Abstract
Globally, breastfeeding and obesity have become paramount importance for mothers and infants. This paper aimed at reviewing the literature to explore the evidence that maternal obesity can have a negative impact on breastfeeding rates. A review of the literature (academic journals) was conducted between 2005 and 2019 using the PRISMA 2009 and critical appraisal approach to critically evaluate the articles and reach an evidence statement.
Concerning the research question of the study, twelve research articles were considered for review. The review found maternal obesity/overweight as independent variables (defined as Prepregnancy or postpartum Body Mass Index) and breastfeeding rate as the dependent outcome variable.
The majority of the studies showed evidence of a negative impact of obesity on breastfeeding rates. Therefore, to understand breastfeeding behavior among obese women, researchers could consider conducting more empirical studies that use well-established theories, including the theory of reasoned action. This review may help clinicians recognize patients who are less likely to breastfeed and consider targeting early intervention.
Background
It is known globally that obesity has become a widespread public health problem. For example, in Nebraska, United States of America (US), the prevalence of adult obesity is reported to be 32.8% (up from 11.3% in 1990) and is ranked the 15th highest rate of obesity in the nation [1]; in addition to, increasing prevalence of obesity in the Arab World including Jordan, Kingdom of Saudi Arabia, United Arab Emirates and others [22,23]. The degree of obesity is measured by the Body Mass Index (BMI) that calculates weight in relation to squared height. BMI between 25 -29kg/m2 is classified as overweight and 30 kg/m2 or higher as obesity [2]. The burden of disease due to obesity extends beyond conventional health consequences to include social, psychological, emotional, economic, and societal costs [3-5].
Obesity is more common among women [6]. Research has indicated that the risk of emerging a variety of non-communicable diseases, including cardiovascular diseases, diabetes, arthritis, infertility, and breast cancer, increases among obese women [7,8]. Successful breastfeeding (BF) is a relatively complex process that begins even before the birth of the baby. Studies show that the first step is the woman’s intention to breastfeed, successfully initiating BF, and then successfully maintaining that process. For optimal benefits for both baby and mother, most authorities recommend exclusive BF to continue for up to six months [9].
BF is an integral part of developing the infant’s brain and body and impacts its health as it grows [10]. Medical conditions such as childhood obesity, gastroenteritis, and type 2 diabetes are increasingly seen among children who are breastfed at lower rates [11]. BF also affects mothers’ health, where there is a decreased risk of postpartum hemorrhage and type 2 diabetes as well as other conditions such as breast, uterine, and ovarian cancers [12].
Several maternal inputs determine the success of the BF process. Medical, socioeconomic, psychosocial, and lifestyle aspects have been repeatedly cited as factors associated with BF practice [13]. Maternal obesity has emerged as yet another element that might negatively impact BF [14-19]. This phenomenon is emerging as a public health concern globally. Referring to the earlier example, in Nebraska, fewer than fifty percent of infants are BF at six months of age, and only 20% are exclusively breastfed at that age. This paper aims to review the literature to explore the evidence that maternal obesity can negatively impact BF rates. This may help clinicians recognize patients who are less likely to breastfeed and consider targeting early intervention at women who are thought to be at a higher risk. The definition of BF rates can be referred to as: “ever breastfed refers to those infants who have been put to the breast, even if only once; and exclusive breastfeeding concerns infants who have only received breast milk during a specified period of time. The cut-off points regarding the duration of exclusive-breastfeeding – 3, 4 and 6 months – are in line with past and current WHO guidelines [13,57]”.
Literature Review
Context
Globally, obesity prevalence is three times since 1975. In 2016, more than 650 million adults were classified as obese, which accounts for 13% of the world’s population; 40% of them were women, according to a 2018 report World Health Organization [20]. The cause of obesity is multiple factors, including physical activity levels, dietary patterns, medication use, food, and education [21]. The Center for Disease Control and Prevention (CDC) reported on obesity as a serious concern due to its association with reduced quality of life, poorer mental health outcomes, and the leading causes of death across the US and extending globally, including diabetes, stroke, heart disease, and cancer [21].
Within Eastern Mediterranean Region (Middle East), seven countries population (adults) were ranked among the ’20 most overweight nations’, including Kuwait (73.4%), Qatar (71.7%), Kingdom of Saudi Arabia (69.7%), Jordan (69.6%), Lebanon (67.9%), United Arab Emirates (67.8%) and Libya (66.8%) [22,23]. Reports from the International Diabetes Federation stated that there were 374,100 new cases of diabetes report in Jordan as an example and are mostly related to obesity [22]. Women suffer more from obesity, especially when they get pregnant. The World Health Organization reports that obesity is a major problem among Jordanian women, with 40% [20,27]. A Jordanian national survey in 2007 showed that obesity is most prevalent among women of reproductive age. From the research report, some of the critical factors for obesity amongst women included marriage at an early age, wealth status, parity, lack of appropriate place for women to exercise, and smoking [20,27].
It is undoubtedly known, there is a global recognition of the advantages of BF for both mothers and infants [1-3]. BF has been lately described as “personalized medicine.” For newborns, the new series published in 2016 by Lancet noted critical evidence demonstrating the notion of BF as a vital cornerstone of children’s survival, growth, health, and development, and thereby associated positively with life expectancy and prosperous future [24]. Additionally, the Lancet series highlights the economic benefits of BF. For instance, it was found that babies who were not breastfed across countries faced financial losses of over $300 billion annually due to the lowered cognitive ability levels, resulting in reduced earning capacity for these persons [24]. The World Health Organization noted the importance and benefits of exclusive breastfeeding (EBF) having more significance and positive social impact in settings of poor nutrition, poverty, and poor personal hygiene, where the baseline disease rates are higher [1,5,58]. Annually, the lives of over 800,000 children less than five years of age can be saved provided that optimal BF is administered [24,25,60].
About twenty percent of neonatal deaths may be prevented with BF initiation within the first hour after birth [7,8,58] in low-income and middle-income countries. Furthermore, the continuation and optimal BF practices have the potential of preventing at least twelve percent of all under-5 deaths [9,26,58]. Research studies have indicated that children who are exclusively breastfed are less vulnerable to developing associated childhood illnesses and fourteen times more likely to combat ill-health than those who are not breastfed [10,26,58,59]. The EBF rates prevalence is lower, and childhood mortality is higher among low-income and middle-income countries [27,58]. In Jordan and Ghana, for instance, the documented rate of infant mortality is 17 per 1000 live births and 53 per 1000 live births; while, the mortality rate of children younger than five years is 21 per 1000 live births and 31 per 1000 live births, and these death rates are moderately related to lowered prevalence of EBF practices, respectively [27,58].
Prevalence
For the first six months, postpartum, early initiation of BF and EBF are strongly endorsed [12]. Globally, the rate of BF initiation is sub-optimal [12,60]. Despite the significant developments in some World Health Organization (WHO) regions, the prevalence of EBF remains of great concern to low-and medium-income countries, as illustrated in a study using data from 66 countries [13,60]. The study reviewed the prevalence of EBF among infants younger than six months for fifteen years, from 1995 to 2010. This study revealed that most EBF among infants increased from 33% in 1995 to 39% in 2010 across developing countries [13,60]. The WHO 2009 report showed that the prevalence of EBF rate (39%) is globally low; within in low-income and medium countries, there is a 36% EBF rate [2,13,60].
In 1997 Jordan, the Demographic and Health Survey (DHS) indicated that the rate of EBF was twelve percent among babies less than six months old [27]. The prevalence of EBF fluctuated for many years in Jordan; in 2002, EBF was 26.7%, then dropped to 22% in 2007, and then had a slight increase to 23% and 26% in 2012 and 2017, respectively [27]. Several Jordanian cross-sectional studies reported suboptimal BF initiation rates ranging from 13% to 19% [27]. Eastern Mediterranean Regional (Middle East Region) data about BF and EBF are not well reported from the Arab World, and cross-sectional studies collect most data. In Saudi Arabia, the rate of initiation of BF among Saudi mothers was at 92%, as compared with the prevalence of initiation of BF as 98% in the United Arab Emirates and 57% in Qatar [28,60].
Barriers
Many factors were identified as obstacles to infant feeding traditions, proper dietary nutrition [13,58]. Some literature relates the lack of BF or even reluctance to do so to poor maternal knowledge or attitude of the mother and maternal and infant medical conditions. Several studies have identified other important factors related to health providers’ attitudes and practices and supportive policies and enabling health facility infrastructure. Several published Jordanian studies reported several adverse challenges and obstacles that influence the initiation and EBF. Of these, Dasoki et al., and Khassawneh et al., showed that Cesarean births and no endorsement of BF initiation policies were obstacles to BF [28-30]. Abuidhail [31] reported that mothers expressed that infants remained hungry after BF. Abu Shosha [32] showed that short intervals between pregnancies and physical breast problems during BF were addressed. Additionally, Khassawneh et al. [28,29] reported the place of work as another obstacle that contributed to mothers’ inability or desirability to practice BF.
Moreover, studies showed that women commonly said they did not intend to practice BF on their newborns, particularly EBF in the first six months [27-32]. Such an intention may be due to the limitations of social support and systems and the challenges posed in the workplace. In these studies, respondents shared concerns about the side effects when mothers BF, in terms of perceived pain and changes in body figure and weight [27-32]. Based on the above-given reasons for not practicing BF, women may be influenced by the knowledge, attitudes, and practices across countries. Adequate knowledge about EBF is the fundamental tool that can direct EBF practice among mothers [27-29]. Therefore, this review paper’s main objective is to review the literature to explore the evidence that maternal obesity can negatively impact BF rates.
Methods
This literature review’s search strategy involved visiting the EBSCO HOST web and Academic Search Premier, PubMed, Web of Science, CINAHL plus full text, Science Direct, EMBASE, Bio Med Central, Wiley online Library, All Health Watch and MLA International Bibliography databases. The inclusion criteria specified peer-reviewed scholarly research articles published in academic journals between 2005 and 2019, full text with references available and English. Items were excluded from the review if they did not answer the research question; if they tackled obesity in children, men, or women who had not given birth; if they were reviews of literature of any kind or if they fell outside the specified search period. A variety of keywords were used, including BF, BF behavior, BF practices, lactation, BMI, maternal, obesity, overweight, observational and cohort studies, and randomized controlled trials. A total of 2,830 articles were located. However, an assessment of these articles revealed that only eleven of them fit the criteria. Further research was carried out through exploring the South Wales University “Find it” global article search, which contributed one more article. A total of twelve research studies were finally considered for review to answer the research question. The PRISMA 2009, Hill and Spittle house, 2004 critical appraisal approach, and the Critical Appraisal Skills Program (CASP, 2013) were primarily used to critically evaluate the articles and reach an evidence statement (Figure 1) [33-35,56,61].
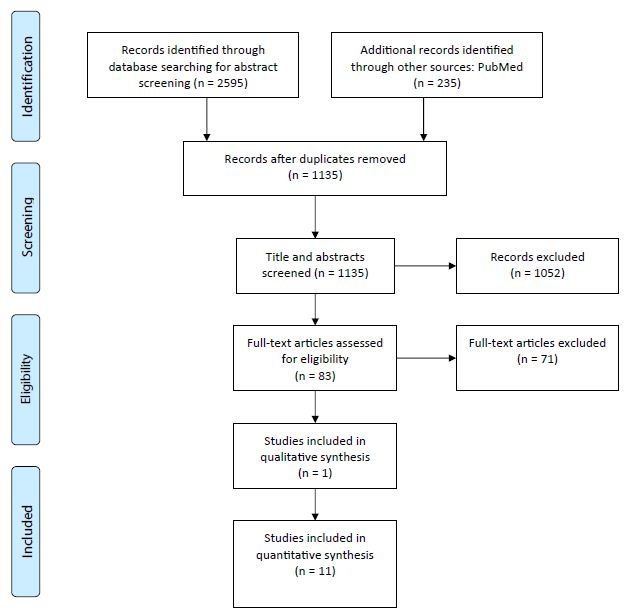
Figure 1: PRISMA 2009 Flow Diagram
Results
The review considered maternal obesity/overweight as independent variables (defined as Prepregnancy or postpartum BMI) and BF rate as the dependent outcome variable. The analysis included assessing whether the studies addressed potential confounding variables that interfere in the relationship between obesity/overweight and BF rates. Besides, the PRISMA 2009 was utilized with the summary as follows: In 2006, Oddy et al. investigated the association of maternal Prepregnancy overweight and obesity with BF duration [36]. This prospective study, conducted in Western Australia, covered 1803 live-born infants and their mothers. Results indicated that, after adjusting for socioeconomic, demographic, biological, and medical factors of mothers and infants, Prepregnancy obesity and overweight had no relationship to the initiation [36]. However, they showed a significant effect on reducing BF at any period before six months; obese mothers were more likely to stop BF at two months Odds ratio (OR 1.89 [95%] CI: 1.45, 2.47) compared to normal-weight mothers (OR 1.76 [95%] CI: 1.35, 2.28) and for less than six months [36].
Mok et al., 2008 investigated the relationship between Prepregnancy BMI of obese mothers and BF practices concerning the initiation and continuation at three months postpartum. The study covered 1432 mothers at the Centre Hospitalier Universitaire de Poitiers, France, in 2005. Obesity was significantly associated with lower BF initiation and continuation rates at one month (p ≤ 0.0001) and three months (p ≤ 0.001). An interesting finding of this study points to the psychological factors that may affect BF. Women reported feeling uncomfortable to breastfeed in public at 3 months [37].
In a cohort study, Liu et al., 2010, investigated race as a contributing factor to the negative impact of maternal obesity on the prevalence of BF. The analysis examined the relationship between maternal obesity and BF initiation and duration among women in South Carolina. This is one of the few studies which explored the effects of race in detail. A random sample of 2,840 black and 3,517 white women was drawn from a population-based Pregnancy Risk Assessment Monitoring System (PRAMS) dataset, which included women who gave birth from 2000 to 2005 [38]. The study revealed that Prepregnancy weight of white women negatively affects BF, especially in morbidly obese mothers (OR 0.63, [95%] CI: 0.42, 0.94). The study also showed that, while black obese women did not initiate BF, obesity did not affect the duration of BF when BMI was continuously measured (adjusted hazard ratio 1.03, (95%) CI: 1.01, 1.04) [38].
The association between BF initiation and maternal Prepregnancy BMI was investigated in 2013 by Thompson et al. in Florida, US. This study used a large population-based sample amounting to 1,161,949 singleton mothers who gave birth between 2004-2009. Women reported Prepregnancy weight, height measurements, and initiation of BF in the instantaneous postpartum period. The results of the study indicated that, after adjustment for the confounding variables, including race (Hispanic and other races), obese mothers were less likely to initiate BF compared to normal-weight mothers (OR: 0.84 (95%) CI: 0.83, 0.85). However, this finding did not apply to overweight mothers [39].
A population-based cohort study investigated a large sample of 22131 women delivering in four hospitals in Ontario, Canada. The findings pointed to a negative impact of obesity on BF intention and initiation. This study recruited women who had full-term live births between 2008- 2010. Study results showed that obese mothers, constituting 21% of the study sample, were less likely to plan to BF. In contrast, overweight mothers (27.7% of the sample) were likely to practice BF as normal-weight mothers. Both obese and overweight mothers were less inclined to initiate BF in hospitals and upon discharge than mothers with normal weight [OR: 0.67(0.60-0.75), 0.68 (0.62-0.76)], respectively [40].
Several elements may contribute to the negative impact of maternal BMI on BF. Some of these are related to the mother’s body shape, which hinders the infant’s physical positioning or leads to mechanical failure during suckling at the nipple [36,41]. Psychosocial factors contribute to embarrassment related to body size or shape, thus interfering with BF, mainly when practiced in public. Other factors are associated with obtaining proper health education and counseling from health professionals [36,41-43].
In the US, a national cohort study conducted by Hauff et al., 2014 found that maternal BMI did not affect BF intention and initiation. However, the duration of “ever” BF and “any” BF, as defined by the authors of overweight and obese mothers, was negatively affected by psychosocial factors. Obese women have a 29% increased risk to stop “any” BF than normal-weight mothers (adjusted hazard ratio for the cessation of BF among obese mothers 1.29 (95%) CI: 1.09-1.53). However, this did not apply to overweight mothers [44]. This longitudinal study suggested that overweight and obese mothers, in contrast to normal-weight mothers, were less confident in their ability to practice BF amongst their infants then they had initially intended. Additionally, their BF continuation was adversely influenced by social networks, friends, and relatives who had a poor BF history [44].
Keely et al., 2015 conducted in depth semi-structured interviews with a group of 28 obese women living in Scotland. The participants were recruited between 2011-2013 and represented different ethnic groups and social classes in the study area. This qualitative study aimed to identify obstacles to BF and learn more about women’s views concerning BF practices and the support provided by family, community, and health services [45]. The findings indicated that obese mothers had intentions to BF for at least 16 weeks. However, several of them failed to continue beyond a few days of initiation [45]. The rest could not continue beyond 6-10 weeks. Challenges identified as contributing to this behavior included physical, social support, and psychological factors [45]. This study’s contributions to the literature could be outlined in three themes: a lack of privacy, the impact of birth complications, and low uptake of specialist BF support [45].
A longitudinal cohort study conducted by Verret-Chalifour et al., 2015 in Quebec-Canada on a sample of 6,592 pregnant women confirmed the negative impact of high Prepregnancy BMI on BF initiation [46]. Obese mothers had a 26% increased risk of non-initiation of BF as compared to normal-weight women (relative risk 1.26 [95%] CI: 1.08- 1.46) [46].
A study from 2018 found that the incidence of self-reported BF problems was comparable across weight status groups: normal-weight and overweight. “Not enough milk” was the principal reason for providing infant milk formula [47]. Overweight women were more likely than normal-weight women to agree that infant formula was as good as breast milk [47].
Several qualitative and quantitative studies from 2019 also confirm that overweight and obese women are less likely to practice BF, have more difficulty with BF, and are strongly influenced by psychosocial factors such as poor self-efficacy and fear of negative evaluation of others based on their weight. [48-50].
Conclusion
The research question under review showed a high prevalence of maternal obesity ranging between 10-25%. The formal studies were mostly cohort, prospective, and population-based, used relatively large samples, and adjusted for most of the potential confounders. Many of the studies were carried out in developed countries, limiting the generalizability of the evidence for public health practice in different settings [51]. The majority of the studies showed evidence of a negative impact of obesity on BF rates. These data strongly suggest that although obese women may experience some additional challenges with BF initiation mechanics, perhaps a more important consideration is their perception of the opinion of the critical others in their social environment. Therefore, to understand BF behavior among obese women, we should consider conducting more empirical studies that use well-established theories, including the theory of reasoned action (TRA) [52]. TRA is a theory that is well manifested in the literature of understanding and predicting human behavior. TRA proposes that ‘intention’ is the main predictor of the behavior and response as a function of two variables: attitudes held towards behaviors, practices, ethics, and subjective norms [52]. TRA concedes humans need to be part of society. Consequently, TRA proposes that those who created an individual’s society and perceived as necessary to the individual, such as family members and friends, significantly influence an individual’s intention to perform a behavior [48]. About the reviewed literature results, it is expected that TRA will provide an excellent theoretical background to study further the effect of subjective norms on obese women’s intention to BF and to continue BF.
The reviewed literature also suggested a difference in intention and duration of obese women based on race. This difference raises the point to the need to explore the effect of culture – individuals’ collective perception of social norms, roles, and values in their environment which controls what behavior is desirable or should be circumvented to shape the intention of an obese woman towards BF [53,54]. For example, Hofstede’s studies on cultural dimensions have described two main groups for cultural differences; individualism and collectivism. Hofstede’s cultural index described individualism as independence from paying more consideration to one’s rights over one’s duties and social interaction [53,54]. On the other hand, collectivism was described as a higher degree of harmony between individuals and groups [55]. Thus, it is expected that the type of culture that obese BF women belong to will determine the degree to which they perceive others’ opinions to be essential and how it will shape their intention to breastfeed and continue for a set duration.
Another concern is a deficit of information among mothers about the importance of BF in both infants’ and mothers’ health. Given the high rates of maternal obesity and low prevalence of BF across the world, physicians and other health care providers are in an ideal position to educate patients- particularly those overweight and obese mothers or mothers-to-be on the benefits of BF and exploring with them their perceptions of factors that may be interfering with their intentions or willingness to breastfeed their infants. Attention to this issue can significantly improve the health of the people in our state for years to come.
Acknowledgments
The authors would like to acknowledge Mohammed Bin Rashid School of Government, Dubai, UAE, and the Alliance for Health Policy and Systems Research at the World Health Organization for financial support as part of the Knowledge to Policy (K2P) Center Mentorship Program [BIRD Project].
References
- State Briefs [Internet]. The State of Obesity. [Cited 2019 Jun 24].
- WHO | Mean Body Mass Index (BMI) [Internet]. WHO. [Cited 2019 Jul 2].
- Kelly T, Yang W, Chen CS, Reynolds K, He J (2008) Global burden of obesity in 2005 and projections to 2030. Int J Obes 2005 32: 1431-1437. [crossref]
- Puhl RM, Heuer CA (2009) The stigma of obesity: a review and update. Obes Silver Spring Md 17: 941-964. [crossref]
- National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants – The Lancet [Internet]. [Cited 2019 Jul 2].
- WHO | obesity among women [Internet]. WHO. [Cited 2019 Jul 2].
- Cohen DA (2008) Obesity and the Built Environment: Changes in Environmental Cues Cause Energy Imbalances. Int J Obes 32: S137-142. [crossref]
- Hu FB, Li TY, Colditz GA, Willett WC, Manson JE (2003) Television Watching and Other Sedentary Behaviors in Relation to Risk of Obesity and Type 2 Diabetes Mellitus in Women. JAMA 289: 1785-1791. [crossref]
- Collective GB, UNICEF. Nurturing the health and wealth of nations: the investment case for breastfeeding. World Health Organization. 2017 Jul. [Internet]. [cited 2019 Jul 2].
- Moore ML (2001) Current Research Continues to Support Breastfeeding Benefits. J Perinat Educ 10: 38-41. [crossref]
- Allen J, Hector D (2005) Benefits of breastfeeding. New South Wales Public Health Bull 16: 42-46. [crossref]
- Heinig MJ (2001) Host Defense Benefits of Breastfeeding for the Infant: Effect of Breastfeeding Duration and Exclusivity. Pediatr Clin North Am 48: 105-123. [crossref]
- Yngve A, Sjöström M (2001) Breastfeeding determinants and a suggested framework for action in Europe. Public Health Nutr 4: 729-739. [crossref]
- Amir LH, Donath S (2007) A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy Childbirth 7: 9. [crossref]
- Krause KM, Lovelady CA, Østbye T (2011) Predictors of breastfeeding in overweight and obese women: data from Active Mothers Postpartum (AMP). Matern Child Health J 15: 367-375. [crossref]
- Leonard SA, Labiner-Wolfe J, Geraghty SR, Rasmussen KM (2011) Associations between high prepregnancy body mass index, breastmilk expression, and breastmilk production and feeding. Am J Clin Nutr 93: 556-563. [crossref]
- Li R, Zhao Z, Mokdad A, Barker L, Grummer-Strawn L (2003) Prevalence of breastfeeding in the United States: the 2001 National Immunization Survey. Pediatrics 111: 1198-1201. [crossref]
- Turcksin R, Bel S, Galjaard S, Devlieger R (2014) Maternal obesity and breastfeeding intention, initiation, intensity and duration: a systematic review. Matern Child Nutr 10: 166-183. [crossref]
- Wojcicki JM (2011) Maternal prepregnancy body mass index and initiation and duration of breastfeeding: a review of the literature. J Womens Health 2002 20: 341-347. [crossref]
- World Health Organization. Obesity and Overweight: Key Facts. 2018 Feb.
- Center for Disease Control and Prevention. Obesity and Overweight. 2017 Aug. Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion.
- Nahhas R (2017) Obesity a major health problem in Jordan. The Arab Weekly.
- Buckingham C, Sauter MB (2018) The World’s Most Overweight Countries. 2018 Jul; 24/7 Wall St Journal.
- Lancet Journal (2016) Breastfeeding Series, Lancet 387: 404-504.
- Debes AK, Kohli A, Walker N, Edmond K, Mullany LC (2013) Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. BMC Public Health 13: S19. [crossref]
- Issaka AI, Agho KE, Renzaho AM (2017) Prevalence of key breastfeeding indicators in 29 sub-Saharan African countries: a meta-analysis of demographic and health surveys (2010-2015). BMJ Open 7: e014145.
- Department of Statistics (DOS) and ICF. Jordan Population and Family and Health Survey 2017-18. 2019 March. Amman, Jordan, and Rockville, Maryland, USA: DOS and ICF.
- Khasawneh W, Khasawneh AA (2017) Predictors and barriers to breastfeeding in north of Jordan: could we do better?. Int Breastfeed J 12: 49.
- Khassawneh M, Khader Y, Amarin Z, Alkafajei A (2006) Knowledge, attitude and practice of breastfeeding in the north of Jordan: a cross-sectional study. Int Breastfeed J 1: 1-17. [crossref]
- Dasoqi KA, Safadi R, Badran E, Basha AS, Jordan S, et al. (2018) Initiation and continuation of breastfeeding among Jordanian first-time mothers: a prospective cohort study. Int J Womens Health 10: 571-577. [crossref]
- Abuidhail J (2014) Colostrum and complementary feeding practices among Jordanian women. MCN Am J Matern Child Nurs 39: 246-252. [crossref]
- Abu Shosha G (2015) The influence of infants’ characteristics on breastfeeding attitudes among Jordanian mothers. Open J Nurs 5: 295-302.
- Loi UR, Gemzell-Danielsson K, Faxelid E, Klingberg-Allvin M (2015) Health care providers’ perceptions of and attitudes towards induced abortions in sub-Saharan Africa and Southeast Asia: a systematic literature review of qualitative and quantitative data. BMC public health 15: 139. [crossref]
- Burls A (2014) What is critical appraisal? Hayward Medical Communications.
- Young JM, Solomon MJ (2009) How to critically appraise an article. Nat Clin Pract Gastroenterol Hepatol 6: 82-91.
- Oddy WH, Li J, Landsborough L, Kendall GE, Henderson S, et al. (2006) The association of maternal overweight and obesity with breastfeeding duration. J Pediatr 149: 185-191.
- Mok E, Multon C, Piguel L, Barroso E, Goua V, et al. (2008) Decreased full breastfeeding, altered practices, perceptions, and infant weight change of prepregnant obese women: a need for extra support. Pediatrics 121: e1319-1324. [crossref]
- Liu J, Smith MG, Dobre MA, Ferguson JE (2010) Maternal obesity and breastfeeding practices among white and black women. Obes Silver Spring Md 18: 175-182. [crossref]
- Thompson LA, Zhang S, Black E, Das R, Ryngaert M, et al. (2013) The association of maternal prepregnancy body mass index with breastfeeding initiation. Matern Child Health J 17: 1842-1851.
- Visram H, Finkelstein SA, Feig D, Walker M, Yasseen A, et al. (2013) Breastfeeding intention and early postpartum practices among overweight and obese women in Ontario: a selective population-based cohort study. J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet 26: 611-615. [crossref]
- Rasmussen KM, Dieterich CM, Zelek ST, Altabet JD, Kjolhede CL (2011) Interventions to increase the duration of breastfeeding in obese mothers: the Bassett Improving Breastfeeding Study. Breastfeed Med Off J Acad Breastfeed Med 6: 69-75. [crossref]
- Ahluwalia IB, Li R, Morrow B (2012) Breastfeeding practices: does method of delivery matter? Matern Child Health J 16: 231-237.
- Jarlenski M, McManus J, Diener-West M, Schwarz EB, Yeung E, et al. (2014) Association between support from a health professional and breastfeeding knowledge and practices among obese women: evidence from the Infant Practices Study II. Womens Health Issues Off Publ Jacobs Inst Womens Health 24: 641-648.
- Hauff LE, Leonard SA, Rasmussen KM (2014) Associations of maternal obesity and psychosocial factors with breastfeeding intention, initiation, and duration. Am J Clin Nutr 99: 524-534. [crossref]
- Keely A, Lawton J, Swanson V, Denison FC (2015) Barriers to breastfeeding in obese women: A qualitative exploration. Midwifery 31: 532-539.
- Verret-Chalifour J, Giguère Y, Forest JC, Croteau J, Zhang P, et al. (2015) Breastfeeding initiation: impact of obesity in a large Canadian perinatal cohort study. Plos One 10: e0117512. [crossref]
- Mallan KM, Daniels LA, Byrne R, de Jersey SJ (2018) Comparing barriers to breastfeeding success in the first month for non-overweight and overweight women. BMC Pregnancy Childbirth 18: 461.
- Chang YS, Glaria AA, Davie P, Beake S, Bick D (2019) Breastfeeding experiences and support for women who are overweight or obese: A mixed methods systematic review. Matern Child Nutr
- Huang Y, Ouyang YQ, Redding SR (2019) Maternal Prepregnancy Body Mass Index, Gestational Weight Gain, and Cessation of Breastfeeding: A Systematic Review and Meta-Analysis. Breastfeed Med Off J Acad Breastfeed Med 14: 366-374. [crossref]
- Claesson I-M, Myrgård M, Wallberg M, Blomberg M (2019) Pregnant women’s intention to breastfeed; their estimated extent and duration of the forthcoming breastfeeding in relation to the actual breastfeeding in the first year postpartum-A Swedish cohort study. Midwifery 76: 102-109. [crossref]
- Yost J, Dobbins M, Traynor R, DeCorby K, Workentine S, et al. (2014) Tools to support evidence-informed public health decision making. BMC Public Health 14: 728.
- Fishbein M, Ajzen I (1976) Misconceptions about the Fishbein model: Reflections on a study by Songer-Nocks. Journal of Experimental Social Psychology 12: 579-584.
- Hofstede G (1984) Cultural dimensions in management and planning. Asia Pacific journal of management 1: 81-99.
- Qasem W, Fenton T, Friel J (2015) Age of introduction of first complementary feeding for infants: a systematic review. BMC pediatrics 15: 107. [crossref]
- Rahman MH, Moonesar IA, Hossain MM, Islam MZ (2018) Influence of organizational culture on knowledge transfer: Evidence from the Government of Dubai. Journal of Public Affairs 18: e1696.
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6: e1000097. [crossref]
- OECD (2009) Breastfeeding rates. OECD Family database. OECD – Social Policy Division – Directorate of Employment, Labour and Social Affairs.
- Nukpezah RN, Nuvor SV, Ninnoni J (2018) Knowledge and practice of exclusive breastfeeding among mothers in the tamale metropolis of Ghana. Reprod Health 15: 140. [crossref]
- Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, et al. (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371: 243-260. [crossref]
- Al Ketbi MI, Al Noman S, Al Ali A, Darwish E, Al Fahim M, et al. (2018) Knowledge, attitudes, and practices of breastfeeding among women visiting primary healthcare clinics on the island of Abu Dhabi, United Arab Emirates. Int Breastfeed J 13: 26. [crossref]
- Fadlallah R, El-Harakeh A, Bou-Karroum L, Lotfi T, El-Jardali F, et al. (2019) A common framework of steps and criteria for prioritizing topics for evidence syntheses: a systematic review. Journal of Clinical Epidemiology 120: 67-85. [crossref]