Abstract
We present an immunocompromised case of colon cancer who received a compound of tegafur and uracil as postoperative adjuvant chemotherapy. However, massive bloody stool passage was found and endoscopy revealed hemorrhagic erosions and ulcers at the ileum, which also caused partial obstruction of proximal small bowel. As persistent massive bleeding, segmental bowel resection was performed and the pathology of the resected lesion confirmed cytomegalovirus ileitis. Meanwhile, the polymerase chain reactions for cytomegalovirus DNA in the stool and peripheral blood samples were both positive. After surgical intervention, however, the intestinal bleeding still persisted and was stopped soon by ganciclovir therapy. In conclusion, intestinal bleeding due to cytomegalovirus ileitis may not be easily controlled without appropriate antiviral therapy. The polymerase chain reactions may be helpful in the earlier detection of cytomegalovirus intestinal disease and provide early initiation of pre-emptive therapy before the histopathological diagnosis is made.
Key words
cytomegalovirus, immunocompromised patients, ileitis
Introduction
Cytomegalovirus (CMV) is a virus that belongs to the family of Herpesviridae and usually causes an asymptomatic infection or produces mild flulike symptoms. Afterward, it remains latent throughout life and may reactivate in the immunocompromised status, thus causing a serious disease with significant morbidity and mortality of the patients [1]. CMV infection can affect any field of the gastrointestinal tract. The most common affected areas are the colon and the rectum, whereas other locations such as the duodenum and ileum are rarely reported [2-4]. Clinical symptoms of CMV ileitis include fever, abdominal pain, anorexia, nausea, vomiting, diffuse abdominal pain, lower abdominal pain, diarrhea, hematochezia or melena [2-4]. Herein we reported a rare case of CMV ileitis in a colon cancer patient presenting with partial small intestine obstruction and massive intestinal bleeding.
Case Report
This 75-year-old man had history of diabetes, gout and chronic hepatitis B virus infection. He was diagnosed with colon cancer and received laparoscopic radical right-sided hemicolectomy and subsequent adjuvant chemotherapy with tegafur/uracil (UFUR) 2 months prior to the admission. He suffered from nausea and vomiting with watery diarrhea since July 23, 2015. The laboratory data showed leukocytosis and the computed tomography (CT) of the abdomen showed segmental small bowel swelling at distal ileum (Figure 1A), causing partial obstruction of the proximal small bowel (Figure 1B). Then, he was admitted to the intensive care unit due to septic shock with acute respiratory failure. However, intermittent bloody stool passage was found. Colonoscopy through the right-sided colostomy showed diffuse hemorrhagic erosions and ulcers at distal ileum (Figure 1C). Thereafter, massive lower gastrointestinal bleeding persisted, thus requiring surgical intervention. Enterolysis and segmental bowel resection with end ileostomy were performed on August 17, 2015. Meanwhile, the polymerase chain reactions (PCRs) for CMV DNA in the stool and peripheral blood sample were both positive. The pathology of the biopsied ileum lesion confirmed CMV ileitis with evidence of some scattered stromal or endothelial cells with eosinophilic nuclear inclusion, which were highlighted by anti-CMV immunostain. Nonetheless, small bowel bleeding persisted even after surgery. Therefore, ganciclovir therapy was initiated and stopped the bleeding soon. Then the patient reached successful weaning from mechanical ventilation and he was uneventfully discharged.
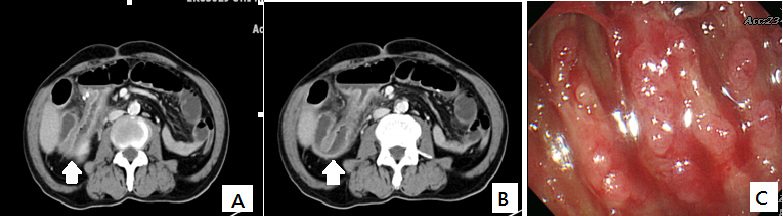
Figure 1. The CT of the abdomen shows segmental small bowel swelling at distal ileum till anastomosis (arrow, A), causing proximal small bowel partial obstruction (arrow, B). Colonoscopy through the right-sided colostomy reveals diffuse hemorrhagic erosions and ulcers at the ileum (C).
Discussion
CMV enteritis with lower gastrointestinal (GI) haemorrhage is a rare presentation. As CMV infection in immunocompromised patients can be lethal, it is important to diagnose and initiate early treatment. In systemic CMV infections, ulceration of the GI tract is common, which could be a primary infection, a superimposed infection, reactivation of latent infection or re-infection with a new virus (1). CMV ileitis is rarely reported in the literature, but could still occur in the immunocompetent patients [2-4]. However, even in an immmunocompromised patient like our presented patient with colon cancer, CMV ileitis bleeding is usually not considered in the earlier course of the GI bleeding disease. Most gastrointestinal CMV infections respond well to ganciclovir treatment. Therefore, the patient should be offered an antiviral treatment as soon as possible. Early diagnosis of suspected CMV infection in immunosuppressed patients with gastrointestinal symptoms is of the utmost importance. Delayed management of CMV ileitis might cause stenosis of the ileum [4] and massive lower gastrointestinal bleeding [5, 6], just like our case; or could also result in small bowel perforation [7]. Nonetheless, CMV ileitis in an immunocompetent patient with mild symptom of epigastric pain may spontaneously recover without antiviral therapy [2].
Repeat endoscopy may be considered if previous study did not meet a concluding gastrointestinal CMV disease. The ileum ulcer is difficult to approach by endoscopy. In the current patient, we could easily assess the lesion site through the right-sided colostomy but endoscopic biopsy was not performed during bleeding episode. CMV-infected hemorrhagic ileitis was diagnosed by subsequent surgical biopsy and thereby antiviral therapy was rather delayed. In this scenario, we recommend pre-emptive antiviral therapy based on the positive results for stool and/or blood CMV-PCRs.
Authorship
Hui-Chun Chao contributed to acquisition of data and drafting the article. Khee-Siang Chan contributed to the patient care and analysis and interpretation of data. Wen-Liang Yu contributed to conception, design and critical revision of the article. All authors approved the final version to be published and agreed for all aspects of the work related.
Conflict of interests
We declare no funding and no conflict of interests. The above study has been granted exemption from review by the Institutional Review Board of Chi-Mei Medical Center (application no.10410-E02).
References
- Ljungman P, Griffiths P, Paya C (2002) Definitions of cytomegalovirus infection and disease in transplant recipients. Clin Infect Dis 34: 1094-1097. [crossref]
- Ryu KH, Yi SY (2006) Cytomegalovirus ileitis in an immunocompetent elderly adult. World J Gastroenterol 12: 5084-5086. [crossref]
- Varma V, Perera MT, Olliff S, Taniere P, Isaac J, Mirza DF (2011) Cytomegalovirus ileitis causing massive gastrointestinal haemorrhage in a patient following hepatic resection. Tropical Gastroenterology 32:145-7.
- Tejedor Cerdeña MA, Velasco Guardado A, Fernández Prodomingo A, Concepción Piñero Pérez MC, Calderón R, et al. (2011) Cytomegalovirus ileitis in an immunocompetent patient. Rev Esp Enferm Dig 103: 154-156. [crossref]
- Meza AD, Bin-Sagheer S, Zuckerman MJ, Morales CA, Verghese A (1994) Ileal perforation due to cytomegalovirus infection. J Natl Med Assoc 86: 145-148. [crossref]
- Lai IR, Chen KM, Shun CT, Chen MY (1996) Cytomegalovirus enteritis causing massive bleeding in a patient with AIDS. Hepatogastroenterology 43: 987-991. [crossref]
- Vilaichone RK, Mahachai V, Eiam-Ong S, Kullavanuaya P, Wisedopas N, et al. (2001) Necrotizing ileitis caused by cytomegalovirus in patient with systemic lupus erythematosus: case report. J Med Assoc Thai 84 Suppl 1: S469-473. [crossref]