Abstract
Objectives: According to the World Health Organization, out of the 5 million snakebites that occur annually, 2.7 million results in envenomation out of which between 81,000 and 139,000 leads to death. Since snakebite is more prevalent in developing countries, it is imperative that their healthcare professionals should be knowledgeable on snakes and snakebites to enable them provide the optimal management of snakebite. This study therefore assessed health professionals’ preparedness by way estimating their knowledge on snakes and snakebites three Tongu districts in Ghana.
Method: Using a de novo semi-structured questionnaire, data was collected from 186 health workers using a google form whose link was sent via WhatsApp platforms on their Android phones. Data was analyzed using Statistical Package for the Social Sciences (SPSS) Version 23. Results were presented in the form of tables and association between variables determined using the appropriate tools at a confidence interval of 95%.
Results: The study showed the respondents’ overall mean knowledge score on snakes was lower than their knowledge on snakebites [(8.31 ± 2.95/18 (46.2%)] vs. [13.78 ± 4.0/22 (62.6%)]. Respondents’ sex and a previous training on snakebite were significantly associated with their knowledge on snakes. Their knowledge on snakebites, was significant associated with type of health facility, professional grouping and training experience (p<0.05).
Conclusions: The knowledge of health workers in the Tongu districts in Ghana on snakes and snakebite was inadequate. Since previous in-service training was associated with respondents’ knowledge on snakes and snakebite, educational intervention is imperative, especially the nursing professionals who are frontline health workers.
Keywords
Knowledge, Healthcare providers, Snakes, Snakebites, Tongu districts
Introduction
According to the World Health Organization, (2010) when venomous snakes bite, it may not introduce venom into the tissue referred to as dry bite or non-venomous bite [1]. Dry bites may or may not be associated with local inflammation but do not present with systemic manifestations. Following a dry bite, the victim may present with presence of fang marks, local swelling, pain, redness and bleeding from the bite sites as well as reduced function of the affected body part resulting in anxiety [1]. The systemic effects produced after injection of large amount of venoms into the victim may cause haemotoxicity, neurotoxicity, nephrotoxicity, and cardiotoxicity.
In West Africa, most of the snakebites occur in the savanna regions with the saw-scaled or carpet viper (Echis ocellatus) being the snake most implicated in causing morbidity and mortality [2]. Other venomous snakes in the West African region include the spitting cobras (Naja nigricollis and N. katiensis), the puff adders (Bitis arietans) and (Dendroaspis spp) the manbas [1].
Although, the exact number of snakebites globally is not known, the WHO (2019a) estimated that about 5.4 million snake bites occur each year, resulting in 1.8 to 2.7 million cases of envenoming [3]. There are between 81 410 and 137 880 deaths and around three times as many amputations and other permanent disabilities each year. Most snake envenoming and fatalities occur in South Asia, Southeast Asia, and sub-Sahara Africa, with India reporting the most snakebite deaths of any country [4]. In sub-Saharan Africa, about a million people are estimated to be bitten by snake each year, with estimated 7000-20 000 deaths occurring with West Africa bearing an annual snakebite deaths of 3,557 to 5,450 [5]. Europe, Australia, and North America statistically have the lowest incidence of envenoming [5]. Many people who survive bites nevertheless suffer from permanent tissue damage caused by venom, leading to disability [6]. Despite the number of deaths caused by snakebite annually, it was until June, 2017 that the World Health Organization formally listed snakebite envenoming as a highest priority neglected tropical disease [7]. Worldwide, snakebites occur most frequently in the summer or dry seasons when snakes are active and humans are undertaking outdoors related activities such as agriculture [8].
Injuries, disabilities and deaths from snakebites are something that happens daily in most parts of the world particularly in the poorest communities. Knowledge in relation to the management of snakebite patients is therefore very important. If clinicians are unfamiliar with the different species of snakes and unable to distinguish between venomous and non-venomous snakes, as well as the characteristics of snakebites, it can be difficult to know how to respond appropriately in terms of management in the event of a bite. Therefore, it is important for healthcare providers especially those in rural environments to be well equipped in terms of knowledge on snakes and snakebites which is required for effective management of victims who get bitten by snakes hence the need for this study in three rurally situated Tongu districts of the Volta region of Ghana. Again, this study is important since a search on the internet found no publication on the level of knowledge of health care professionals on snakes and snake bites in Ghana although some studies were done in some African countries.
Methodology
Study Design
A descriptive cross-sectional design was used to conduct this study between May to July 2019 among health care providers comprising of medical doctors, pharmacists, pharmacy technicians, physician/medical assistants, nurses of various categories and midwives working in selected Community-Based Health Planning and Service (CHPS) compound, health centres and hospitals.
Study Location
The study was undertaken in selected health facilities across the three neighbouring districts in the Volta region of Ghana namely South Tongu, North Tongu and Central Tongu. The selected health facilities include the Sogakope district and Comboni hospitals, Kpotame, Dabala, and Adutor health centres, Sasekope and Agbakope CHPS compounds from the South Tongu district; the Battor Catholic hospital and Volo health centre in the North Tongu district; the Adidome hospital, Mafi-Kumase and Mafi Dove health centres in the Central Tongu district. The Tongu districts are located in the South eastern part of the Ghana and are mainly inhabited by people of the Ewe tribe speaking the Tongu dialect. The total population of these districts in the 2010 population census was 237, 138 with agriculture as the main occupation of the people [9].
Sample Size
The sample size for this study was calculated using the Cochran formula, 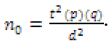
Where t = value for selected alpha level of 0.025 in each tail = 1.96, d = acceptable margin of error for proportion being estimated = 0.05, p is the estimated proportion of an attribute that is present in the population, which is considered as 0.5 and q is 1-p. The knowledge of health care providers about snakes, snakebites and the management of snakebites was estimated at 50%.
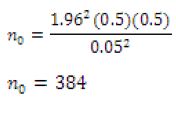
Since 384 exceeds the 5% (537 x 0.05 = 26.9) of the eligible study population of 537 having excluded the 20 who took part in the piloting, there was the need to use the Cochran correction formula to get adjusted sample size ![]()
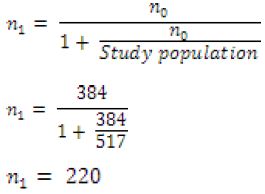
Assuming a response rate of 90%, the actual sample size = ![]() = 244
= 244
The total response received was 186 giving a response rate of 76.2% (186/244*100).
Sampling Technique
A total of 186 respondents across the three Tongu districts participated in the study. The selection of respondents for this study was done through the use of both census and convenience sampling techniques. Effort was made to take a census sample of all the pharmacists (5), physician/medical assistants (26), medical doctors (17), and pharmacy technicians (6) because of their small numbers in the selected health facilities. However, for the nurses and midwives who were about 483, convenience sampling technique was applied to select the respondents.
Collection Instrument and Technique
Data for the study was collected in the period between May and June, 2019 through the use of a self-administered semi-structured questionnaire designed using google form. Section one of the questionnaire consists of eight questions on sociodemographic characteristics of the respondents; section two, eighteen questions assessing the knowledge on snakes and section three, sixteen questions assessing the knowledge on snakebites. The questionnaire development was guided by the WHO (2010) publication on Guidelines for the prevention and clinical management of snakebites in Africa. The questionnaire was administered through the WhatsApp accounts of the respondents using the link https://forms.gle/iV5NtKzdjbg5LTSc9 which they submitted online after the completion of the form.
Data Analysis
Microsoft Excel spreadsheet was generated from the google form. The data was processed and cleaned after which analysis was done using Statistical Package for the Social Sciences (SPSS) Version 23. Descriptive data were presented as frequencies, percentages and means in tables. Association between variables was determined using a confidence interval of 95%. Significance was assumed when p<0.05.
Data Measurement
The level of knowledge of respondents on snakes and snakebite were assessed by scoring the answers provided by the respondents which are compared with literature sources. A score of 1 mark was awarded for any correctly answered question with options to choose from. Besides the wrong answer, an ‘I don’t know’ option also attracts no mark. For open-ended questions that requires the respondent to provide a specified number of answers, each correct answer scores 1 mark, hence the maximum total score for a question requiring three answers is 3. The total scores for the knowledge on snakes and snakebites of the respondents were 18 and 22 respectively.
Ethical Consideration
Permission was sought from the District Health Directorates, Medical Superintendents and the Administrators of the South Tongu, North Tongu and Central Tongu hospitals before the data was collected. Study tool used for the study was approved by the Ethic Committee of the School of Medicine and Health Sciences of the University for Development Studies. Consent was obtained once the respondents agree to take part in the study, completed the form and submitted it. The preamble on the questionnaire explained the purpose of the research and stating clearly that submitting the form after completion is indicative of giving consent. They were also assured of confidentiality of all the information they were to provide.
Results
Socio-Demographic Characteristics of Respondents
Table 1 shows the socio-demographic characteristics of respondents in this study. Majority, 95 (51.1%) were males, and were within the age group 30-39 years, 98 (52.7%). Most respondents, 87 (46.8%) were from the South Tongu district, followed by the North Tongu, 54 (29.0%) with Central Tongu having the least number of respondents, 45 (24.2%). For the number of years of practice, majority, 112 (60.2%) had served for less than five years with the least number, 3 (1.6%) working for more than ten years. Majority of respondents, 146 (78.5%) work at various hospitals, while those from health centres and CHPS zones were 25 (13.4%) and 15 (8.1%) respectively. Registered General Nurses, 80 (43.3%) formed the largest number of health professional group with the pharmacists, 4 (2.2%) being the least.
Table 1: Socio-demographic characteristics of respondents.
| Variable | Subgroup | Frequency | Percentage (%) |
| Sex | Male | 95 | 51.1 |
| Female | 91 | 48.9 | |
| Age (years) | 20-29 | 81 | 43.5 |
| 30-39 | 98 | 52.7 | |
| >39 | 7 | 3.7 | |
| District | South Tongu | 87 | 46.8 |
| Central Tongu | 45 | 24.2 | |
| North Tongu | 54 | 29.0 | |
| Number of years of practice (years) | <5 | 112 | 60.2 |
| 5-10 | 71 | 38.2 | |
| >10 | 3 | 1.6 | |
| Level of health facility | CHPS compounds | 15 | 8.1 |
| Health Centre | 25 | 13.4 | |
| Hospital | 146 | 78.5 | |
| Profession category | Registered General Nurse | 80 | 43.0 |
| Enrolled/Community Nurse | 37 | 26.3 | |
| Midwife | 15 | 8.1 | |
| Medical Doctor | 14 | 7.5 | |
| Pharmacy Technician | 5 | 2.7 | |
| Pharmacist | 4 | 2.2 | |
| Physician/Medical assistant | 19 | 10.2 |
Knowledge of Respondents about Snakes
Table 2 shows knowledge of respondents on snakes. The top five best answered questions on the knowledge of respondents about snakes were; Snakes being reptiles (99.0%), Cobra being venomous (92.0%), not all snakes are venomous (85%), identification of Cobra (82.0%), Cobra being the snake that spit into the eyes of the perceived enemies and Puff adder being venomous (67.0%). Five questions about snakes which were most poorly scored were; Identification of Savanna egg eater (2.0%), identification of Boomslang (3.0%), identification of Africa beauty snake (4.0%), Savanna egg eater being nonvenomous (5.0%) and Africa beauty snake being partially venomous (10.0%). The overall average knowledge score of respondents about snakes was 8.31 ± 2.950/18 (46.2%).
Table 2: Knowledge of respondents on snakes.
| Question | Responses | Mean knowledge score | Percentage knowledge score | ||
| Correctness | Frequency | Percentage | |||
| What type of animals are snakes? (Reptiles) | Incorrect | 2 | 1.1 | 0.99 ± 0.103 | 99.0 |
| Correct | 184 | 98.9 | |||
| All snakes are carnivorous, i.e. feed on other animals. (Yes) | Incorrect | 78 | 41.9 | 0.58 ± 0.495 | 58.1 |
| Correct | 108 | 58.1 | |||
| All snakes are venomous, i.e. inject “toxins” or venom into a person after a bite? (No) | Incorrect | 28 | 15.1 | 0.85 ± 0.359 | 85.0 |
| Correct | 158 | 84.9 | |||
| All snakes have fangs in front of their mouth. (No) | Incorrect | 86 | 46.2 | 0.54 ± 0.500 | 54.0 |
| Correct | 100 | 53.8 | |||
| Snakes pick sounds using their ears? (No) | Incorrect | 133 | 71.5 | 0.28 ± 0.453 | 29.0 |
| Correct | 53 | 28.5 | |||
| Name of snake that spits venom towards the eyes’ enemies? (Cobra) | Incorrect | 62 | 33.3 | 0.67 ± 0.473 | 67.0 |
| Correct | 124 | 66.7 | |||
| Identify the snake A
{Boomslang/green tree snake) |
Incorrect | 181 | 97.3 | 0.03 ± 0.162 | 3.0 |
| Correct | 5 | 2.7 | |||
| Is snake A venomous, partially venomous (V) or nonvenomous (NV)? (NV) | Incorrect | 94 | 50.5 | 0.49 ± 0.501 | 50.0 |
| Correct | 92 | 49.5 | |||
| Identify snake B (Cobra)
|
Incorrect | 34 | 18.3 | 0.82 ± 0.388 | 82.0 |
| Correct | 152 | 81.7 | |||
| Is snake B venomous, partially venomous or nonvenomous? (V) | Incorrect | 15 | 8.1 | 0.92 ± 0.273 | 92.0 |
| Correct | 171 | 91.9 | |||
| Identify snake C (Python)
|
Incorrect | 76 | 40.9 | 0.59 ± 0.493 | 59.0 |
| Correct | 110 | 59.1 | |||
| Is snake C venomous, partially venomous or nonvenomous? (NV) | Incorrect | 114 | 61.3 | 0.39 ± 0.488 | 39.0 |
| Correct | 72 | 38.7 | |||
| Identify snake D (Savanna egg eater) | Incorrect | 183 | 98.4 | 0.02 ± 0.126 | 2.0 |
| Correct | 3 | 1.6 | |||
| Is snake D venomous, partially venomous or nonvenomous? (NV) | Incorrect | 176 | 94.6 | 0.05 ± 0.226 | 5.0 |
| Correct | 10 | 5.4 | |||
| Identify snake E (Puff adder) | Incorrect | 133 | 71.5 | 0.28 ± 0.453 | 29.0 |
| Correct | 53 | 28.5 | |||
| Is snake E venomous, partially venomous or nonvenomous? | Incorrect | 62 | 33.3 | 0.67 ± 0.473 | 67.0 |
| Correct | 124 | 66.7 | |||
| Identify snake F (Africa beauty snake) | Incorrect | 178 | 95.7 | 0.04 ± 0.203 | 4.0 |
| Correct | 8 | 4.3 | |||
| Is snake F venomous, partially venomous (PV) or nonvenomous? (PV) | Incorrect | 167 | 89.8 | 0.10 ± 0.304 | 10.0 |
| Correct | 19 | 10.2 | |||
| Overall mean score | 8.31 ± 2.950/18 | 46.2% | |||
Correct answers are in parenthesis ( ) at the end of the question.
Association between Socio-Demographic Characteristics and Knowledge on Snakes
Table 3 shows association between socio-demographic characteristics and knowledge on snakes. For knowledge of respondents about snakes, males significantly scored better than females (9.04 vs. 7.55; p < 0.001). Respondents working at the lowest part of the health system, the CHPS compound obtained the best scores (9.27), followed by those in the health centres (9.24) while respondents in hospitals scores the least of 8.05 but the differences were not significant. Respondents from the Central Tongu district obtained the best mean score (9.04) followed by North Tongu (8.67) and South Tongu recorded the lowest (7.17) but the differences were not significant. There was no significant association between area of profession and knowledge on snakes but pharmacists had the highest mean score (10.25) and the Registered General Nurses (RGNs) had the lowest mean score (7.80). The prescribers and pharmacy groups had a better knowledge mean scores of 9.67 and 9.27 respectively while the nurses and the midwives group scored 8.01 but there were no significant differences. Respondents who had training on snakebite management significantly scored better than those who did not received training (9.93 vs. 7.60; p < 0.0001). Respondents with more than 10 years of practice scored better with mean score of 12.50, followed by respondents with < 5years (8.48) and 5-10 years (7.93) in that order but there were no significant differences.
Table 3: Association between socio-demographic characteristics and knowledge on snakes.
| Variable | Sub group | Mean score ± standard deviation (SD) | p-value |
| Sex | Male | 9.04 ± 2.982 | < 0.001* |
| Female | 7.55 ± 2.730 | ||
| Level of health facility | CHPS compound | 9.27 ± 2.963 | 0.75 |
| Health centre | 9.24 ± 3.551 | ||
| Hospital | 8.05 ± 2.803 | ||
| District of health facility | South Tongu | 7.71 ± 2.753 | 0.27 |
| Central Tongu | 9.04 ± 3.398 | ||
| North Tongu | 8.67 ± 2.706 | ||
| Area of profession | RGN | 7.80 ± 2.528 | 0.35 |
| Pharmacist | 10.25 ± 4.924 | ||
| Medical officer | 9.64 ± 3.455 | ||
| Physician assistant | 9.00 ± 3.448 | ||
| CHN/ENa | 7.82 ± 2.855 | ||
| Pharmacy technician | 9.20 ± 3.114 | ||
| Registered midwife | 9.73 ± 2.890 | ||
| Professional groups | Nursing and midwifery group | 8.01 ± 2.726 | 0.30 |
| Prescriber group | 9.67 ± 3.755 | ||
| Pharmacy group | 9.27 ± 3.412 | ||
| Training | No training | 7.60 ± 2.600 | <0.001* |
| Received training | 9.93 ± 3.076 | ||
| Number of years of practice | <5 years | 8.48 ± 2.825 | 0.060 |
| 5-10 years | 7.93 ± 3.073 | ||
| >10 years | 12.50 ± 2.121 |
aCHN/EN – Community Health Nurse/Enrolled Nurse, * Statistically significant.
Knowledge of Respondents on Snakebite
The top five best answered questions on the knowledge of respondents about snakebite were; the local signs and symptoms of snakebite (93.0%), ways of preventing snakebite (84.0%), handling of a death snake not being safe enough (78.0%), signs and symptoms of snakebite being determined by the type of snake responsible for the bite (78.0%), the rainy season being the season with most snakebite incidence in Ghana (74.3%), The five most poorly scored questions on knowledge about snakebite were; percentage of snakebite (out of hundred percent) that may come from venomous snakes (1.1%), walking on a log of wood being the best thing to do to prevent snakebite when you come across a log of wood on your path in the forest (11.2%), number of times a venom will be injected into a victim out of hundred bites (13.4%), sleeping under mosquito nets preventing snakebites (32.1%) and the day being the most common time of snakebite (37.0%). The overall average knowledge score of the respondents on snakebite was 13.78 ± 4.000/22 (63%). Table 4 shows knowledge of respondents on snakebite.
Table 4: Knowledge of respondents on snakebite.
| Question |
Responses |
Mean knowledge score ± SD | Percentage knowledge score | ||
| Sub-group/
Correctness |
Frequency | Percentage | |||
| State 3 ways a person can prevent snake bitesa | 0/3 | 3 | 1.6 | 2.53 ± 0.758 | 84.0 |
| 1/3 | 21 | 11.2 | |||
| 2/3 | 36 | 19.3 | |||
| 3/3 | 126 | 67.4 | |||
| Handling a dead snake’s head is safe enough? (No) | Incorrect | 41 | 21.9 | 0.78 ± 0.416 | 78.0 |
| Correct | 145 | 77.5 | |||
| Fang marks can always be seen or found on the victim after every snake bite? (No) | Incorrect | 57 | 30.5 | 0.69 ± 0.462 | 69.0 |
| Correct | 129 | 69.0 | |||
| Can a person report at the hospital with symptoms of snake bite toxin injection without actually being bitten by a snake after he or she might have been pricked by an object he or she suspected to be a snake? (Yes) | Incorrect | 70 | 37.4 | 0.62 ± 0.486 | 62.0 |
| Correct | 116 | 62.0 | |||
| Sleeping under mosquito nets can prevent snakebites. (Yes) | Incorrect | 126 | 67.4 | 0.32 ± 0.469 | 32.1 |
| Correct | 60 | 32.1 | |||
| Do you think every time a venomous (“poisonous”) snake bites, it always injects venom (poison) into the victim? (No) | Incorrect | 93 | 49.7 | 0.50 ± 0.501 | 50.0 |
| Correct | 93 | 49.7 | |||
| Which of the following is best used to determine if a person bitten by a snake had venom actually being injected into him or her by the snake?b | Incorrect | 64 | 34.2 | 0.66 ± 0.476 | 65.2 |
| Correct | 122 | 65.2 | |||
| Signs and symptoms of snake bites are determined by the type of snake responsible for the bite. (Yes) | Incorrect | 41 | 21.9 | 0.78 ± 0.416 | 78.0 |
| Correct | 145 | 77.5 | |||
| State 3 local symptoms and signs you will see on the part of the human body bitten by a snake.c | 0/3 | 4 | 2.1 | 2.78 ± 0.612 | 93.0 |
| 1/3 | 7 | 3.7 | |||
| 2/3 | 14 | 7.5 | |||
| 3/3 | 161 | 86.1 | |||
| State 3 general or systemic signs and symptoms that may be exhibited by a venomous snake bite victim.d | 0/3 | 20 | 10.7 | 2.12 ± 1.030 | 71.0 |
| 1/3 | 28 | 15.0 | |||
| 2/3 | 47 | 25.1 | |||
| 3/3 | 91 | 48.7 | |||
| Out of ONE HUNDRED (100) snake bites, what percent may come from venomous snakes? (30) | Incorrect | 184 | 98.4 | 0.01 ± 0.103 | 1.1 |
| Correct | 2 | 1.1 | |||
| Out of ONE HUNDRED (100) bites by venomous snakes, how many times do you think venom will be injected into the victim? (50) | Incorrect | 161 | 86.1 | 0.13 ± 0.342 | 13.4 |
| Correct | 25 | 13.4 | |||
| The signs and symptoms of snake bite depends on the amount of venom injected by the snake. (Yes) | Incorrect | 73 | 39.0 | 0.61 ± 0.490 | 60.4 |
| Correct | 113 | 60.4 | |||
| What time of the day do you think snake bites are most common? (During the day) | Incorrect | 117 | 62.6 | 0.37 ± 0.484 | 37.0 |
| Correct | 69 | 36.9 | |||
| Which season in Ghana is snake bites most common? (Rainy) | Incorrect | 47 | 25.1 | 0.75 ± 0.436 | 74.3 |
| Correct | 139 | 74.3 | |||
| When you are walking in the forest or farm and you come across a log of wood across your path, what would be the best thing to do prevent being bitten possibly by a snake? e | Incorrect | 165 | 88.2 | 0.11 ± 0.317 | 11.2 |
| Correct | 21 | 11.2 | |||
| Overall mean score | 13.78 ± 4.000/22 | (63%) | |||
aKeep grass short or the ground clear around your house; Clear underneath low bushes to close to the house; Avoid keeping livestock in the house; Store food in rat- proof containers; Do not have tree branches touching your house; Use a light and proper shoe when walking at night; Clear heaps of rubbish from near your house. bSigns and symptoms. cPain, swelling, fang marks, blisters formation, swollen lymph nodes draining the site, local bruising and bleeding, redness of the site. dBleeding and clotting disorders, dizziness, blurred vision, and syncope which may occur as a result of hypotension after the bite, Transient paraesthesiae of the tongue and lips, heaviness of the eyelid, nausea and vomiting, bilateral ptosis, respiratory and generalized flaccid paralysis. eStep/walk on it. Correct answers are in parenthesis ( ) at the end of the question.
Association between Socio-Demographic Characteristics and Knowledge on Snakebite
Table 5 shows association between socio-demographic characteristics and knowledge on snakebite. Male respondents had a better means knowledge score on snakebites than their female counterparts (14.49 vs. 13.03) but the difference was not significant. Respondents from the CHPS compound significantly scored better than respondents from the health centres and hospitals (16.6 > 14.84 > 13.31; p < 0.03). Respondents from Central Tongu obtained the highest mean score, (14.36) on knowledge about snakebite, followed by North Tongu (14.28) and South Tongu scored the lowest (13.17) but the differences were not significant. Pharmacists and medical doctors significantly scored better than Physicians assistants (PAs), Pharmacist technicians, Community health nurses/Enrolled nurses (CHN/ENs) and Registered general nurses (RGNs) on knowledge on snakebite (p 15.09 > 13.35; p < 0.020). Respondents who had training on snakebite management significantly scored better than those who had not received training on snakebite management (15.60 vs. 12.98; p < 0.0001). There was no significant association between number of years of practice and knowledge on snakebite management. Respondents with more than 10 years of practice obtained the best mean score of 15.50, followed by < 5 years (14.13) and lastly 5-10 years (13.18) but the differences were not significant.
Table 5: Association between socio-demographic characteristics and knowledge on snakebite.
| Characteristic | Sub-group | Mean Score + SD | P-value |
| Sex | Male | 14.49 ± 3.670 | 0.12 |
| Female | 13.03 ± 4.210 | ||
| Type of health facility | CHPS compound | 16.60 ± 4.290 | 0.03* |
| Health centre | 14.84 ± 5.088 | ||
| Hospital | 13.31 ± 3.621 | ||
| District of health facility | South Tongu | 13.17 ± 3.593 | 0.152 |
| Central Tongu | 14.36 ± 4.107 | ||
| North Tongu | 14.28 ± 4.444 | ||
| Area of profession | RGN | 12.80 ± 3.107 | 0.023* |
| Pharmacist | 16.50 ± 3.416 | ||
| Medical officer | 16.50 ± 2.739 | ||
| Physician assistant | 14.05 ± 3.908 | ||
| CHN/EN | 13.96 ± 4.528 | ||
| Pharmacy technician | 15.40 ± 6.693 | ||
| Registered midwife | 14.27 ± 5.325 | ||
| Professional group | Nursing and midwifery group | 13.35 ± 3.921 | 0.020* |
| Prescribers | 15.89 ± 5.207 | ||
| Pharmacy group | 15.09 ± 3.625 | ||
| Training | No training | 12.98 ± 3.686 | <0.001* |
| Received training | 15.60 ± 4.118 | ||
| Number of years of practice | <5 years | 14.13 ± 4.186 | 0.240 |
| 5-10 years | 13.18 ± 3.386 | ||
| >10 years | 15.50 ± 2.121 |
*Statistically significant.
Discussion
The findings from the study showed that, majority, 95 (51.1%) of the respondents were males to similar studies in Nigeria and Cameroun but different from the study in Laos [10-12]. This could be because in Ghana, health care professional groups (medical doctors, pharmacists and pharmacy technicians, physician assistants) in exception of the nursing and midwifery profession are dominated by males although presently there are more males in the nursing profession than it used to be some years ago. Most of the respondents were within the age groups 30-39 years (52.7%)) and 20-29 years (43.3%). This age groups fall within the group considered to be the working age group (15 years and above) in Ghana by the Ghana Statistical Service (GSS) [9]. It is therefore not surprising that majority of health care professionals in the three districts are of a youthful age group. The result of the study also showed that the South Tongu district recorded the highest number of respondents, 87 (46.8%) in the study. This was because the South Tongu district has two main hospitals (the District hospital and Comboni hospital) and more health centres and CHPS compounds combined than the North and South Tongu districts. The results on the number of years of practice revealed that 112 (60.2%) of the respondents form the majority with less than five years of practice. This result corresponded with the findings of Michael et al. (2018) where 66.3% of the respondents were with < 10 years working experience. This could be due to the reason that most professionals who had served for more than five years had gone to further their studies as health professionals in Ghana are granted study leave after working for a period of 3 to 5 years. The study also revealed that majority, 146 (78.5%) worked at the hospitals while to 25 (13.4%) and 15 (8.1%) worked in the health centres and CHPS compound respectively. This is because the hospitals have larger number of health care professionals than the lower level health facilities. The nursing group (RGN: 43% and EN/CHN: 26.3%) formed the most common group of health workers in the study because of their dominance in terms of numbers in every health facility in Ghana. This result is in contrast with a similar study conducted in Lao People Democratic Republic (Lao PDR) and Cameroun where physicians formed the majority of the respondents [11,12]. The difference clearly could be the difference in the settings of the different studies and target groups involved in these studies.
The overall average knowledge score rated by the respondents on knowledge on snakes in the study was 46.2%. This score shows that the health care providers performed below average in the assessment of their knowledge about snakes. Health professionals were least knowledgeable about identity of various species of snakes. Similar study done in India [13] revealed that 65% of the respondents had poor information about snake identification. Similar studies in Lao, Nigeria and Cameroun also found health professional exhibiting poor knowledge on identification of snakes [10-12]. This means the health training schools in many countries do not have enough materials on snakes and snakebites and even after graduation, not many health authorities organize in-service training on snakes and snake bite management. This is of a great concern because, to be able to determine whether envenoming could occur or had occurred after a snakebite, the health care professionals need to identify the type of snake involved in the bite if brought along or upon description by victim or relatives. Knowing that the offending snake species is venomous, partially venomous or nonvenomous will guide the health care professional on how best to manage the condition and whether it will be necessary to administer anti-snake venom which is usually difficult to get in many countries. Despite the low overall level of knowledge, male health workers possess a significantly better knowledge on snakes than females. The difference in knowledge score between the sexes on snakes could possibly be because women generally fear snakes and would do everything to avoid issues concerning snakes [14]. The reason why health care providers working in the lowest part of the health system (CHPS zones and health centres) had better score on knowledge on snakes than those working in the higher level (hospitals) could be because since they work in more rural communities where snakes are more common, they will invariably be more familiar with snake species than those from the facilities located in the bigger towns where encounters with snakes are less common. The results of this study also showed that the prescribers (medical officers and physician assistants) and the pharmacy group (pharmacists and pharmacy technicians) had better knowledge on snakes than the nurses and midwives just as reported in the Cameroonian study [11]. These differences in knowledge between these groups of health care professionals could be because the prescribers and the pharmacy professionals may have had more training on snakebite management than the nurses and the midwives. Again, the prescribers also play important role in the management of snakebites while the pharmacy personnel supply the medications but the involvement of a nurse in the snakebite issues depended on his or her area of work. The study showed a high level of knowledge among the health care professionals on the local signs and symptoms (93.0%) and preventive measures (84.0) of snakebites. These results corroborated the findings in a similar study in Northern Nigeria where respondents scored 62.3% on clinical features of snakebite and 97.1% on preventive measures [10]. The reason that could account for the high level of knowledge among the health care professional on the local sign and symptoms of snakebite could be that most of them have severally seen victims of snakebite reporting to the health facility presenting with these signs and symptoms. The study also revealed that majority (74.3%) of the respondents knew that snake bites occur more often during the rainy season in Ghana. The high knowledge on the season with the most prevalence of snakebite may be because during the rainy season, the number of snake bite cases reporting to the health facilities increases as compared to the dry season. The overall average knowledge score of 63.0% on the knowledge about snakebite is an indication of some deficit in knowledge of health care professionals in the Tongu districts about snakebites. The overall knowledge score on snakebite is a little higher (63.0% vs. 52.9%) than what was recorded in the study conducted among physicians in Northern Nigeria [10]. A study in Cameroon also recorded poor knowledge on snake bites among health professionals [11]. This study therefore reveals a yawning gap between what our health care professionals should know and what they know about snakes and snake bites which will compromise their management of victims of snake bites. If health workers in rural environments where more snake bites will be reported seem to possess such low level of knowledge about consequences and management of effects of human snake conflict, then it can be extrapolated to mean than health practitioners in urban areas will be more deficient in snake bite management. This study however had some limitations worth noting. This study was conducted in only three out of about two hundred and sixty districts of Ghana so may not represent the situation across the country. Again, since convenience sampling was used in the selection of the nursing professionals, there may be some biases in their selection which can affect the generalization of the results of this study. Despite these limitations, the outcomes of this study being the first of its kind in Ghana, should cause health policy-makers to provide more in-service training on snakes and snake bites to all health workers so as to bridge the gap of knowledge deficit. Again, health training institutions should include snake bites issues in their academic curricula so that their trainees will be adequately equipped to help reduce morbidity and mortality associated with snake bites after graduation.
Conclusion
This study had shown some inadequacies in knowledge regarding snakes and snakebites among health care professional in the three Tongu districts of the Volta region of Ghana. Since in-service training was associated with respondents’ knowledge on snakes and snakebite, there is a clear need for improvement in knowledge about snakes and snakebites among health workers in the three Tongu districts and across the Ghana.
Acknowledgement
We wish to acknowledge the support of heads of health facilities where the data was collected for granting the permission for the study to be conducted in their health institutions. We also acknowledge the support given the team of researchers by health workers in the North, Central and South Tongu districts of the Volta region. The authors had no conflict of interest in this research since the study was funded by the researchers themselves.
References
- WHO Regional Office for Africa. Guidelines for the prevention and clinical management of snakebite in Africa: Mauritius. 2010. Retrieved April 15 2019 from
http://afrolib.afro.who.int/documents/2010/En/Snakebite_guidelines.pdf. - Habib AG. Public health aspects of snakebite care in West Africa: perspectives from Nigeria. Journal of Venomous Animals and Toxins including Tropical Diseases. 2013;19:1-4.
https://doi.org/10.1371/journal.pntd.000671 - Prevalence of snakebite envenoming. 2019a. Retrieved June 5, 2019 from
https://www.who.int/snakebites/epidemiology/en/ - Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, Savioli L, Lalloo DG, de Silva HJ. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008 Nov 4;5(11):e218.
- Snakebite envenoming. 2019b. Retrieved May 21, 2019 from
https://www.who.int/snakebites/treatment/Diagnostic_tests_and_tools/en/ - Williams D, Gutiérrez JM, Harrison R, Warrell DA, White J, Winkel KD, Gopalakrishnakone P. The Global Snake Bite Initiative: an antidote for snake bite. The lancet. 2010 Jan 2;375(9708):89-91.
- Chippaux JP. Snakebite envenomation turns again into a neglected tropical disease! Journal of Venomous Animals and Toxins including Tropical Diseases. 2017 Dec;23(1):38.e218.
- Wingert WA, Chan L. Rattlesnake bites in southern California and rationale for recommended treatment. Western Journal of Medicine. 1988 Jan;148(1):37.
- Ghana Statistical Service. Population and Housing Census Summary Results of Final. 2012. Retrieved July 17, 2019 from
http://statsghana.gov.gh/gssmain/storage/img/marqueeupdater/Census2010_Summary_report_of_final_results.pdf - Michael GC, Grema BA, Aliyu I, Alhaji MA, Lawal TO, Ibrahim H, Fikin AG, Gyaran FS, Kane KN, Thacher TD, Badamasi AK. Knowledge of venomous snakes, snakebite first aid, treatment, and prevention among clinicians in northern Nigeria: a cross-sectional multicentre study. Transactions of The Royal Society of Tropical Medicine and Hygiene. 2018 Feb 1;112(2):47-56.
- Taieb F, Dub T, Madec Y, Tondeur L, Chippaux JP, Lebreton M, Medang R, Foute FN, Tchoffo D, Potet J, Alcoba G. Knowledge, attitude and practices of snakebite management amongst health workers in Cameroon: Need for continuous training and capacity building. PLoS neglected tropical diseases. 2018 Oct 25;12(10):e0006716.
- Inthanomchanh V, Reyer JA, Blessmen J, Phrasisombath K, Yamamoto E, Hamajima N. Assessment of knowledge about snakebite management amongst healthcare providers in the provincial and two district hospitals in Savannakhet Province, Lao PDR. Nagoya journal of medical science. 2017 Aug;79(3):299.
- Pandve HT, Makan A, Kulkarni TA. Assessment of awareness regarding snakebites and its related issues among rural communities. SF J Pub Health. 2017;1(1).
- Rakison DH. Does women’s greater fear of snakes and spiders originate in infancy?. Evolution and Human Behavior. 2009 Nov 1;30(6):438-444.