence in non-psychiatric medicine. Patient Education and Counseling 77: 60–67.
- Gabay G, Moskowitz HR, Silcher M, Galanter E (2017) Mind Genomics: The New Novum Organum: Policy, Perceptions and Emotions in Health. Pardes Academic Publishing
- Kahneman D (2011) Thinking, Fast and Slow. Macmillan. ISBN 978-1-4299-6935-2
- Vrinten C, McGregor LM, Heinrich M, von Wagner C, Waller J, et al. (2017) What do people fear about cancer? A systematic review and meta-synthesis of cancer fears in the general population. Psychooncology 26: 1070–1079. [crossref]
- Vrinten C, McGregor LM, Heinrich M, von Wagner C, Waller J, et al. (2017) What do people fear about cancer? A systematic review and meta-synthesis of cancer fears in the general population. Psycho-oncology 2016: 1070–1079.
- Vrinten C, Waller J, von Wagner C, Wardle J (2015) Cancer fear: facilitator and deterrent to participation in colorectal cancer screening. Cancer Epidemiol Biomarkers Prev 24: 400–405.
- Moser RP, McCaul K, Peters E, Nelson W, Marcus SE (2007) Associations of perceived risk and worry with cancer health-protective actions: data from the Health Information National Trends Survey (HINTS). J Health Psychol 12: 53–65. [crossref]
- Murphy PJ, Marlow LAV, Waller J, Vrinten C (2018) What is it about a cancer diagnosis that would worry people? A population-based survey of adults in England. BMC Cancer 18: 86. [crossref]
- Bridges JF, Mohamed AF, Finnern HW, Woehl A, Hauber AB (2012) Patients’ preferences for treatment outcomes for advanced non-small cell lung cancer: A conjoint analysis. Lung Cancer 77: 224–231.
- Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, et al. (2011) Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value in Health 14: 403–413.
- Buhrmester M, Kwang T, Gosling SD (2011) Amazon’s Mechanical Turk: A New Source of Inexpensive, Yet High-Quality, Data? Perspect Psychol Sci 6: 3–5. [crossref]
- Marshall D, Bridges JF, Hauber B, Cameron R, Donnalley, et al. (2010) Conjoint analysis applications in health—how are studies being designed and reported? The Patient: Patient-Centered Outcomes Research , 3: 249–256.
- Pignone, Michael P, Brenner AT, Sarah Hawley, Stacey L, et al. (2012) Conjoint analysis versus rating and ranking for values elicitation and clarification in colorectal cancer screening. Journal of general internal medicine 27: 45–50.
- Ryan M (1999) Using conjoint analysis to take account of patient preferences and go beyond health outcomes: an application to in vitro fertilisation. Social science & medicine 48: 535–546.
- Ryan M, Farrar S (2000) Using conjoint analysis to elicit preferences for health care. BMJ 320: 1530–1533. [crossref]
- Gabay G, Moskowitz HR (2012) The algebra of health concerns: implications of consumer perception of health loss, illness and the breakdown of the health system on anxiety. Inter j of cons studies 36: 635–646.
- Gofman A, Moskowitz H (2010) Isomorphic permuted experimental designs and their application in conjoint analysis. Journal of Sensory Studies 25: 127–145.
- Beusterien K, Grinspan J, Kuchuk I, Mazzarello S, Clemons M, et al. (2014) Use of conjoint analysis to assess breast cancer patient preferences for chemotherapy side effects. The Ocologist 19: 127–134.
- Gabay G (2016) Exploring perceived control and self-rated health in re-admissions among younger adults: A retrospective study. Patient Education and Counseling 99: 800–806.
- Costa MLV, Ribeiro KDCB, Machado MAC, Costa ACLV, Montagnini AL (2006) Prognostic score in gastric cancer: the importance of a conjoint analysis of clinical, pathologic, and therapeutic factors. Annals of surgical oncology 13: 843–850.