Abstract
Introduction: Scorpion envenomation is a common occurrence in tropical areas. There are three grades of severity. Cardiovascular complications are the most feared and condition the vital prognosis of the victim.
Observation: We report the case of scorpion envenomation that occurred in a 23-year-old young man with no cardiovascular history in the Kidal region in northern Mali. Three hours after the injection, the patient presented with massive Acute Pulmonary Edema (APO) and a state of cardiogenic shock. In intensive care at the level 2 hospital (HN2), he had received treatment based on oxygen therapy, diuretics and vasoactive amine (Dobutamine). He was then evacuated to HN3 in Dakar (Senegal). The evolution has been favorable.
Conclusion: Scorpion envenomings are serious. Cardiovascular complications condition the vital prognosis of the patient. It is a real medical race against time.
Keywords
Envenomation, Scorpion, Cardiogenic shock, Sahara-Africa
Introduction
Each year, more than one million scorpion stings and more than 3000 deaths are recorded worldwide [1-3]. Scorpion envenomation is common in tropical and sub-tropical areas. Its evolution can be serious and life threatening. Scorpion stings have a mortality rate of 1 to 2%, mainly due to cardio-respiratory failure in the absence of treatment [1-3]. We report the case of a massive acute pulmonary edema (APO) with post-scorpion sting cardiogenic shock, which occurred in a young man in Kidal (extreme north of Mali).
Observation
The victim was a 23-year-old soldier with no particular history, particularly cardiovascular, on a United Nations peacekeeping mission in the Kidal region of Mali. The scorpion sting was unique, sitting at the level of the foot and took place on May 19, 2020 at 7 p.m. It was a yellowish colored scorpion known as Leiurus quinquestriatus. The victim was taken immediately to the level 1 medical structure of his unit, he received an analgesic treatment based on Paracetamol. Three hours later, faced with the worsening of the clinical condition (confusion, agitation and profuse sisters), the victim was referred to the level 2 hospital for better care.
The rapid clinical examination on admission (H0) to intensive care at level 2 hospital (HN2), a field hospital, noted a patient covered in profuse sweating, agitated and confused with a Glasgow score of 13/15. The conjunctivae were well colored, the extremities cold, the peripheral pulses stringy, the arterial pressure (BP) impregnable. The patient was polypneic with a respiratory rate (RR) of 30 breaths per minute, oxygen saturation (SpO2) was 89% on room air. The temperature was 37.2°C. Cardiac auscultation noted tachycardia with a heart rate (HR) of 140 beats/min with a left and right gallop sound. There was no breath or friction. Lung auscultation revealed bilateral crackles reaching three-quarters of both lung fields. Locally at the level of the foot, a circumscribed inflammatory edema is observed. We concluded that there was grade 3 scorpion envenomation complicated by cardiogenic shock with massive APO. In an emergency, the victim monitored under a multi-parameter scope was placed in a semi-sitting position and received oxygen therapy with a high-concentration mask, continuous Dobutamine with an electric syringe pump (PSE), administration of a first dose of antiscorpionic serum (SAS) at the PSE, a slow vascular filling with Gelofusine 500 ml.
At (H0+20 mn), the patient presented coughing efforts with frothy pink sputum and vomiting efforts. The SpO2 was still below 90%, the FR at 30 cycles/min, the HR had increased to 151 beats/min. BP was perceived at 87/70 mmHg. We started doses of Furosemide 20 mg IVD every 10-15 min depending on SBP, administered a second dose of SAS à la (PSE), Omeprazole (40 mg), injectable Metoclopamide and Betamethasone 8 mg in intravenous. There was no extrasystole on the scope.
The electrocardiogram (Figure 1) had objectified a tachycardia at 150 beats/minute. The AP chest X-ray showed hilifuge-like fluffy opacities in “butterfly wings” disseminated in the two pulmonary fields in favor of a massive (APO) (Figure 2). A cardiac ultrasound (Fast Echo) carried out had objectified a left ventricle (LV) at 56 mm, severe global parietal hypokinesia, a restrictive mitral filling flow (E/A at 4), the systolic ejection fraction of the LV estimated at 25%, a TAPSE at 9 mm without PAH (Figure 3).
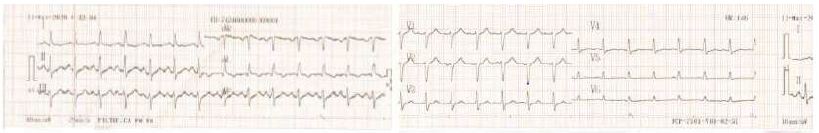
Figure 1: Electrocardiogram performed at H0 + 10 min

Figure 2: Chest X-ray (prone position) at H0 + 30 min
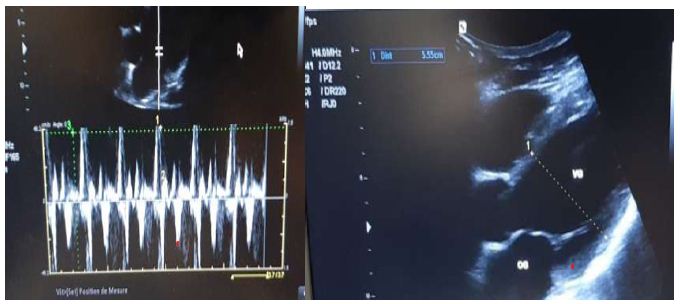
Figure 3: Cardiac echography (Fast echo under Dobutamine) H0 + 30mn
At H0+8H we objectified a clinical improvement with disappearance of the signs of cardiogenic shock, the SBP always lower than 100 mmHg, the diuresis was 1000 ml in 8 hours. The crackles had descended to the bases of the lungs; the sounds of galloping persisted.
The tube coagulation test had objectified clots which crumbled easily after 30 minutes (coagulopathy). Serum creatinine was 21 mg. The complete blood count had objectified a hemoconcentration with a hemoglobin level of 21.8 g/dl, hematocrit at 75%, a white count at 11,700/mm3; platelets at 258,000/mm3; troponin I was positive at 3.07 ng/ml. Hepatic transaminases were: AST at 91 U/L and ALAT at 33 U/L.
We concluded that there was grade 3 scorpion envenomation complicated by cardiogenic shock with massive AO, coagulation disorders and probably functional renal failure. It is an acute myocarditis with a cardiogenic and/or lesional APO.
At H0+12H the patient is conscious cooperative, with a RR at 20 cycles/min, a saturation at 97% under oxygen, but a SBP lower than 90 mmHg under Dobutamine. He persisted with galloping noises with an HR greater than 120 beats/min. The crackles have completely disappeared.
At H0+2 p.m., the patient underwent medical evacuation under continuous oxygen therapy and Dobutamine by medicalized flights to Dakar in Senegal (level 3 health structure).
After three days (D3) of hospitalization at the Principal Hospital of Dakar, the clinical condition of the patient had improved, he had been completely weaned from Dobutamine. The cardiac ultrasound performed had objectified a ventricle with a size limit of 55 mm with a left ventricular ejection fraction of 55%. The patient was declared unfit as a precaution for the continuation of his mission in this particularly trying military theater for the organisms.
Comments
Scorpion stings are more common in tropical areas such as northern Mali where temperatures reach up to 45°C. Local populations and missionaries engaged in this area are exposed to scorpion stings [4].
In this area of the Saharan strip, the majority of stings occur during the hot period (from April to August) when the activity of the scorpion is maximum [5,6] as was the case in our patient. This would be explained by the nature of scorpions, which are thermophilic arthropods that go into hibernation at the start of the cold seasons.
Sorpionic envenomations are classified into three grades [7] depending on the severity of the systemic manifestations. In 90 to 95% of cases, the sting is limited to grade 1 local manifestations (very sharp pain and local neurological signs). Grade 2 combines hypertensive flare-ups, fever, sweats, chills, priapism, abdominal pain, vomiting, excessive sweating and marks an evolutionary turning point towards grade 3. The latter is characterized by: consciousness disorders of various depths, respiratory distress, cardiovascular shock, as in our victim. Systemic manifestations appear between the 3rd and 15th hour after the bite [7].
The active components of dangerous scorpion venom for humans are peptide neurotoxins that cause the release of mediators (cathecholamines, and acetylcholine). Stimulation of the sympathetic system leads to an adrenergic discharge responsible for tachycardia and a hypertensive attack at the beginning. On the other hand, stimulation of the parasympathetic system is at the origin of the cholinergic syndrome, hence vomiting and abdominal pain [8].
Cardiovascular failure results from 3 main mechanisms: adrenergic myocarditis occurring under the effect of a massive discharge of catecholamines, toxic myocarditis caused by direct action of the venom on the myocardial tissue and myocardial ischemia due not only to the discharge of catecholamines but also to the action of cytokines and/or neuropeptide on the coronary vessels [9-11].
Our patient presented the three characteristics of scorpion heart disease that make it original: severity (profound alteration of cardiac function), biventricular damage, and its reversibility [12]. This character increases the similarities between scorpionic cardiomyopathy and stress cardiomyopathy having as common denominator, the intense discharge of catecholamines.
APO can be mixed: cardiogenic and lesional. The mechanisms involved in cardiogenic APO are multiple [10,12]: increase in systemic BP and peripheral vascular resistance (PVR) in the first 120 minutes following the puncture, a drop in left ventricular compliance by sudden elevation of end-diastolic pressures of the left ventricle as evidenced by the restrictive filling flows in our victim.
Lesional APO is related to a direct action of the venom at the pulmonary level causing inflammation and pulmonary capillary hyperpermeability [10,13]. It is for this reason and to minimize the side effects of Scorpion Venom Antiserum that we added corticosteroid therapy to the care of our patient.
The antivenom used was Scorpion Venom Antiserum IHS® active on the venom of Androctonus amorous and Leiurus quinquestriatus. Its administration must be as soon as possible after a scorpion sting to be more effective, especially in areas where dangerous species live [14]. Unlike snake antivein serums, Scorpion Venom Antiserum is not available or accessible to our populations in the Saharan strip.
Conclusion
Scorpion stings are common in tropical Africa. Scorpion envenomation can manifest as local signs, whether or not followed by general signs. The cardio-respiratory attack constitutes the most formidable complication threatening in the short term the vital prognosis of the victim. Scorpion heart disease is biventricular, severe but reversible subject to appropriate and effective early treatment.
References
- Isbister GK, Bawaskar HS (2014) Scorpion Envenomation. N Engl J Med 371: 1557-1560.
- Dabo A, Golou G, Diarra N, Goyffon N, Doumbo O (2011) Scorpion envenoming in the North of Mali (West Africa): Epidemiological, clinical and therapeutic aspects. Toxicon 58: 154-158. [crossref]
- Chippaux JP, Goyffon M (2008) Epidemiology of scorpionism: a global appraisal. Acta Trop 107: 71-79. [crossref]
- Goyffron M, Billiald P (2007) Envenimation VI- Le scorpionisme en Afrique. Med Trop 67: 439-446.
- Ben Othman A, Ben Abdallah N, Aoun MB (2016) The scorpion envenomation in the region of Faouar-KEBILI at 2010-2012 : study of 421 cases. Tunis Med 94: 102-106. [crossref]
- Bahloul M, Chabchoub I, Chaari A, Chtara K, Kallel H, et al. (2010) Scorpion Envenomation Among Children: Clinical Manifestations and Outcome (Analysis of 685 Cases). Am J Trop Med Hyg 83: 1084-1092. [crossref]
- Elatrous S, Besbes-Ouanes L, Fekih Hassen M, et al. (2008) Les Envenimations Scorpionnique Graves. Med Trop 68: 359-366.
- Chippaux JP (2012) Emerging options for the management of scorpion stings. Drug Design, Development and Therapy 6: 165-173. [crossref]
- Hamouda C, Ben Salah N (2010) Envenimations scorpioniques en Tunisie. Med Emergency 5: 24-32.
- Bahloul M, , Regaieg K, Chabchoub I, Kammoun M, Chtara K, et al. (2017) Les envenimations scorpioniques graves: physiopathologie et rôle de l’inflammation dans la défaillance multiviscérale. Médecine et Santé Tropicales 27: 214-221.
- Bouaziz M, Bahloul M, Hergafi L, Kallel H, Chaari L, et al. (2006) Factors associated with pulmonary edema in severe scorpion sting patients: a multivariate analysis of 428 cases. Clin Toxicol (Phila) 44: 293-300. [crossref]
- Hajiba A (2015) Epidémiologie et facteurs pronostiques des envenimations scorpioniques dans le service de réanimation pédiatrique du CHU de Marrakech [Thèse]. Marrakech-Safi.
- Bisbahloul M, Kallel H, Rekik N, Hamida CB, Chelly H, et al. (2005) Atteinte cardiovasculaire lors d’envenimation scorpionique grave: Mécanismes et physiopathologie . La Presse Médicale 34: 115-120.
- Ndiaye AM, Niang C, Dembele M, et al. (2017) Envénimation scorpionique grave chez un militaire sénégalais en mission de maintien de paix au Darfour. Revue Internationale de Santé des Forces Armées 90: 79-82.