Clinical Image
Neurosarcoidosis is known as the involvement of the central nervous system in sarcoidosis, usually affects patients between 30 and 40 years of age, more predominantly in women. It can affect different organs such as the lung, lymph nodes, eyes, joints and more rarely (5% of cases) the central nervous system, which manifested with a clinical and radiological polymorphism that makes the diagnosis more difficult. Clinical symptomatology is very variable, rarely isolated without systemic sarcoidosis involvement, and in some cases the diagnosis is made only based on imaging data; if signs are present, they would be related to the type of intracranial involvement (leptomeningeal, pachymeningeal, parenchymal, pituitary stalk, etc.): headaches (hydrocephalus), endocrine signs of hypothalamic or pituitary involvement: diabetes insipidus, optic nerve involvement, facial nerve palsy, general signs: Tiredness, joint pain [1].
The diagnosis is difficult and relies on the Association of clinical and paraclinical arguments. The main ones are magnetic resonance imaging, cerebrospinal fluid study, intradermal tuberculin reaction, phosphocalcic and angiotensin-converting enzyme evaluation. MRI identified lesions present an iso or hyperintense signal in T1 signal, variable signal in T2, hypo signal diffusion with high ADC, are intensely and homogeneously enhanced after injection, and may involve a single or several compartments [2].
Pachymeninge
Thickening of the pachymeninges, which is most often in hyposignal, T2 enhances homogeneously.
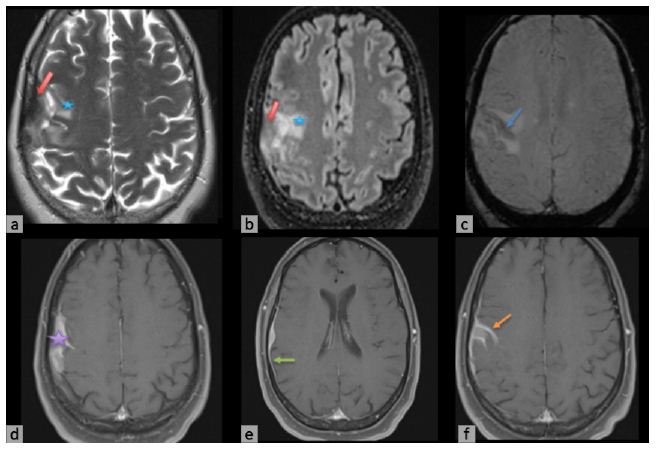
Figure 1: Brain MRI in a 56-year-old woman, partial left convulsive seizure for 3 months, shows an extra axial mass of the right frontal convexity in heterogeneous signal T2 (red arrow) with subcortical oedema (blue star) in Axial T2 and Flair (a, b). Without restriction on diffusion. In SWI (c) shows a leptomeningeal hemosiderosis, homogeneously enhanced in T1 contrast enhanced (d). This mass infiltrates the cortical sulci, with enhancement of the pachymeninges and leptomeninges (e, f).
Leptomeninges
The key sequence is contrast-weighted T1, shows focal or general leptomeningeal enhancement, node or smooth, about the basal aspects of the brain and the polygon of Willis ; sometimes it goes along the spaces of the Wirshow Robbin, as it may mimic parenchymal lesions.
Parenchyma
Parenchymal involvement is the most common and diverse, appearing as intraparenchymal masses or nodules, periventricular white matter involvement, or extension of leptomeningeal lesions through perivascular spaces.
Hypothalamic and Pituitary
Frequently associated with more extensive leptomeningeal involvement, as it can be isolated, it is observed in some cases only in the infundibulum.
Cranial Nerve
All cranial nerves can be affected, either in isolation or as part of a diffuse leptomeningeal injury. The two nerves that are most sought after are the facial nerve, which is often symptomatic, and the optic nerve [3].
The most important differential diagnoses of neurosarcoidosis are meningioma, dural metastasis, idiopathic hypertrophic cranial pachymeningitis, tuberculous, metastasis, lymphoma, multiple sclerosis, ADEM, primary brain tumors. Treatment based on corticosteroids is recommended as first-line therapy in patients with neurosarcoidosis, although immunosuppressive drugs are usually added due to the chronic course of this condition and to limit the side effects of steroids. With high rate of relapses.
References
- Shah R, Roberson GH, Curé JK (2009) Correlation of MR imaging findings and clinical manifestations in neurosarcoidosis. AJNR Am J Neuroradiol 30: 953-961. [crossref]
- Smith JK, Matheus MG, Castillo M (2004) Imaging manifestations of neurosarcoidosis. AJR Am J Roentgenol 182: 289-295. [crossref]
- Mahi M, Semlali S, En-Nouali H, Karouache A, Satte A, et al. (2007) Imagerie de la neurosarcoïdose. Feuillets de Radiologie 47: 357-362.