Introduction
Nationally and internationally, maternal mortality is an important indicator of the quality of a nation’s healthcare [1]. Recent statistics reported by the Centers for Disease Control and Prevention (CDC) indicates an increase in the pregnancy-related maternal mortality ratio (MMR) to 17.0 deaths per 100,000 live births from 2011–2013 [2], while in Europe and maternal death rates are declining [3,4]. When analyzing the demographics of maternal deaths in the U.S., it appears pregnancies in rural environments are more at risk, with some maternal mortality rates in rural areas as high as 28.7 deaths per 100,000 live births [5]. A study by Kozhimannil and colleagues [6] demonstrated a rise in the maternal mortality and morbidity of both rural and urban areas, but rural mothers had a 9% greater chance of an adverse outcome compared to the urban mothers. The WHO has identified several factors that account for 75% of all maternal deaths: severe bleeding and infections after childbirth, pre-eclampsia and eclampsia, complications from delivery, and unsafe abortion [7]. The majority of these conditions could be prevented if recognized and treated by a skilled medical professional and if birth takes place in a sanitary place early enough (e.g. hospital), which can be difficult if the patient lives in an area with a shortage of skilled healthcare providers or a long distance from these professionals, as is often the case in rural settings. The purpose of this article is to examine the differences in maternal death rates between rural and urban Illinois stratified by urbanization level and race/ethnicity from 2007 to 2016.
Methods
Maternal death rates per 100,000 women ages 15 through 54 were obtained from the CDC Wonder website for years 2007 to 2016. This age range was chosen to include a larger sample size who are still capable of child-bearing and whose cause of death was within the pregnancy categories of ICD-10 (O00 to O99). This data was further stratified into six urbanization categories defined by the Office of Management and Budget and National Center for Health Statistics: large central metro, large fringe metro, medium metro, small metro, micropolitan, and non-core. A literature search using PRISMA guidelines was conducted using the term “maternal mortality” and keywords “community” and/or “neighborhood.” Studies were limited to those written in English. Maternal death rates per 100,000 women ages 15 through 54 for the various subgroups were calculated using the CDC Wonder website, and statistical comparison of rates was done using methods described by Dever [8].
Results
Maternal death rates were first analyzed by urbanization categories for all races for the U.S. compared to Illinois (Graph 1). The only statistically significant difference was found in the large fringe metro category with Illinois having a significantly lower maternal death rate than the U.S. Other than small metro, all other urbanization categories had lower maternal death rates than the U.S. When these urbanization categories were broken down into racial/ethnic subgroups, White mothers in both Illinois and the U.S. as a whole were found to have statistically significant higher maternal death rates in the micropolitan and non-core categories (rural) when compared to the large central metro category. The Illinois white non-core rate was at least twice that of the four most urban areas. Maternal deaths for African American mothers in Illinois were too low to calculate a valid rate for rural areas, but U.S. African American maternal deaths are on average about 2.5 times than that of the U.S. Whites.
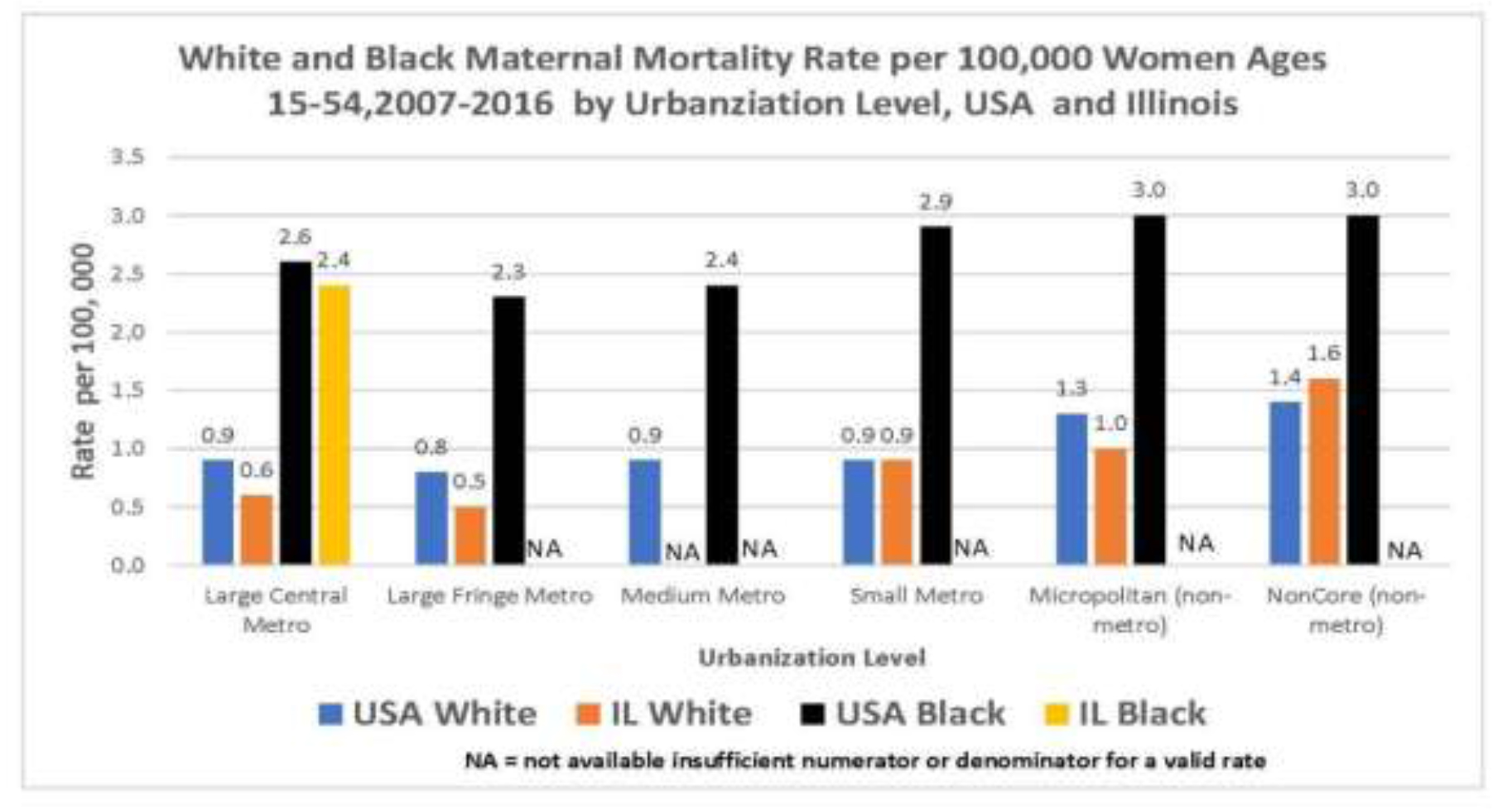
Graph 1
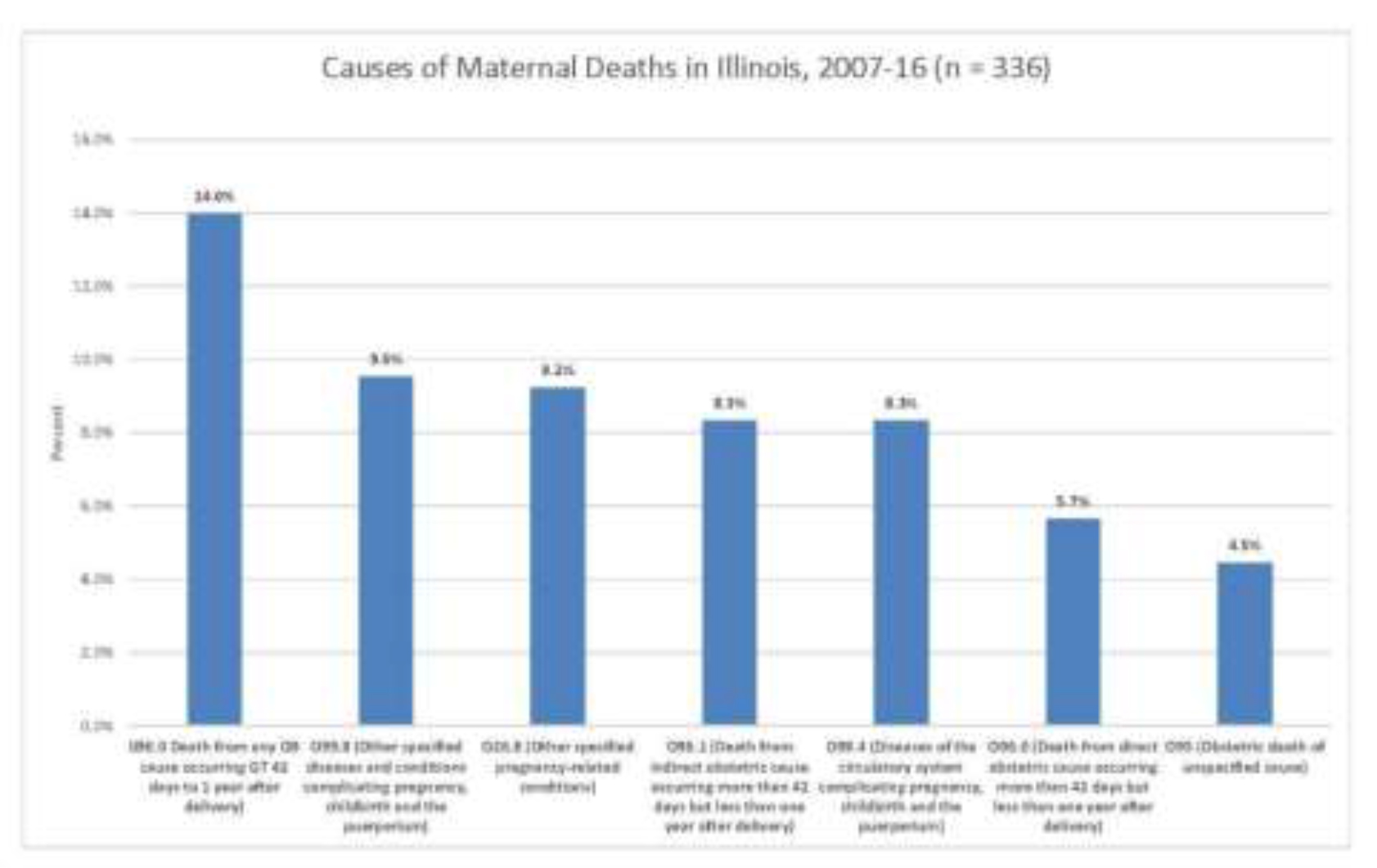
A gradual increase in maternal death rates within both Hispanics and non-Hispanics was observed as urbanization decreased, as the area became more rural (Graph 2). When comparing the large central metro U.S. non-Hispanic mothers to those in non-core areas, the more rural mothers had a statistically significant higher maternal death rate. Regarding the causes of maternal death according to ICD-10 codes. Any obstetrical complication from 42 days to a year postpartum (O90.0) was the most common coded caused of death at 14% (Graph 3). Overall about 28% of maternal deaths, both indirectly and directly related to an obstetrical cause, occur greater than 42 days but less than a year postpartum.
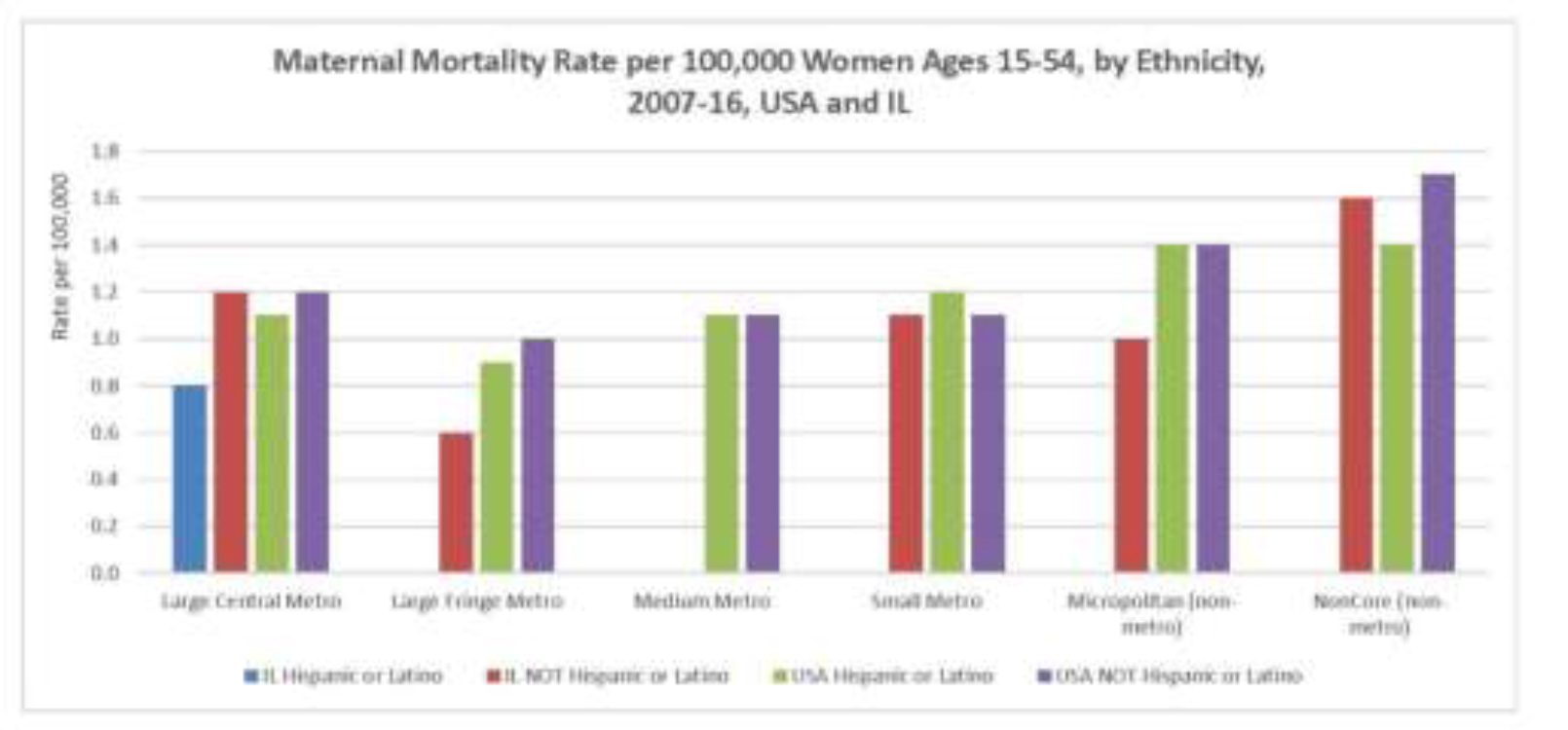
Graph 2
Graph 3
Discussion
White mothers residing in rural areas have higher maternal death rates when compared to all other mothers. These maternal deaths negatively impact the health and future outcomes of the infants left motherless in addition to financially impacting the families due to medical costs. About one-third of maternal deaths occur 42 days postpartum; literature suggests these deaths may be due to life-threatening bleeding and infections, blood pressure elevations, complications from childbirth, and unsafe abortions [7]. Kozhimannil and colleagues [9] attribute the patterns seen in rural areas to the loss of obstetrical care in rural settings, requiring mothers to travel in order to safely deliver their babies. Future studies should focus on determining the specific clinical causes of maternal death in rural areas in order to develop interventions to reduce and prevent maternal death. The limitations within this study lie partially in the dataset from the CDC. The data assumes the causes of maternal death are correctly coded on the death certificate; incorrect coding would alter the death rate from its true value. Maternal mortality rates would have been a more precise measure as it uses the number of women who gave birth as the denominator rather than the number of women in that specific subgroup. Some data was limited due to low population numbers in different subgroups; maternal death rates for Hispanic mothers in Illinois could only be calculated in the large central metro area as the numbers were too low in the less urban categories. A future study should aim to investigate the causes of the very elevated Black maternal death rate in Illinois as well as the U.S. Other studies may investigate maternal death patterns according to age, education level, access to pre- and post-natal care, and the experience of the delivering provider in those areas. These findings may help stimulate improvements where shortfalls lie in order to provide the best care to mothers as possible.
In conclusion, this study shows substantially elevated maternal death rates for mothers residing in rural areas relative to urban areas and serves as basis to advocate for systematic changes in those areas whose mothers are at the highest risk.
References
- MacDorman MF, Declercq E, Cabral H, Morton C (2016) Recent increases in the U.S. maternal mortality rate: Disentangling trends from measurement issues. Obstet Gynecol 128: 447–455. [crossref]
- Creanga AA, Syverson C, Seed K, Callaghan WM (2017) Pregnancy-related mortality in the united states, 2011–2013. Obstet Gynecol 130: 366–373. [crossref]
- MacDorman MF, Declercq E, Thoma ME (2017) Trends in maternal mortality by sociodemographic characteristics and cause of death in 27 states and the District of Columbia. Obstet Gynecol 129: 811–818. [crossref]
- United nations millennium development goals. http://www.un.org.proxy.cc.uic.edu/millenniumgoals/. Accessed Mar 29, 2018.
- Meyer E, Hennink M, Rochat R, et al. (2016) Working towards safe motherhood: Delays and barriers to prenatal care for women in rural and peri-urban areas of georgia. Matern Child Health J 20: 1358–1365. [crossref]
- Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK (2019) Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health Affairs 38: 2077–2085.
- WHO | maternal mortality. WHO Web site. http://www.who.int.proxy.cc.uic.edu/mediacentre/factsheets/fs348/en/. Accessed Mar 29, 2018.
- Dever GEA (1991) Community health analysis: Global awareness at the local level. 2nd ed. Gaithersburg, Md: Aspen Publishers.
- Kozhimannil KB, Hung P, Henning-Smith C, Casey MM, Prasad S (2018) Association between loss of hospital-based obstetric services and birth outcomes in rural counties in the united states. JAMA 319: 1239–1247.