Abstract
A major hazard to world health is the global pandemic of preeclampsia (PE risk. It is acknowledged as a chronic, incapacitating illness with major complications. This finally leads to the untimely death of both the mother and the fetus. It also drastically reduces life expectancy, can result in multi-system morbidities, and raises healthcare expenses. Regardless of knowledge, all forms of preeclampsia result in unacceptably high stress for Imo State in terms of people and society. Therefore, this study focused on Imo State in Southeast Nigeria to examine the knowledge impact of the hazards related to pre-eclampsia during pregnancy. In this investigation, both descriptive and analytical study designs were used. Target, stratified, and random sampling were all used as data collection methods. The sample size included 3690 individuals from different parts of the state. Data collection for the study was done using questionnaires. With the generated data, tables and charts were made. In terms of statistics, Chi-square analysis was used to determine the difference between patient and individual knowledge of risk factors. Out of 2700 persons that responded to the question on whether they know about risks of preeclampsia, 68% of them representing 1761said “Yes”, while 32% representing 829 said “No”; a chi-square contingency analysis on the respondents’ knowledge of risks of preeclampsia yielded a value of 70.6764 (p<0.05). On whether they know if they are living with risks of preeclampsia, 829 out of 2700 respondents which represent (11.33%)of the responses said “Yes”, while 2340 which accounted for (88.67%) of the responses said “No”. This puts the prevalence rate at 11.33%, but blood pressure screening results puts the prevalence rate at 39.00%. When asked if they know their blood pressure, 31% of the respondents which accounted for 811±7.8 out 2700 responses said “Yes”, while 61.00% representing 1494±2.1490 out 2700 said “No”; a chi-square contingency analysis gave a value of 152.7232 with a p-value of <0.001 indicating very high significant difference. Also, great percentage of the respondents has idea of hereditary as risk factors that associated with risks of preeclampsia. Pregnant women in Imo state are not well informed about PE. Higher education is a key element that promotes adequate knowledge of physical education.
Keywords
Impacts, Imo State, Pre-eclampsia, Risks, Knowledge
Introduction
Preeclampsia (PE) is a multisystem illness associated with pregnancy that lacks a known cause. PE’s underlying cause is currently being researched. It is believed to happen in two stages, though. The first stage includes the impairment of local placental hypoxia and fetal trophoblastic invasion of the decidua. The second stage involves abnormal production of pro-inflammatory, antiangiogenic, and angiogenic factors as well as the release of placental blood-related substances into the maternal circulation [1].
Elevated blood pressure and proteinuria are the typical symptoms of Preeclampsia, and the clinical manifestation often starts around the 20th week of pregnancy or later in the pregnancy, regressing after delivery. Early-onset PE (occurring before 34 weeks of gestation) and late-onset PE (occurring beyond 34 weeks of gestation) are the two primary kinds. Early-onset PE is linked to higher odds of problems than late-onset PE, including preterm birth, fetal growth restriction, and maternal morbidity and death [2]. This is true even if the presenting characteristics of early- and late-onset PE may overlap. Women living with Preeclampsia also exhibit a variety of indications and symptoms that are related to various organ systems. The multi-organ system dysfunction in Preeclampsia frequently results in headaches, visual abnormalities, abnormal renal function, severe hypertension, chest pain, pulmonary oedema and low oxygen saturation, nausea, and abnormal liver function, among other symptoms. First pregnancy, age (pregnancy after 18 or at an advanced age), family history of Pre-eclampsia, personal history of Pre-eclampsia, obesity, gestational diabetes, multiple pregnancy, and preexisting illnesses such chronic hypertension are all risk factors for Pre-eclampsia [3].
According to reports, Pre-eclampsia complicates 2-8% of pregnancies globally and up to 10% in underdeveloped nations, making it one of the top causes of maternal mortality and morbidity. Very high percentage of Imo people are thought to have Pre-eclampsia. It is one among the top five killers of pregnant women and newborns. PE can develop into eclampsia, which can result in adverse fetal outcomes like preterm birth, small-for-gestational-age babies, placental abruption, and perinatal death. It can also raise the risk of cardiovascular and cerebrovascular diseases, as well as venous thromboembolism in later life .Additionally, women with Pre-eclampsia are more likely to experience postpartum depression and other mental health problems such shame, remorse, failure-related feelings, a sense of loss of control, and post-traumatic stress disorder [4].
Adequate understanding of a disorder aids in its management, control, and prevention. According to reports, people who are knowledgeable about their disease are more likely to adhere to therapy and experience fewer difficulties. The slow reporting of women to healthcare facilities after experiencing a sign or symptom in Imo State Nigeria is a significant barrier in the fight against Preeclampsia. Preeclampsia is a disease with visible signs and symptoms that needs to be treated right away. With the right information, women experiencing Preeclampsia would notify the hospital sooner, receive treatment sooner, and experience fewer negative effects. This highlights how important it is for women to understand the disease fully [5,6].
In order to accomplish this, it is necessary to evaluate the pre-existing knowledge about Preeclampsia, particularly among high-risk groups like pregnant women. Previous research from the Nigeria and a few African nations suggests that women generally have little awareness of PE [7]. However, there isn’t a study available right now that assesses Imo State’ level of Preeclampsia knowledge.
Due to a lack of reliable statistical information, it is difficult to establish full understanding on Risks Associated with Preeclampsia during Pregnancy in Imo State. The goal of the current study is to contrast the risks associated with preeclampsia during pregnancy in Imo State, Nigeria. The results of this analysis should help Imo State, Nigeria, establish efficient preeclampsia management and general prevention efforts.
Materials and Methods
Study Area
The study was carried out in Nigeria’s Imo State. One of Nigeria’s 36 States, Imo State is situated in the Southeast geopolitical zone. Imo State has an area of roughly 5,100 sq km and is located between latitudes 4°45’N and 7°15’N, as well as longitudes 6°50’E and 7°25’E. It is bordered on the east by Abia State, on the west by Delta State and the River Niger, on the north by Anambra State, and on the south by Rivers State. Isu, Okigwe, Oguta, Orlu, Mbaise, Mbano, Mbaitoli, Mbieri, Orodo, Nkwere, and Orsu are among Imo State’s important cities in addition to Owerri [8].
Study Design
This study used both descriptive and analytical study designs [9]. This included the knowledge of risks connected to pregnancy-related pre-enclampsia. Analytical design was utilized to analyze the distribution’s determinants, whereas descriptive design was employed to evaluate the risks associated with pre-enclampsia during pregnancy.
Survey Methods and Sampling Technique
The survey methods used in this study were random, target, and stratified sampling [10]. Random sampling was used to gather data from the LGAs, target was used to gather data from the hospitals, and stratified was used to gather data for the entire state, in which case each LGA was used as a stratum.
Sample Size
With survey software’s sample size calculator, the confidence interval and level were set at 5% and 90%, respectively. The distribution of Imo State’s population by gender, age, profession, and other factors is not known with any recent accuracy. The official 2006 census served as the foundation for this study’s population estimations. It is reported that Imo State had 3,927,563 people living there as per the official census from 2006. According to projections, the population will increase by 3.3% from 2006 to reach 5,408,800. Males made up 1,976,471 (or 50.3%) of the population in 2006, while females made up 1,951,092 (or 49.7%). There is no discernible difference in the proportion of men and women.
One can extrapolate from the aforementioned facts since there was no official information available regarding the number of women of childbearing age. Groups of people aged 0 to 14 (1,415,929) and 65 and older (170,069) were not included because they were either too young or too old. The group of people aged 15 to 64 (2,341,565) has now left. 49.7% of the population was female overall in 2006. From the entire 15- to 64-year age range, the female population was estimated as 0.497 × 2,341, 565=1,163,75.
Questionnaire 1: 2700 (no of questionnaires administered to each LGA depended on the population of the LGA) respondents for the general populace.
Questionnaire 2: 540 (20 from each LGA) respondents for the category of Risks Associated with Pre-enclampsia during pregnancy.
Method of Data Collection
Research instrument for data collection was questionnaires and materials such as blood pressure measuring kits, measuring tape and weighing balance was used for physical examination.
Questionnaires
Well-structured questionnaires were used to obtain data from respondents; the questionnaires were arranged in the following order:
Questionnaire 1
This was used to indicate information from the general populace. It was organized into knowledge impact of Risks Associated with Preeclampsia during pregnancy
Ethical Consideration
Before administering surveys to respondents, letters of approval or authorization were submitted for the management of health institutions’ approval. Additionally, before giving out questionnaires, those who had Risks Associated with Preeclampsia during Pregnancy were asked for their permission. Before administering the questionnaires to the broader public, a similar consent was requested.
Data Presentation and Statistical Analysis
The association between the risks of preeclampsia during pregnancy and age was measured using correlation and regression analysis, in which case r (correlation coefficient) and r2 (coefficient of simple determinant) were obtained using SPSS statistical software version 17.0.
Tables and charts with the generated data were created. Data that were produced in accordance with various parameters that were taken into consideration in this study were measured for correlation using descriptive statistics, including mean, relative standard error, and standard deviation. Version 17.0 of the statistical program SPSS was used for this [11]. Patients’ perceptions of risk factors for preeclampsia and complications were evaluated using chi-square.
Utilizing computer-aided software, GenStat Statistical Software, the coefficient of variation (% CV), which measures variability, was calculated for the data collected from the various LGAs.
Results
This research work on knowledge impacts of Risks Associated with Pre-eclampsia during pregnancy in Imo State. The data and results that were obtained from this research study were presented in Tables (Figures 1 and 2).
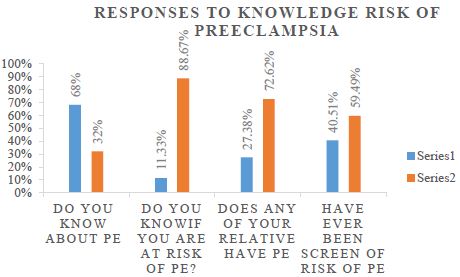
Figure 1: Responses to knowledge risk of preeclampsia.
Knowledge of risk of preeclamsia (1) The results showed that 1761 (68%) respondents answered positively to knowing about risk of preeclamsia while 829 (32.00%) responded negatively to knowing about preeclamsia. A chi-square statistical test yielded a value 70.6764 (p< 0.0526) which was very significant at p< 0.05.
The result on whether the respondents knew whether they were living with risk of preeclamsia showed that 299 (11.33%) knew they were living with risk of preeclamsia while 2340 (88.67%) did not know if they were living with risk of preeclamsia. A 27 x 2 contingency chi-square test of significance gave a value of 13964.021 (p<0.0000) which was significant at p<0.001.
Greater percentage of the respondents which represented 1883 (72.62%) answered negatively to having a relative with risk of preeclamsia while 710 (27.38%) responded positively to having relatives with risk of preeclamsia. A chi-square test gave a value of 58.4932 (p=0.2808) which was not significant at p>0.05.
The results showed that 1056 (40.51%) of the respondents have never been screened for risk of preeclamsia while 1551 (59.49%) respondents have been screened for risk of preeclamsia before. A chi-square test of significance gave a value of 93.493 (p=0.0005) which was very highly significant at p<0.05.
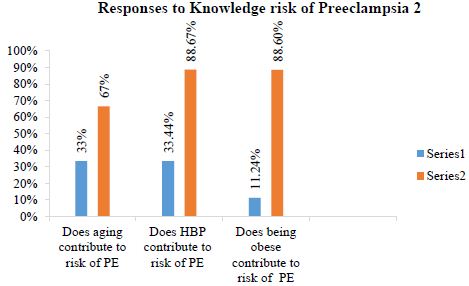
Figure 2: Responses to Knowledge risk of Preeclampsia 2.
Knowledge of risk of preeclampsia (2) The second section on the knowledge of risk of preeclampsia (2) is shown in Table 2 below. 850 (33.44%) respondents answered ‘Yes’ to knowing their aging contribute to Risk of preeclampsia while 1692 (66.56%) respondents answered ‘No’ to knowing their aging contribute to Risk of preeclampsia. A chi-square test of significance having degree of freedom of 26 yielded a value of 115.7206 (p<0.001) which was very highly significant at p<0.05.
955 (39.00%)respondents answered ‘Yes’ to knowing their blood pressure level while 1494 (61.00%) respondents answered ‘No’ to knowing their blood pressure level. A chi-square test of significance yielded a value of 152.7232 (p<0.001) which was very highly significant at p<0.001.The results equally showed that majority of the respondents did not know their blood pressure level.
On whether the respondents knew being obese contribute to risk of preeclampsia, 257 (11.24%) respondents answered ‘Yes’ to knowing that being obese contribute to Risk of preeclampsia while 2030 (88.76%) respondents answered ‘No’ to knowing that being obese contribute to Risk of preeclampsia. A chi-square test of significance having degree of freedom of 26 yielded a value of 71.2682 (p=0.047775) which was very highly significant at p<0.05.
Discussion
Preeclampsia Risks in Imo State: The Impact of Knowledge
Preeclampsia risks have been shown to have a negative impact on Imo State people. Other studies have measured knowledge status using a number of characteristics, including career, education, income, or regional deprivation. Numerous facets of knowledge state may be represented by these markers [12].
One of the reasons for poor performance at work has been linked to preeclampsia risk. Preeclampsia knowledge increases the likelihood that a woman will be at low risk. Obesity and blood pressure are associated with higher preeclampsia risks and also have worse knowledge levels [13]. The fact that most participants were aware of PE, primarily due to awareness of chronic hypertension, can be linked to the population’s lack of knowledge of PE. However, only a small percentage of people were well informed on the signs, causes, and complications of PE.
Preeclampsia is now well acknowledged as a potential problem. It is immediately identified as “high blood pressure in early pregnancy” due to its alarming nature. Almost everyone who was tested or interviewed in this study referred to the illness that was being studied as a “sickness that hurt the embryo [14].
This suggests that most people in Imo State were already aware of the disease. Preeclampsia is a risk that many people in the state acknowledged, although a sizable portion of them did not know about other preeclampsia risks. Contrary to the fact that they were aware of the sickness, many did not know what their blood pressure was. This shows that many people, whether they have preeclampsia or not, have not been diagnosed with the risks associated with the condition or do not care to know what their blood pressure is [15].
Pre-eclampsia often begins after 20 weeks of pregnancy in women whose blood pressure was previously normal. The mother and the kid could both encounter serious, perhaps fatal, issues.
There might be no symptoms. High blood pressure and protein in the urine are important indicators. However, it could be difficult to distinguish between this and an usual pregnancy [16].
Pre-eclampsia is commonly managed with oral or intravenous medication until the infant is old enough to be delivered. In many cases, this entails weighing the risks of an early birth against those of chronic pre-eclampsia symptoms. Pre-eclampsia is responsible for 9% of maternal mortality in Africa and Asia and problems in 2-8% of pregnancies worldwide [17]. Globally, the majority of deaths attributed to pregnancy-associated hypertension diseases occur in underdeveloped countries. According to the World Health Organization, pre-eclampsia is projected to occur seven times more commonly in less developed countries (2.8% of live births) than in more developed ones (0.4%) [18,19]. Imo State, Nigeria, has a higher and nearly twice as high prevalence rate when compared to the rest of the world and the continent of Africa. It’s possible that Imo State in Nigeria’s rising crises is to blame for this high incidence. The genesis of preeclampsia may be influenced by maternal, paternal, and fetal genetic factors, according to early family-based research. According to the WHO, with a 2.8 prevalence rate, there are about three new cases every 40 seconds, or close to 10 million cases per year [20]. In Imo State, four new cases would consequently occur every 40 seconds, with a prevalence rate of 11.33%. According to observation, the largest rises are anticipated to take place in regions with a majority of developing economies. Imo State is located in Nigeria, where emerging economies are the majority. This makes Imo State’s situation worse.
Without concerted efforts to halt it in its tracks, the prevalence rate of 11.33% in Imo State would likely rise to greater levels in the upcoming years, which is quite concerning. Throughout the course of the study, more residents of Imo State were discovered to be ignorant about their preeclampsia risks. After being admitted to the hospital or when their health has gotten worse, they only realize they are at risk for preeclampsia [21,22].
Preeclampsia concerns have also resulted in restrictions on movement in preeclampsia patients due to increased blood pressure. As a result, it makes social interaction between people take longer. However, given factors that affected awareness of PE were not static or general demographic factors, the low knowledge of PE found in this study might be improved. Evidently, after controlling for confounders that could have confounded the association, the high educational level was the only significant factor that was independently associated with adequate knowledge of PE. This study suggests that efforts to reduce PE-related fatalities in Imo State might be greatly aided by the employment of an efficient method of teaching women, possibly at prenatal appointments and through media channels. Indeed, it has been demonstrated that increasing patient understanding of PE encourages earlier reporting of signs and symptoms, which can result in prompt treatment and better health outcomes for both the mother and the infant.
Conclusion
Residents of Imo State are increasingly at risk for preeclampsia, as many sufferers are unaware of their illness. Preeclampsia chances varied across the state based on factors like knowledge.
Indeed, few pregnant women are aware of preeclampsia. A higher degree of education is a key element that promotes adequate knowledge of physical education. This emphasizes the necessity of stepping up efforts to increase women’s knowledge about PE in order to enhance pregnancy outcomes. Education may be provided through national education programs, media platforms, or contextual health education at Antenal care.
References
- Morton CH, Seacrist MJ, VanOtterloo LR, Main EK. (2019) Quality improvement opportunities identified through case review of pregnancy-related deaths from preeclampsia/eclampsia. J Obstet Gynecol Neonatal Nurs 48(3): 275-287. [crossref]
- Das S, Das R, Bajracharya R, Baral G, Jabegu B, Odland JØ (2019) Incidence and risk factors of pre-eclampsia in the paropakar maternity and women’s hospital, Nepal: A retrospective study. Int J Environ Res Public Health 16(19): 1-8. [crossref]
- com.ng (2022). Imo State History, Local Government Area, and Senatrial Zones/Districts. [crossref]
- Ebrahimi A, Sayad B, Rahimi Z. (2020) COVID-19 and psoriasis: biologic treatment and challenges.J Dermatolog Treat. J Dermatolog Treat 1-5. [crossref]
- Belay AS, Wudad T. (2019) Prevalence and associated factors of pre-eclampsia among pregnant women attending antenatal care at Mettu Karl referral hospital, Ethiopia: cross-sectional study. Journal of Clinical Practice 25(1): 14. [crossref]
- World Health Organisation’ (2011). WHO recommendations for prevention and treatment of preeclampsia and eclampsia. [crossref]
- Wandabwa J, Doyle P, Kiondo P, Campbell O, Maconichie N, Welishe G. (2010) Risk factors for severe pre-eclampsia and eclampsia in Mulago Hospital, Kampala, Uganda. East African Medical Journal 87(10): 415-424. [crossref]
- Stevens W, Shih T, Incerti D, Ton TGN, Lee HC, Peneva D. (2017) Short-term costs of preeclampsia to the United States health care system. Am J Obstet Gynecol 217(3): 237-248.e16. [crossref]
- Nnodim J, Emmanuel N, Hope O, Nwadike C, Ukamaka E, Christian O. (2017) Membrane potential, serum calcium and serum selenium decrease in preeclampsia subjects in Owerri. Universa Medicina 36(2): 88-93.
- Siddiqui A, Deneux-Tharaux C, Luton D, Schmitz T, Mandelbrot L, Estellat C (2020) Maternal obesity and severe pre-eclampsia among immigrant women: a mediation analysis. Sci Rep 10(1): 1-9. [crossref]
- Ajah LO, Ozonu NC, Ezeonu PO, Lawani LO, Obuna JA, Onwe EO. (2016) The Feto-Maternal Outcome of Preeclampsia with Severe Features and Eclampsia in Abakaliki, South-East Nigeria. Journal of Clinical Diagnostics and Research 10(9): QC18-QC21. [crossref]
- Amaral LM, Wallace K, Owens M, LaMarca B (2017) Pathophysiology and Current Clinical Management of Preeclampsia. Curr Hypertens Rep 19(8): 616. [crossref]
- Vidaeff A, Pettker CM, Simhan H (2019) Gestational Hypertension and Preeclampsia ACOG PRACTICE BULLETIN. Clinical Management Guidelines for Obstetrician-Gynecologists. Am Coll. Obstet Gynecol 133(1): 1–25. [crossref]
- Williams PJ and Broughton Pipkin F (2011) The genetics of pre-eclampsia and other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol 25: 405-417. [crossref]
- Cerdeira AS, O’Sullivan J, Ohuma EO. (2019) Randomized interventional study on prediction of preeclampsia/eclampsia in women with suspected preeclampsia: INSPIRE. Hypertension 74: 983-990. [crossref]
- Churchill D, Duley L, Thornton JG, Moussa M, Ali HS, Walker KF. (2018) Interventionist versus expectant care for severe pre-eclampsia between 24 and 34 weeks’ gestation. Cochrane Database Syst Rev 10: CD003106. [crossref]
- Chappell LC, Brocklehurst P, Green ME (2019) Planned early delivery or expectant management for late preterm preeclampsia (PHOENIX): a randomised controlled trial. Lancet 394: 1181-1190. [crossref]
- Bellamy, L, Casas, J, Hingorani, AD, Williams, DJ. (2007) Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. British Medical Journal 335: 974-985. [crossref]
- Birhanu MY, Temesgen H, Demeke G, Assemie MA, Alamneh AA, Desta M, et al. (1995) Importance of matrix metalloproteinases in human trophoblast invasion. Early Pregnancy 1(4): 263-269. [crossref]
- Gray KJ, Kovacheva VP, Mirzakhani H, Bjonnes AC, Almoguera B, Wilson ML, et al (2018) Gene-Centric Analysis of Preeclampsia Identifies Maternal Association at PLEKHG1. Hypertension 72(2): 408-416. [crossref]
- Duhig KE, Myers J, Seed PT (2019) Placental growth factor testing to assess women with suspected pre-eclampsia: a multicentre, pragmatic, stepped-wedge cluster-randomised controlled trial. Lancet 393: 1807-1818. [crossref]
- Hayes-Ryan D, Khashan AS, Hemming K (2021) Placental growth factor in assessment of women with suspected preeclampsia to reduce maternal morbidity: a stepped wedge cluster randomised control trial (PARROT Ireland). BMJ 374: n1857. [crossref]