Abstract
Background: Carpal tunnel syndrome is considered the most common nerve compression disorder of the arm and an important cause of pain, neurologic symptoms and functional limitation of the wrist and hand. Carpal tunnel syndrome is a complex disorder associated with localized compression of the median nerve at the carpal tunnel.
Aim and objectives: To assess the functional outcome of Mini open carpal tunnel release.
Patients and methods: The present study was conducted on 25 patients in Post graduate Department of Orthopaedics, Govt. Hospital for Bone and Joint Surgery, an associated hospital of Govt. Medical College Srinagar from July 2019 to August 2021.
Results: The average symptom severity score improved from 3.5 preoperatively to 1.3 at final follow up of 6 months. The average functional status score improved from 3.3 preoperatively to 1.42 at the final follow up of 6 months. The mean DML and mean DSL decreased from 5.9 mS and 5.2 mS pre operatively to 4.7 mS and 3.9 mS respectively at the final follow up of 6 months. The mean sensory conduction velocity at 6 months post-operative was 39.6 m/s with range from 22.6 to 60.9 m/s. The mean sensory conduction velocity increased from 28.4 m/s pre operatively to 39.6 m/s at the final follow up of 6 months. 2 patients (8%) in our study experienced persistent symptoms 1 patient (4%) had superficial infection which settled with oral antibiotics.
Conclusion: Mini open carpal tunnel release is an effective procedure which gives excellent symptomatic and functional outcome with very few complications. The mini open technique gives an additional advantage of less operative time, less wound related complications, improved cosmesis and quicker return to routine activity as compared to the open release.
Keywords
Carpal tunnel syndrome, Mini-open, Median nerve, Transverse carpal ligament
Introduction
Carpal Tunnel Syndrome (CTS) is a fairly common peripheral neuropathy, caused by median nerve compression at the wrist level. The prevalence of CTS is believed to be 3.8% of general population around the world. The syndrome is more common in females than in males, with a peak age range of 40-60 years. On the basis of clinical examinations and nerve conduction studies, it had been approximated that one ·in every 5 subjects who complain of symptoms such as pain, numbness and a tingling sensation in hands could have CTS.
In recent years there has been an increase in incidence of CTS, may be due to the awareness of people about this disease, the upward disease detection rate, the work is more and more meticulous and delicate requiring using wrist continuously [1-7]. The etiology of CTS is largely structural, genetic and biological, with environmental and occupational factors. 70% of CTS cases are of unknown causes, the others are due to intrinsic and extrinsic factors. Intrinsic factors which exert pressure within the tunnel are pregnancy, hemodialysis, gout, diabetes, Rheumatoid arthritis, various other inflammatory and connective tissue disorders and systemic diseases like hypothyroidism, etc. Extrinsic factors which exert pressure outside the tunnel are lipomas, ganglion and vascular formations. Patients with CTS present with a constellation of symptoms including numbness and tingling of hand in the distribution of median nerve, nocturnal paresthesias as well as weakness and atrophy of the thenar muscles [8-11].
CTS may be managed conservatively at first with local corticosteroid injections, splints, and other techniques. However, in recent practice, treatment is selected considering various factors such as the stage of disease, the severity of symptoms or the patient preference. Splinting, local steroid injections and oral steroids have proven effective in some cases. The rationale for wrist splint is based on observations that CTS symptoms improve with rest and aggravate with activity. Subsequent research has suggested that the therapeutic effect of wrist splinting arises from minimizing carpal tunnel pressures. Corticosteroid treatment is effective in reducing inflammation and edema of synovium and tendons. It also has harmful effect on tenocyte function by reducing collagen and proteoglycan synthesis. However non operative modalities are preferred in the early stages of the disease. Advanced stages with persistent clinical features need a surgical release from the compression. Surgery offers an effective way of treating the condition. The basic principle of CTS surgery is to increase the volume of the carpal tunnel by releasing the transverse carpal ligament (TCL) thereby releasing pressure on the median nerve. A wide variety of surgical techniques have been described for CTS. However, as of yet, no strong evidence has suggested that any one approach is superior to the others [12-17].
Mini incision release is a less invasive technique with lower rate of complications, shorter operative time and more cost effectiveness. Although each technique has advantages and disadvantages, a few studies reported that mini incision release technique decreases the pathologic swelling of the median nerve and scar formation at the inlet of the carpal tunnel [18,19]. Thus in this study we aim to evaluate the safety, effectiveness and recurrence rate of mini-open carpal tunnel release technique.
Patients and Methods
This was a prospective study that was conducted from July 2019 to July 2021 which included 25 consenting patients who presented to the Post graduate Department of Orthopaedics, Govt. Hospital for Bone and Joint Surgery, an associated hospital of Govt. Medical College Srinagar and diagnosed as having carpal tunnel syndrome following approval by institutional ethical committee.
Inclusion Criteria
- Signs, symptoms and electro-diagnostic tests characteristic of carpal tunnel syndrome
- No response to conservative treatment for at least 6months
- Age >18 years
- All sexes
Exclusion criteria
- Peripheral Neuropathy
- Prior Carpal Tunnel release
- Inflammatory arthropathy
- Deformity of hand/wrist
- Prior trauma (<2weeks)
- Pregnancy
- Operation for excision of neoplasm
Surgical Technique
Prophylactic Antibiotic (IV Cefuroxime 1.5 gm) was given half an hour before surgery. The surgical intervention was performed under regional Anaesthesia (Axillary / Supra clavicular block) using a tourniquet. The patient placed in the supine position with the hand, wrist and fingers stretched in slight extension position, a small support placed under the wrist. A 1.5-2 cm longitudinal incision, located on the vertical line drawn from the third inter digital space and extending proximally to the distal wrist crease, was performed. The skin subcutaneous tissue dissected, the proximal end of the transverse carpal ligament visualized, and the dorsal and ventral surfaces of the ligament were dissected. Using scissors, the transverse carpal ligament was cut in the proximal to distal direction. After achieving hemostasis, the surgical field was irrigated with a physiological saline solution and the skin closed with silk. The patients’ hands and palms dressed with ample cotton padding and elevated (Figure 1).
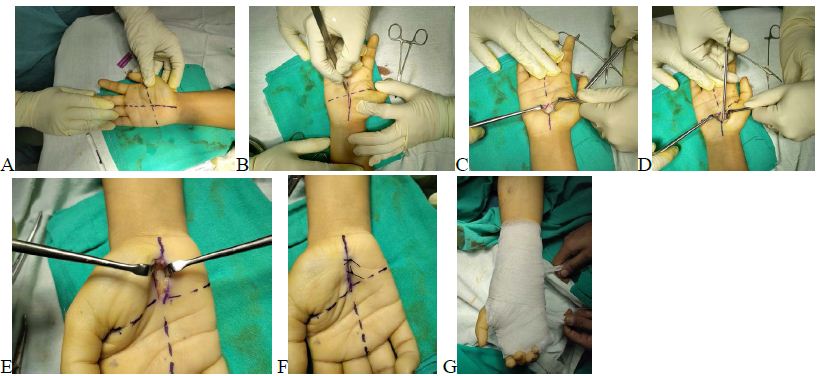
Figure 1: Intra-operative pictures.
(A) On Table Skin Marking for Incision (B) Skin Incision(C) Superficial Dissection (D) Cutting of Transverse Carpal Ligament (E) Exposure of Median Nerve (F) Skin Closure (G) Bulky Antiseptic dressing.
Post-operative Rehabilitation and Follow-up
Single dose of IV antibiotic was given Post Operatively followed by oral Antibiotics for 5 days. Finger ROM exercises were started immediately after surgery. Dressing was changed to a lighter one at 3 to 4 days to start wrist motion. Patients were allowed to return daily normal activities at 3 to 4 weeks post operatively. Patients were followed up at 3 and 6 months post operatively and NCV was repeated at 6 months post operatively. Outcome was assessed by Boston Carpal Tunnel Questionnaire-1993 (Tables 1 and 2).
Table 1: Symptom severity scale according to BOSTON CARPAL TUNNEL
| 1 | 2 | 3 | 4 | 5 | |
| 1. How severe is the hand or wrist pain that you have at knight? | Normal | Slight | Medium | Severe | Very serious |
| 2. How often did hand or wrist pain wake you up during a typical knight in the past two weeks? | Normal | Once | 2-3 times | 4-5 times | More than 5 times |
| 3. Do you typically have pain in your hand or wrist during the daytime? | No pain | Slight | Medium | Severe | Very serious |
| 4. How often do you have hand or wrist pain during the daytime? | Normal | 1-2 times/day | 3-5 times/day | More than 5 times | Continued |
| 5. How long on average does an episode of pain last during the daytime? | Normal | <10 minutes | 10-60 continued | >60 minutes | Continued |
| 6. Do you have numbness (loss of sensation) in your hand? | Normal | Slight | Medium | Severe | Very serious |
| 7. Do you have weakness in your hand or wrist? | Normal | Slight | Medium | Severe | Very serious |
| 8. Do you have tingling sensation in your hand? | Normal | Slight | Medium | Severe | Very serious |
| 9. How severe is numbness (loss of sensation) or tingling at knight? | Normal | Slight | Medium | Severe | Very serious |
| 10. How often did hand numbness or tingling wake you up during a typical knight from last two weeks? | Normal | Once | 2-3 times | 4-5 times | More than 5 times |
| 11. Do you have difficulty with the grasping and use of small objects such as keys or pens? | Without difficulty | Little difficulty | Moderate difficulty | Very difficulty | Very difficulty |
Table 2: Function status scale according to BOSTON CARPAL TUNNEL
| No difficulty | Little difficulty | Moderate difficulty | Intense difficulty | Cannot perform the activity due to hand and wrist symptoms | |
| Writing | 1 | 2 | 3 | 4 | 5 |
| Buttoning in cloths | 1 | 2 | 3 | 4 | 5 |
| Holding a book while reading | 1 | 2 | 3 | 4 | 5 |
| Gripping of a telephone handle | 1 | 2 | 3 | 4 | 5 |
| Opening of jars | 1 | 2 | 3 | 4 | 5 |
| Household chores | 1 | 2 | 3 | 4 | 5 |
| Carrying of grocery basket | 1 | 2 | 3 | 4 | 5 |
| Bathing and dressing | 1 | 2 | 3 | 4 | 5 |
Results
In our study, the mean age of patients was 50.4 (range 35-60) years. The mean duration of surgery was 10.8 (range 8-15) minutes. Demographic and baseline clinical data for the patient cohort are shown in Table 3. In our study, the average symptom severity score at 3 and 6 months post-operative was 1.8 (range 1.45 to 3.18) and 1.58 (range 1.27 to 2.9) respectively. The average symptom severity score improved from 3.5 preoperatively to 1.3 at final follow up of 6 months. The average functional status score at 3 and 6 months postoperative was 1.68 (range 1.33 to 3) and 1.42 (range 1.6 to 2.5). The average functional status score improved from 3.3 preoperatively to 1.42 at the final follow up of 6 months (Table 4). The mean DML and DSL at 6 months post-operative was 4.6 mS (range 3.3 to 6.2 Ms) and 3.9 mS (range 3.1 to 6.5 mS) respectively. The mean DML and mean DSL decreased from 5.9 mS and 5.2 mS pre operatively to 4.7 mS and 3.9 mS respectively at the final follow up of 6 months. The mean sensory conduction velocity at 6 months post-operative was 39.6 m/s with range from 22.6 to 60.9 m/s. The mean sensory conduction velocity increased from 28.4 m/s pre operatively to 39.6 m/s at the final follow up of 6 months (Table 5). 2 patients (8%) in our study experienced persistent symptoms 1 patient (4%) had superficial infection which settled with oral antibiotics (Table 6). Overall, most of the patients achieved satisfactory results.
Table 3: Descriptive Statistics of the Study Population (N=25)
| Variables | No. of patients | Percentage | |
| Sex | Male | 2 | 8 |
| Female | 23 | 92 | |
| Age group | <34 years | 0 | 0 |
| 34-45 years | 5 | 20 | |
| 46-55 years | 15 | 60 | |
| >55 years | 5 | 20 | |
| Side | Right | 13 | 52 |
| Left | 7 | 28 | |
| Bilateral | 5 | 20 | |
| Pre-operative symptom duration | <6 months | 0 | 0 |
| 6-12 months | 11 | 44 | |
| 13-24 months | 11 | 44 | |
| 25-36 months | 3 | 12 | |
Table 4: Symptom severity score and function status scale according to BOSTON CARPAL TUNNEL
|
|
Average score | Pre-operative | 3 months post-operative | 6 months post-operative | |||
| No. of patients | Percentage | No. of patients | Percentage | No. of patients | Percentage | ||
| Symptom severity score | 1-2 | 0 | 0 | 21 | 84 | 23 | 92 |
| 2.01-3 | 0 | 0 | 3 | 12 | 2 | 8 | |
| 3.01-4 | 23 | 92 | 1 | 4 | 0 | 0 | |
| 4.01-5 | 2 | 8 | 0 | 0 | 0 | 0 | |
| Mean | 3.5 (range3.09-4.09) | 1.8 (range 1.45-3.18) | 1.58 (range 1.27-2.9) | ||||
| Functional status score | 1-2 | 0 | 0 | 24 | 96 | 24 | 96 |
| 2.01-3 | 11 | 44 | 1 | 4 | 1 | 4 | |
| 3.01-4 | 14 | 56 | 0 | 0 | 0 | 0 | |
| 4.01-5 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Mean | 3.15 (range 2.66-4) | 1.68 (range1.33-3) | 1.42 (1.16-2.25) | ||||
Table 5: Distal motor latency, Distal sensory latency and Sensory conduction velocity Pre-operatively and 6 months post-operative
| Average score | Pre-operative | 6 months post-operative | |||
| No. of patients | Percentage | No. of patients | Percentage | ||
| Distal motor latency (mS) | <4 | 0 | 0 | 7 | 28 |
| 4-6 | 16 | 64 | 16 | 64 | |
| 6.01-8 | 7 | 28 | 2 | 8 | |
| >8 | 2 | 8 | 0 | 0 | |
| Mean | 5.6 (range 4.2-8.1) | 4.6 (range 3.3-6.2) | |||
| Distal sensory latency (mS) | <4 | 4 | 16 | 13 | 52 |
| 4-6 | 16 | 64 | 11 | 44 | |
| 6.01-8 | 3 | 12 | 1 | 4 | |
| >8 | 2 | 8 | 0 | 0 | |
| Mean | 5.2 (range 3.45-8.5) | 3.9 (range 3.1-6.5) | |||
| Sensory conduction velocity (m/s) | <20 | 6 | 24 | 0 | 0 |
| 20-30 | 9 | 36 | 1 | 4 | |
| 30.01-40 | 6 | 24 | 15 | 60 | |
| >40 | 4 | 16 | 9 | 36 | |
| Mean | 28.4 (range 12.3-44) | 39.6 (range 22.6-60.9) | |||
Table 6: Superficial infection which settled with oral antibiotics
| Complications | No. of patients | Percentage |
| Persistent symptoms | 2 | 8 |
| Superficial infection | 1 | 4 |
| Nil | 22 | 88 |
| Total | 25 | 100 |
Discussion
Conventional open carpal tunnel release has been widely accepted as an effective method for treating carpal tunnel syndrome after failed conservative management. This prospective study demonstrated the benefits of mini-open carpal tunnel release under local anesthesia, in terms of clinical recovery and relief of symptoms in the short and long term (3 and 6 months respectively). These improvements were of both statistical significance and clinical relevance. These procedures have shown comparable postoperative pain, earlier recovery and return to work, improved grip strength, and reduced complication rate. These are easier to perform and safer procedures as compared to endoscopic ones and do not require any special equipment. The technique requires limited dissection and little interruption of tissue planes as compared to the open method and doesn’t divide the subcutaneous tissue or the palmar fascia as much as the open method does [20-24].
In this study we found that the mean age of development of carpal tunnel was 50.4 years, which is comparable to Thanh Ma Ngoc et al. (2017) which showed that the mean age was 50.3 years. Hamid Reza Aslani et al. (2012) noted high incidence of carpal tunnel syndrome in females, which is similar to our study. In our study the mean pre-operative symptom duration was 17.4 months with range from 6 to 36 months. In other previously done studies, the mean pre-operative duration ranged from 10.8 to 13.3 months. In our study, the average pre-operative DML was 5.6mS with range from 4.2 to 8.1. In other previously done studies this mean ranged from 5.44 to 7.3 which is comparable to our study. The mean operative time in our study was 10.8 minutes with a range from 8 to 15 minutes which is comparable Keykhosro Mardanpour et al. (2018) who noted in his study the mean operative time was 12 minutes. In our study, the average 3 months post-operative symptom severity score was 1.8 which is comparable with previously done study by Seyho Cem Yucetas et al. (2012) as 1.95. In our study, the average functional severity score at 3 months was 1.68 and the average DML at 6 months post-operative was 4.6mS which is comparable with the results obtained in study done by Heybeli et al. (2002) as 1.5 and 4.7 mS respectively. Majority of patients in our study had no complications. 2 patients experienced persistent symtoms (8%). In other studies inadequate symptom relief ranged from 2% to 3.8%. 1 patient (4%) in our study had has superficial infection. The percentage of infection ranged from 0% to 1.9% in other studies.
One weakness of our study is the group of the patients is small. In addition, the follow up may be too short. However, for a preliminary report, the result is quite encouraging, i.e., the procedure improves the symptom of the patients even in short term follow-up and improve the cosmetic appearance compare to a long incision. We hope to collect more patients and carry out longer follow-up in the future [25-29].
Conclusion
Mini open carpal tunnel release is an effective procedure which gives excellent symptomatic and functional outcome with very few complications. The mini open technique gives an additional advantage of less operative time, less wound related complications, improved cosmesis and quicker return to routine activity as compared to the open release.
References
- Alfonso C , Jann S , Massa R, Torreeggiani A.(2010). Diagnosis , treatment and follow up of the carpal tunnrl syndrome: a review. Neural Sci .31:243-252. [crossref]
- Aroori S, Spence RA.(2008). Carpal tunnel syndrome. Ulster Med 77:6-17
- Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, etal.(1999). Prevalence of carpal tunnel syndrome in a general population. JAMA. 282:153-158. [crossref]
- Phalen GS.(1966). The carpal tunnel syndrome. Senventeen years’ experience in diagnosis and treatment of 654 hand. J Bone Joint Surg Am.48:211-228.
- Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, etal.(1999). Prevalence of carpal tunnel syndrome in a general population. JAMA. 282(2):153-158. [crossref]
- Jenkins PJ, Duckworth AD, Watts AC, McEachan JE (2012). The outcome of carpal tunnel decompression in patients with diabetes mellitus. J Bone Joint Surg 94:811-814. [crossref]
- Palmer AK, Toivonen DA (1999) Complications of endoscopic and open carpal tunnel release. J Hand Surg 24: 561-565. [crossref]
- Lozano-Calderon S, Anthony S, Ring D.(2008). The quality and strength of evidence for etiology: Example of carpal tunnel syndrome. J Hand Surg Am. 33:525-38. [crossref]
- Wong KC, Hung LK, Ho PC, Wong JMW (2003) Carpal tunnel release – A prospective, randomized study of endoscopic versus limited-open methods. J bone Joint Surg. 85-B:863-868. [crossref]
- Kasdan ML (2000) Complications of endoscopic and open carpal tunnel release. J Hand Surg 25:185. [crossref]
- Muller M,TsuiD, Schnur R, HardJ, Biddulph D L,etal.( Effectiveness of hand therapy intervention in primary management of carpi tunnel syndrome: a systemic review. J Hand therapy. 17:210-228.
- Padua L, Coraci D, Erra C, Pazzaglia C, Paolasso I et al.(2016). Carpal tunnel syndrome: clinical features, diagnosis, and management. Lancet Neurol. 15:1273-4. [crossref]
- Piazzini DB, Aprile I, Ferrara PE, et al.(2007). A systematic review of conservative treatment of carpal tunnel syndrome. Clin Rehabil. 21:299-314.[crossref]
- Walker WC, Metzler M, Cifu DX, Swartz Z.(2000). Neutral wrist splinting in carpal tunnel syndrome: a comparison of nightonly versus full-time wear instructions. Arch Phys Med Rehabil. 81:424-429.[crossref]
- Graham B, Peljovich AE, Afra R, et al.(2016). The American academy of orthopaedic surgeons evidence-based clinical practice guideline on: management of carpal tunnel syndrome. J Bone Joint Surg Am.98:1750-4.[crossref]
- Huisstede BM, Randsdorp MS, Coert JH, Glerum S, van-Middelkoop M, etal.(2010). Carpal tunnel syndrome. Part II: effectiveness of surgical treatments-a systematic review. Arch Phys Med Rehabil. 91:1005-1024.[crossref]
- Standring S.(2005). Gray’s Anatomy: The Anatomical Basis of Clinical Practice. New York: Elsevier .p.913.
- lsogai S, Murakami G, Wada T, Akita K, YamashitaT, etal.(2002). Laminar configuration of the transverse carpal ligament. J OrthopSci .7:79-83.[crossref]
- Phalen GS.(1966). The carpal-tunnel syndrome. Seventeen years’ experience in diagnosis and treatment of 654 hands. J Bone Joint Surg. 48:211-28.
- Cellocco P, Rossi C, Bizzarri F, Patrizio L, Costanzo G.(2005). Mini-open blind procedure versus limited open technique for carpal tunnel release: a 30-month followup study. J Hand Surg Am. 30:493-9.[crossref]
- Wong KC, Hung LK, Ho PC, Wong JMW.(2003). Carpal tunnel release. A prospective, randomized study of endoscopic versus limited-open methods. J Bone Joint Surg Br. 85:863-8. .[crossref]
- Lee WP, Strickland JW.(1998). Safe carpal tunnel release via a limited palmar incision. Plast Reconstr Surg.101:418-6.
- Abdel-Moneim H, Said A-B.(2016). Double mini incision in the treatment of carpal tunnel syndrome. Egypt Orthop J.51:90-3.
- Ngoc TM, Dung TT, Huu MN, Le KT, Tran Q, et al. (2017) The Result of Mini-Open Surgery for Carpal Tunnel Syndrome. Ann Musculoskelet Med 1: 046-049.
- R. Aslani et al.(2012). Comparison of carpal tunnel release with three different techniques. Clinical Neurology and Neurosurgery 114: 965-968.[crossref]
- Mardanpour K, Rahbar M, Mardanpour S.(2019). Functional outcomes of 300 carpal tunnel release: 1.5 cm longitudinal mini-incision. AsianJ Neurosurg 2019; 14:693-7. [crossref]
- Seyho Cem Yücetaş1 Adem Yildirim2.(2013). Comparative Results of Standard Open and Mini Open, Knife Light Instrument-Assisted CarpalTunnel Release.J Neurol Surg A Cent Eur Neurosurg. 74:393-9. [crossref]
- Heybeli, Kutluhan S, Demirci S, Kerman M , Mumcu EF.(2002). Assessment of outcome of carpal tunnel syndrome: a comparison of electrophysiological findings and a self-administered boston questionnaire. Journal of Hand Surgery.27B: 3: 259-264.