Abstract
Background: National Heart Institute (NHI), Cairo – Egypt is a tertiary care center serving cardiovascular patients nationwide. In this study, patients admitted to our institute’s cardiac care unit (CCU) with critical acute cardiovascular conditions (ACVC) were included to assess the management strategies and the in-hospital outcome.
Aim: Determine different presenting diagnoses admitted to NHI-CCU with documentation of their primary management strategies and its correlated outcomes.
Methodology: A prospective cohort study of all comers to NHI-CCU for one month duration from 15/7/2020 to 15/8/2020.
Results: This study represents a cohort of all comers admitted to our institute with ACVC during the study period. Total of 445 patients were included. In terms of gender, 301 patients were males (67.8%) and 143 patients were females (32.2%). The mean age of patients in this cohort was 55.8 ± 13.0 years of age. Patients spent a total length of hospital stay of 2250 days, with an average hospital stay per patient of 6 ± 6 days. The overall mortality was 13% (i.e.: 58 patients). Of particular notice patients presenting with cardiogenic shock or pulmonary edema complicating acute coronary syndrome (ACS) had longer hospital stay and higher mortality.
Conclusion: The current strategy for managing ACS or HF at NHI had markedly improved with a high success rate and favorable overall outcome across different age groups. The presence of acute pulmonary edema or Cardiogenic shock on admission to CCU in patients with ACS (STEMI or NSTE-ACS) is strongly correlated with prolonged hospital stay and in-hospital mortality. Reperfusion strategies, either Primary PCI (PPCI) or pharmaco-invasive approach, has a positive impact on short-term outcome and length of hospital stay. This positive impact is blunted in patients complicated with acute pulmonary edema or cardiogenic shock. Device therapy in patients with decompensated HF impacts short-term outcomes and correlates with a shorter hospital stay.
Introduction
ACVCs are a worldwide health issue that affects both industrialized and underdeveloped countries [1]. This is related to increased mortality; more extended hospital stays, and increased healthcare expenditures. The purpose of this study is to evaluate the treatment strategy, and in-hospital outcomes of patients admitted to NHI with ACVC over a one-month duration.
Objectives
Improve the care of ACVC in NHI and provide optimized management plans.
Aim
Determine different presenting diagnoses admitted to NHI-CCU with documentation of their primary management strategies and their correlated outcomes.
Methodology
Study Design
A prospective cohort study.
Study Setting
Cardiac Care Unit – National Heart Institute
Study Period
One month – Mid-July to Mid-August 2021
Study Population
Inclusion Criteria:
- All comers with ACVC requiring admission to CCU for at least 24 hours
Exclusion Criteria:
- Incomplete or missing diagnosis or outcome.
Study Procedures
All consecutive patients with ACVC admitted to the CCU at the NHI from mid-July to mid-August 2021 were included in this study. Patients’ data were collected, including personal information, clinical history, diagnoses, plan of management, and status at discharge. Further stratification for each group of patients with a specific diagnosis was done according to the management plan. According to the diagnosis and management plan, patients’ status at discharge was recorded.
Data Collection
Patients’ data were collected using a pre-designed electronic worksheet. Once a patient’s data is submitted, it is backed up to an online database. A double-check was performed before patient discharge to ensure no data was missing. In addition, senior staff continuously monitored, assessed, and revised the data collection process to ensure data integrity and completeness.
Ethical Aspects
Informed written consent was signed by all patients who accepted enrollment in this study. In critically ill patients and patients who died before signing a consent, a next of kin signed in substitute.
Statistical Analysis
The Statistical Package for Social Sciences, version 26.0 – 2018 (SPSS Inc., Chicago, Illinois, USA), was used for statistical assessment. Demographic data, clinical diagnoses, plan of management, and hospital outcome were compared using Chi-squared (χ2) test for categorical variables and the unpaired t-test for continuous variables. Relationships between management plans and hospital outcomes were assessed using logistic regression analysis. Quantitative data were expressed as mean ± SD. Qualitative data were expressed as frequency and percentage, and a P value less than 0.05 was considered significant.
Results
During the study period of 1 month from mid-July to mid-August 2021, a total of 445 patients were admitted to the CCU. Primary diagnoses were ACS, CHF, Pulmonary embolism, aortic dissection, Infective endocarditis, and CHB. Regarding gender, 302 patients were males (67.8%), and 143 patients were females (32.2%). Accordingly, the male-to-female ratio is 2.06:1.
Mortality in this cohort was 13% (i.e., 58 patients). The highest mortality was recorded in patients with aortic dissection; that is 100%.
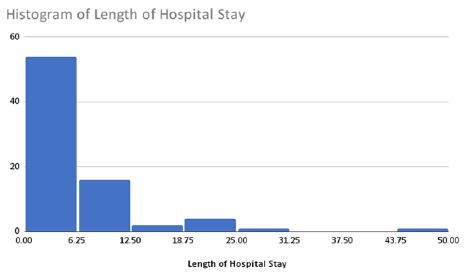
Patients spent a total of 2250 days, with the mean length of hospital stay per patient being six ± six days. The maximum hospital stay was 46 days. The minimum hospital stay was one day.
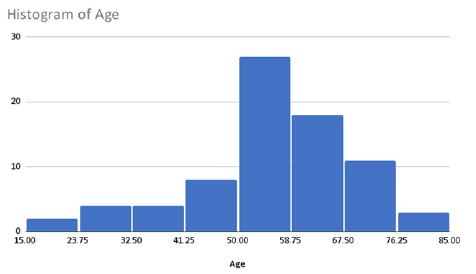
The mean age of patients in this cohort was 55.8 ± 13.0 years of age. The youngest patient was 16-year-old, while the oldest patient was 82-year-old (i.e., Range: 16-82)
|
Primary Diagnosis |
Total no. = 445 |
|
| ACS |
202 |
45.39% |
| High degree AV block |
133 |
29.89% |
| CHF |
78 |
17.53% |
| Ventricular Tachycardia |
11 |
2.47% |
| Pulmonary Embolism |
8 |
1.80% |
| Atrial Fibrillation |
5 |
1.12% |
| Aortic Dissection |
3 |
0.67% |
| Infective Endocarditis |
2 |
0.45% |
| Device related infection |
1 |
0.22% |
| Left Atrial Myxoma |
1 |
0.22% |
Acute Coronary Syndromes
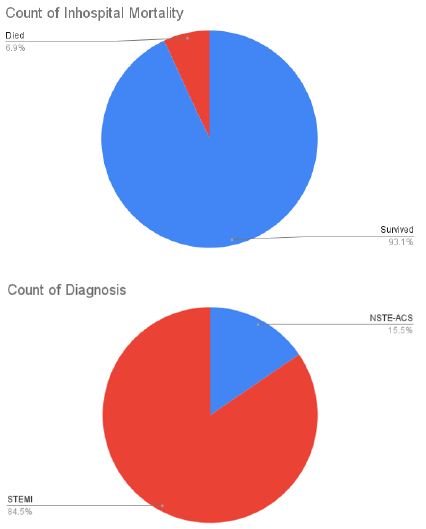
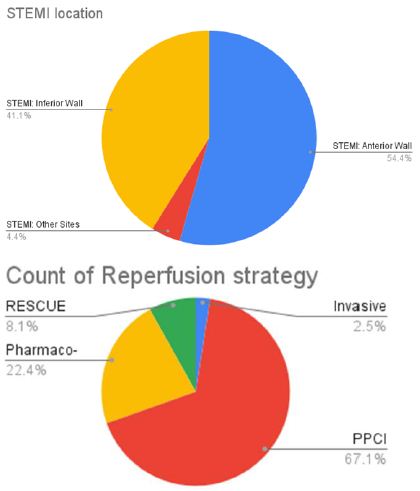
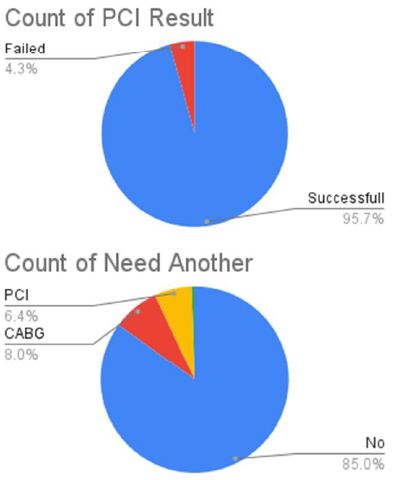
During the study period, a total of 202 cases of ACS were admitted to CCU. The In-hospital mortality was 6.9%. Most of the cases were STEMI (84.5%) vs. 15.5% NSTE-ACS. 95% of the patients had undergone invasive coronary angiography their admission. The initial strategy for STEMI was PPCI in 67%, while the pharmaco-invasive plan was 22.4%. Rescue PCI needed in 8.1%. Delayed PCI was carried out in 2.5%. The success rate for PCI is 96%—failed PCI in 7 patients (4 planned for CABG, two intended for a second attempt).
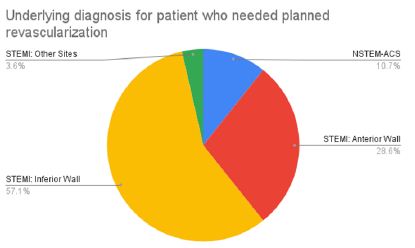
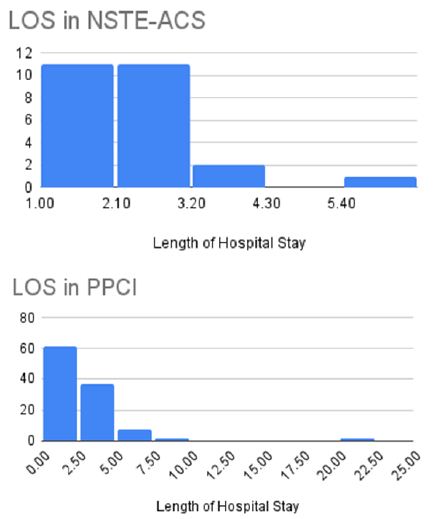
Further revascularization was needed in 14% of cases (8% required CABG, 6% staged PCI). Only 10% of patients who needed further revascularization were initially diagnosed with NSTE-ACS, 90% were STEMI (most commonly inferior STEMI). Thrombolytic therapy was used in 22.4% of STEMI cases. Only SK was used and successful in 69% of cases. All patients with failed SK went for Rescue PCI. Length of hospital stay in PPCI was 2.9 days while was 4.5 days inpatient who received thrombolytic therapy. And was 2.5 days for NSTE-ACS patients. The initial management strategy was significantly correlated with length of hospital stay in STEMI cases (P=0.0002), and the use of thrombolysis was significantly related to a more extended hospital stay P<0.0212.

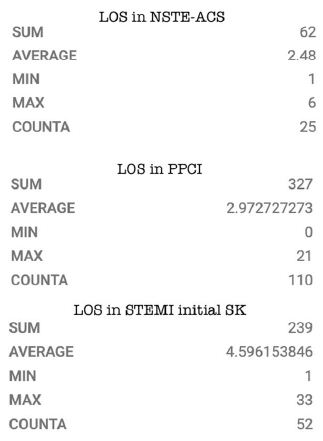
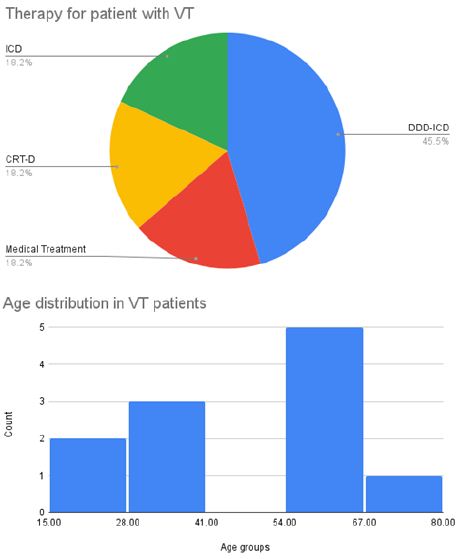
Presenting Diagnosis as AHF among ACS Patients
Patients admitted with cardiogenic shock and pulmonary edema due to an underlying acute coronary syndrome represents a small fraction of ACS patients admitted to NHI. Fifteen cases showed signs of severe AHF during their initial presentation, either APE or Cardiogenic shock. Analysis of ACS complicated by severe AHF showed that Conservative treatment was the most common therapy for those patients. PCI has done in 33%. CABG is 13.3%. Only one case documented a mechanical complication of STEMI (VSR; percutaneous closure was attempted, and the patient died after the procedure. The mortality was 76% in all cases, 80% for PCI, and 75% for the conservatively treated group and 50% for CABG patients.
The use of hemodynamic support was considered in 2 cases; both had IABP insertion (one during PCI the other during CABG).

In regression analysis, the presence of severe AHF (APE or Cardiogenic shock) was the only variable that showed a strong correlation with in-hospital mortality Acute decompensated Heart Failure (AHF).
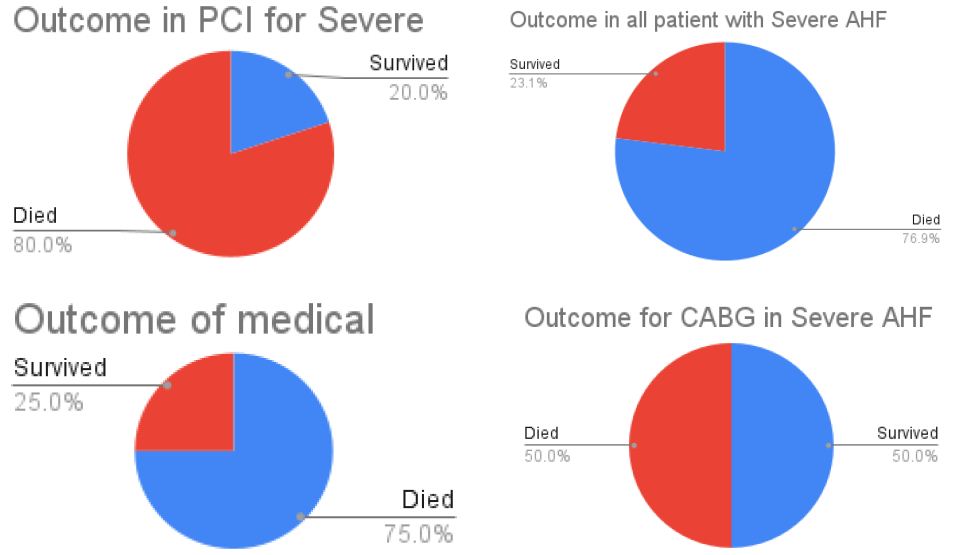
A total of 78 cases were admitted with AHF. 66.7% were males. Various age groups were noticed; the most common decade was 50-60 years, followed by 60-70 years. More than half of the patients’ overall hospital stay was six days. The initial medical strategy was considered in all patients and was directed only toward guidelines-directed medical therapy, and device therapy was considered in the eligible patient. Precipitating factor for decompensation was not documented in admission notes.
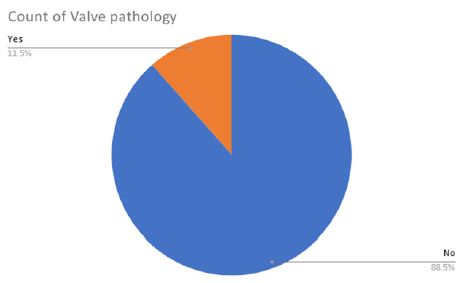
50% of the patients have underlying IHD. 50% (39 cases) are NICM the underlying etiology in patients with NICM was identified in 8 cases (20.5%); 3 cases have primary valve disease as underlying etiology (2 cases with rheumatic MS and one case with severe AS and MR), one case with PPCM, two patients with HFpEF and two patients with isolated right-sided HF. The rhythm was AFib in 24.4% of cases. Moderate to severe secondary valve pathology was documented in 8 patients with AHF; 10.2%. The most common valve pathology was Functional Mitral regurge (5 cases), MR and TR (3 cases), and isolated TR (one patient). Rhythm and valve lesions were not correlated with in-hospital outcomes.
Device therapy in HF correlated with a shorter hospital stay (P=0.0045). Devices used were CRT, CRT-D, and ICD.
IHD in a patient with HF is associated with a prolonged hospital stay. AF, valve pathology is not associated with outcome or stay
Non-Ischemic Cardiomyopathy
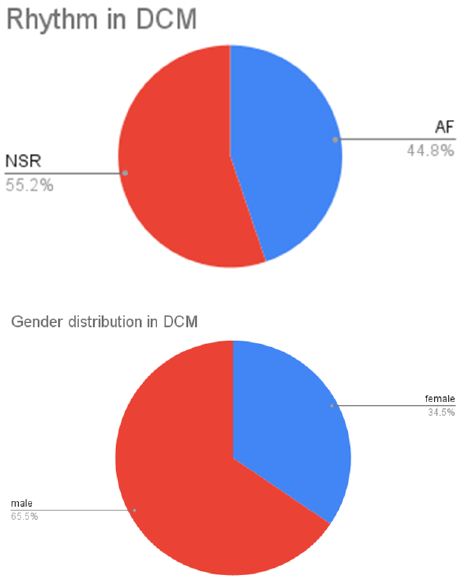
58 cases admitted with decompensated HF without underlying IHD. 65.5% were males. AF was the rhythm in 44.8%. All patients were managed medically. Mortality was in 3 patients; 1 because of VF and two because of progressive pump failure and multisystem affection. The underlying etiology was not identified in 90% of the cases. The diagnosis of HFpEF was documented only in 2 cases out of 78% with CHF, which indicates a significant challenge in identifying this specific subgroup and possibly missing proper diagnostic criteria for this group of patients. In patients with the underlying etiology of primary valve disease for CHF, the rheumatic pathophysiology is more common than degenerative, reflecting the current challenge in developing countries where RHD is still the most common pathology for VHD.
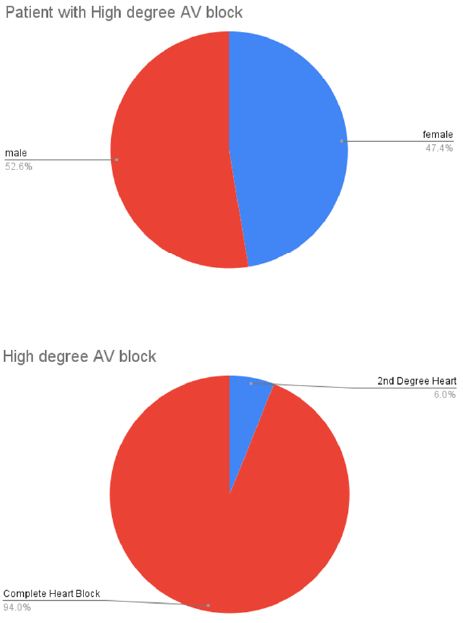
Heart Block
During the study period, 133 patients were admitted to CCU with a high degree A-V block. Eight cases with the second degree and 94% with CHB. 52.4% were males, and 47.6% were females. The average age was 61 years; the range was 1-90 years. The average hospital stay was 7.2 days. 131 patients received a PPM. One patient was managed with medical therapy, and one patient died before pacemaker insertion. A dual-chamber pacemaker was used in 53.4% of cases, while a single lead pacemaker was used in 46.6%. In addition, two patients required CRT while eight patients required ICD according to the associated condition.
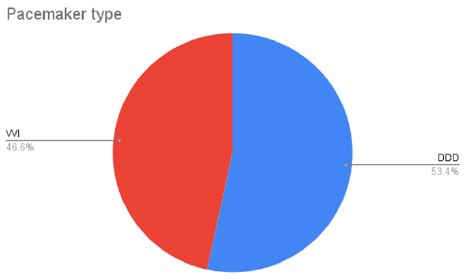
Pulmonary Embolism
Eight cases were admitted with pulmonary embolism. Thrombolytic therapy was the strategy in 62.5% of cases. Medical therapy (anticoagulation) was used in 37.5%. No mechanical therapy was used. Mortality in one patient.
Acute Aortic Dissection
Three patients were admitted with acute aortic dissection; all were Stanford Type A. All were planned for surgical repair. In-hospital mortality 100%. 2 of them died before surgery.
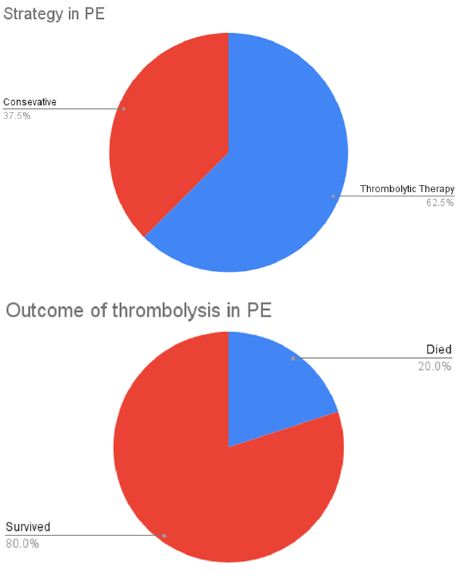
Arrhythmia
Eleven patients were admitted with VT. The most common presenting symptom is syncope. Ten were males, and one was female. The average age was 46 years (range from 19-70 years). Device-based therapy was the default strategy for management in 9 patients. Devices used were DDD-ICD (5 cases), ICD (2 cases), and CRT-D (2 cases). Medical therapy was the strategy in 2 cases. Mortality was 1 case.
Atrial Fibrillation (AF)
AF was the primary diagnosis in 5 cases. 4 were males. Rate control is used in one patient. Electrical cardioversion was used in one patient. Three cases underwent ablation for AF. Mortality in one point, which was in the ablation group.
As a secondary diagnosis, AF was ubiquitous in all cases admitted with CHF. Found in 44.8% of all patients with DCM and 11% of cases with ICM. All patients were managed medically.
SVT
One case was admitted with resistant SVT and underwent ablation successfully.
Cardiovascular Related Infections
Three cases were admitted with infections. 2 had IE; one was native tricuspid, and one was prosthetic valve endocarditis. Both were treated medically. One was device-related (Pacemaker) and required device replacement.
Others
One case was admitted with left atrial myxoma and went surgery.
Discussion
Our management strategies and outcomes were compared to the internationally available observational data for each subgroup of cases.
ACS
In patients with ACS, the invasive approach was the default method for most patients admitted to NHI. PPCI was the standard treatment for all STEMI patients. However, the pharmaco-invasive plan was an acceptable option in circumstances where ideally timed reperfusion was not achievable. PPCI has a success rate of 96%, which satisfies international standards [2,3]. Thrombolysis was successful in 69% of patients; however, the only thrombolytic agent utilized was SK, the only agent available, and no adverse effects were reported. Newer agents, such as t-PA and TNK, would produce a better result.
In patients with NSTE-ACS, the invasive technique was used in all scenarios; this could be related to the higher risk category of NSTE-ACS referred to NHI, where Invasive strategy should be the standard regimen.
In ACS patients presented by AHF, the consideration of an invasive strategy was considerably lower. The most frequent method was to use medical treatment. This finding could be related to the interventionist perception of the procedural risk or futility of any intervention. In some instances, advanced shock and multisystem affection were the primary causes of this significant caring trend change. The survival in those subgroups of patients who underwent invasive treatment was 20% [4,5], while the survival for conservative strategy was 25%. CABG was considered in few cases; however, the number is too small to make a clear conclusion. It should be noted that IABP was the only hemodynamic support available to those individuals because advanced MCS (Impella® and LVAD) were not available.
Acute Decompensated Heart Failure
As regards decompensated HF, admission criteria were based only on clinical evaluation and radiological findings. As per study protocol, AHF complicating ACS was included in the ACS subgroup but not in the AHF group. The average hospital stay was similar to the international data [6].
Device therapy, including CRT, CRT-D, and ICD, was associated with a shortened hospital stay. However, we cannot make a causal relation between an acute benefit of device therapy and short-term outcomes in those patients.
Pulmonary Embolism
For a patient with PE, more than half the patients received thrombolytic therapy. The decision of thrombolysis was physician dependent and non-standardized. Initial hemodynamic data was missing. SK was the only thrombolytic agent used, as a newer agent was not available. Mechanical thrombectomy was not used in any patient, as mentioned above.
Aortic Dissection
In our snapshot cohort, only 3 cases were admitted over a month duration. All patients were of Stanford type A, and all of them planned for surgical repair. Mortality was 100%. Time to surgery was missed. The small number of cases and the available data limits our capability to provide a clear conclusion. However, it is urgently needed to collect more data over an extended time to verify patient outcomes.
Atrial Fibrillation
A common condition exists either as a primary or secondary diagnosis, especially in patients with CHF, either DCM or IHD. The consideration of ablation in AF is an outstanding achievement. However, it was noticed that conservative medical therapy was the default strategy for all patients with CHF and AF. The consideration of device therapy targeting LV dysfunction was much less when AF was associated. Moreover, concern for rhythm control or ablation for AF was underutilized with CHF.
Heart Block
Our Success rate in device therapy is meeting the international standards [7,8]. A dual-chamber in almost half of the patients is an excellent achievement in a big volume center with limited resources. Thirty patients stayed in hospital more than eight days, up to 88 days, with an average of 22 days. There is no clear explanation for the underlying reason for their prolonged hospital stay and whether the delay was because of delayed intervention or procedure-related. A follow-up registry is needed to evaluate long-term outcomes and reflect our practice on functional class and quality of life [9].
Conclusion and Recommendations
- Although it is a single-center experience, NHI is a high-volume cardiac center with a CCU admission rate of around 400 patients per month.
- NHI has established a successful 24/7 PCI service with a high success rate. Accordingly, invasive reperfusion methods, whether PPCI or pharmaco-invasive, have a beneficial influence on short-term results and hospital stay length.
- The present method for addressing ACS or HF at NHI has significantly improved, with a positive overall result across all age categories.
- Strategies that result in a shorter hospital stay and reduced readmissions should be seriously explored in such a high-volume institution.
- Accurate monitoring of timed reperfusion goals for various ACS reperfusion methods is urgently required to tackle all time delay components.
- Complicated ACS patients with AHF have a very high risk of poor outcomes and are significantly associated with more extended hospital stays and in-hospital deaths. In this group of patients, invasive strategies -in our local experience-provided a muted benefit, indicating the need for further development in treatment measures. Well-established methods like ventricular unloading devices or MCS should be considered urgently to support successful mechanical reperfusion and improve prognosis.
- Available Device therapy (CRT, DRT-D, and ICD) in patients with decompensated HF impacts short-term outcomes and correlates with a shorter hospital stay. Follow-up data reflecting the impact on long-term effects is needed.
- Poor outcomes noticed in specific diagnoses like cardiogenic shock and Aortic dissection mandate the generation of an institute-specific registry for more precise data collection over a more extended period to guide further management optimization.
- Creating an electronic health record for mega data collections will offer a clearer picture of healthcare quality rather than analysis of snapshot data. As a result, more comprehensive recommendations regarding areas for improvement will be implemented.
References
- Savarese G, Lund LH (2017) Global Public Health Burden of Heart Failure. Cardiac Failure Review 3: 7-11. [crossref]
- Shehab A, Al-Dabbagh B, Almahmeed W, et al. (2012) Characteristics and in-hospital outcomes of patients with acute coronary syndromes and heart failure in the United Arab Emirates. BMC Res Notes 5: 534. [crossref]
- Peter J McCartney, Colin Berry (2019) Redefining successful primary PCI. European Heart Journal – Cardiovascular Imaging 20: 133-135. [crossref]
- Nieminen MS, Harjola VP (2005) Definition and epidemiology of acute heart failure syndromes. Am J Cardiol 96: 5G-10G. [crossref]
- Cannon CP, Battler A, Brindis RG, Harrington RA, Krumholz HM, et al. (2001) American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee). J Am Coll Cardiol 38: 2114-2130. [crossref]
- Cowie MR, Anker SD, Cleland JGF, Felker GM, Filippatos G, Jaarsma T, et al. (2014) Improving care for patients with acute heart failure: before, during and after hospitalization. ESC Heart Fail 1: 110-45. [crossref]
- Armstrong PW, Pieske B, Anstrom KJ, Ezekowitz J, Hernandez AF, et al. (2020) Vericiguat in Patients with Heart Failure and Reduced Ejection Fraction. The New England Journal of Medicine 382: 1883-1893. [crossref]
- Lee TC, Kon Z, Cheema FH, et al. (2018) Contemporary management and outcomes of acute type A aortic dissection: an analysis of the STS adult cardiac surgery database. J Card Surg 33: 7-18. [crossref]
- Rajaeefard A, Ghorbani M, Babaee Baigi MA, Tabatabae H (2015) Ten-year Survival and Its Associated Factors in the Patients Undergoing Pacemaker Implantation in Hospitals Affiliated to Shiraz University of Medical Sciences During 2002 – 2012. Iranian Red Crescent Medical Journal 17: e20744. [crossref]