Abstract
Helicobacter pylori is considered one of major carcinogens organisms which cause gastric, pancreatic and lung cancers. Arising studies are still to understand about relationship between H-pylori and tumor markers. Patients undergoing liver transplantation are put under a full investigation protocol for exclusion criteria, yet H-pylori infection is not well considered.
Objectives: To study findings associated with detection of H-pylori in Egyptian patients recruited for liver transplantation and taking into consideration their prognostic value.
Material and methods: a retrospective study of 40 cases of patients recruited for liver transplantation at the National Hepatology and Tropical Medicine Research Institute (NHTMRI). Data include patient Age and sex, Blood group, Hepatitis viral markers, Tumor markers (CA125, CA19.9, CEA, and AFP), Bilharzial Ag/Ab and Autoimmune profile (ASMA, ANA and AMA). Histopathologic and immunohistochemical assessment of H-Pylori expression in hepatic tissue and pre hepatic lymph nodes.
Results: there was a significant relation between Anti-H-pylori Antibody expression in lymph node tissue to the tumor marker (CA 19.9) in studied cases with significant (P value 0.046). More than 80% of studied cases that showed dysplasia in liver tissue express Anti-H-pylori antibody in liver tissue. The relation between Anti-H-pylori Antibody expression in lymph nodes and dysplasia in liver tissue of studied cases was statistically significant (p value=0.037).
Conclusion: H-pylori infection should be considered among the causes of CA 19-9 elevation so that needless interventions and health expenses can be prevented. While in case of transplantation, presence of H-pylori as a carcinogen should be fully evaluated with consideration to other tumor markers and serological markers with new scoring formulation strategies.
Abbreviations: AFP: Alpha Feto Protein; AMA: Anti-Mitochondrial Antibody; ANA: Anti-Nuclear Antibody; ASMA: Anti-Smooth Muscle Antibody; CA: Carbohydrate Antigen; CEA: Carcino-Embryonic Antigen; CMV: Cytomegalovirus; EBV: Epstein-Barr Virus; HBV: Hepatitis B Virus; HCC: Hepatocellular Carcinoma; HCV: Hepatitis C Virus; IgG: Immunoglobulin G; LN: Lymph Nodes; MALT: Mucosa Associated Lymphoid Tissue Lymphoma; AILD: Autoimmune Liver Disease; TGFB: Transforming Growth factor B1
Introduction
As Liver transplantation survival rates frequency has been increased, postoperative management of recipients requires more attention. Increasing reports about de novo gastric cancer after transplantation and there are many studies about critical role of H-pylori infection as a gastric carcinogen. Chronic inflammation, Immune stimulation and cellular proliferation have been always implicated in tumors pathogenesis, thus this pathogenesis progression should always be investigated and monitored in post transplantation patients [1-3].
Other long-term complications of H-pylori should also be well investigated, studying serological findings associated with detection of H-pylori in Egyptian patients recruited for liver transplantation is a key step to predict and prevent complications and their pathogenesis.
Material and Methods
A retrospective study of 40 cases of cirrhotic patients with decompensated end stage liver disease recruited for liver transplantation collected from the National Hepatology and Tropical Medicine Research Institute (NHTMRI). The study protocol was approved by The Research Ethics committee (REC) GOTHI on 13 -1- 2021. Data were collected from reports regarding personal data (age and sex), clinical, laboratory and pathological data. data were collected and tabulated. The following data and investigations were collected and done at NHTMRI: – Age and sex of patient. – Blood group. – Hepatitis viral markers. – Tumor markers (CA125, CA19.9, CEA and AFP). – Bilharzial Ag/Ab. – Autoimmune profile (ASMA, ANA and AMA). – Histopathological findings in the liver (Cholestasis, Dysplasia and HCC). – Etiology of cirrhosis. Histopathologic, Staining and Immunohistochemical Assessment of Anti-H-pylori antibody expression in hepatic tissue and enlarged prehepatic LNs.
Statistical Method
The collected data was revised, coded tabulated and introduced to a PC using Statistical package for Social Science (SPSS 25)
Results
Demographic Data
Results showed that the majority (36 cases) of studied liver cirrhotic cases were male patients. As for age in our study ranges between 20 and 60 years old with mean age about 44years. With 70% of them above the age of 40 years.
Blood Group
Blood groups are shown in the below Graph 1.
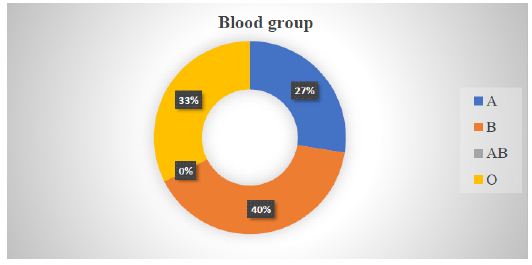
Graph 1: Distribution of cases according to the blood group of studied cases: 40% of cases were blood group B.
Virology Profile
More than half of cases were HCV positive.
- All patients were EBV IgG (Epstein-Barr virus) CMV (Cytomegalovirus) IgG positive (Graph 2).
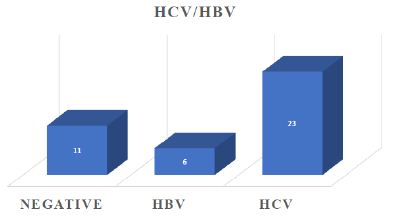
Graph 2: Distribution of cases according to viral markers (HBV and HCV) of studied cases.
Bilharziasis
More than 70% of cases were negative bilharzial Ag/Ab.
Etiology of Cirrhosis
Regarding etiology of cirrhosis, more than 50% of cases were HCV related cirrhosis.
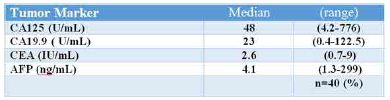
Tumor Markers
- Tumor markers showed average values at time of transplantation; cases showed normal level of CA125 (50%), AFP level (62%), CEA level (92%) and CA19.9 (72%) (Table 1).
Table 1: Tumor markers of total studied group at time of transplantation.
Autoimmune Profile
Regarding autoimmune profile, more than half of studied cases were positive for ASMA (Anti smooth muscle antibody) and > 72% were negative for ANA (Antinuclear antibody). All patients were AMA negative.
Pathological Data
Regarding to histopathological findings in liver tissue, more than 50% of studied cases were positive cholestasis, 40% of them were positive dysplasia while 25% were positive for hepatocellular carcinoma (Graph 3).
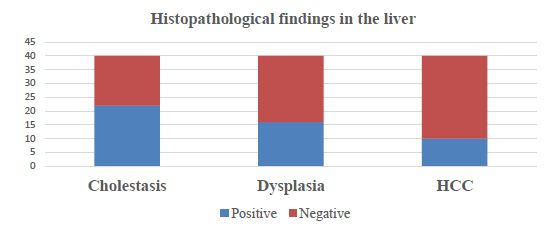
Graph 3: Distribution of cases according to liver findings (cholestasis, dysplasia, and HCC) in studied cases.
Anti H-pylori Antibodies
85% of studied cases were positive for anti H-pylori antibodies in liver tissue while 70% of studied cases were positive for anti H-pylori antibodies in the LN tissue (Graph 4).
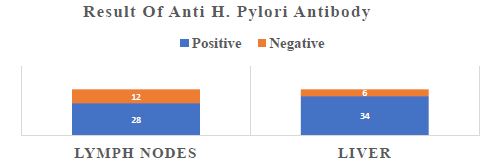
Graph 4: Distribution of cases according to Anti-H. Antibody expression in liver and LN tissues of studied cases.
Expression of Anti H-pylori Antibodies with Age
The relation between age groups and Anti-H. Antibody expression in liver of studied cases was statistically significant (p value=0.006). About 80% of cases with positive anti H antibodies in liver were above age of forty (Graph 5).
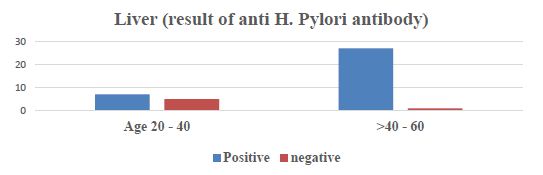
Graph 5: Relation between age group and Anti-H. Antibody expression in liver of studied cases.
Expression of Anti H-pylori Antibodies with Blood Groups
- All blood group A and O cases express Anti-H antibody in liver tissue, while less than forty percent of blood group B cases didn’t express Anti-H antibody in liver tissue.
A statistically significant relationship was obtained between Anti-H. Antibody expression in liver and (O) blood group in studied cases (p value=0.006) while the relation between Anti-H. Antibody expression in lymph nodes and (O) blood group in studied cases was statistically insignificant (p value=0.908) (Graph 6).
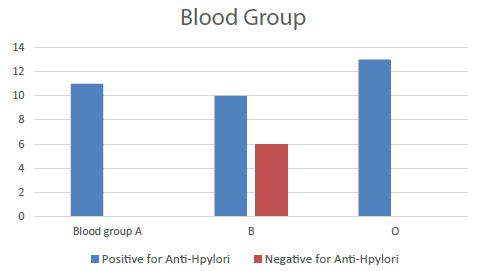
Graph 6: Relation between Anti-H. Antibody expression in liver and blood groups in studied cases.
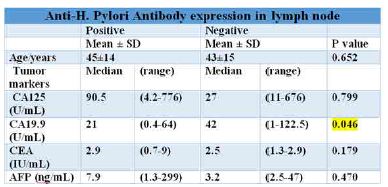
Expression of Anti H-pylori Antibodies with Tumor Markers
Relation between Anti-H-pylori Antibody expression in lymph node tissue to the tumor marker (CA 19.9) in studied cases was significant (P value 0.046) (Table 2).
Table 2: Relation of Anti-H. Antibody expression in lymph node to age group and tumor markers in studied cases.
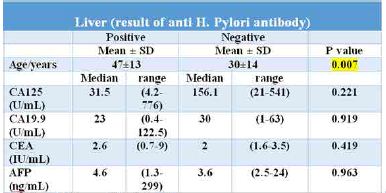
Relation of Anti-H
Antibody expression in liver to age group: mean age positive cases was 47 years with ±13 in contrast with 30 years with SD ±14 negative cases with significant P value (0.007). Relation of Anti-H. Antibody expression in liver to tumor markers in studied cases was Insignificant (Table 3).
Table 3: Relation of Anti-H. Antibody expression in liver to age group and tumor markers in studied cases.
Pathological Findings
Expression of anti H-pylori Antibodies with Dysplasia
50% of studied cases that showed dysplasia in liver tissue expressed Anti-H. Pylori antibody in the lymph nodes. The relation between Anti-H. Pylori Antibody expression in lymph nodes and dysplasia in liver tissue of studied cases was statistically significant (p value=0.037).
More than 80% of studied cases that showed dysplasia in liver tissue express Anti-H. Pylori antibody in liver tissue. 17% of studied cases that were negative for dysplasia in liver tissue didn’t express Anti-H. Pylori antibody in liver tissue (Graph 7).
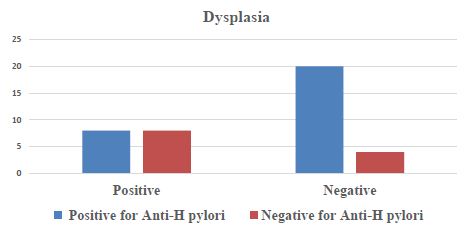
Graph 7: Relation between Anti-H. Antibody expression in lymph nodes and dysplasia in studied cases.
Expression of anti H-pylori antibodies with HCC
60% of cases that were positive HCC in liver expressed Anti-H. antibody in lymph nodes. A statistically significant relationship was obtained between Anti H-pylori antibody expression in lymph nodes and HCC in liver of studied cases (p value=0.041).
All cases that showed HCC in liver tissue express Anti-H. Pylori antibody in the liver tissue while 29% of the cases that were negative for HCC in liver tissue didn’t express Anti-H. Pylori antibody in the lymph nodes. A statistically insignificant relationship was obtained between Anti-H. Pylori Antibody expression in lymph nodes and HCC in liver tissue of studied cases (p value=0.307) (Graph 8).
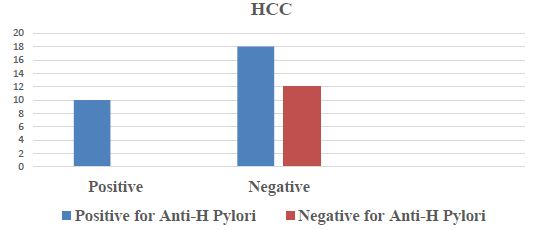
Graph 8: Relation between Anti-H. Antibody expression in lymph nodes and presence of HCC in liver of studied cases.
Discussion
This study, alongside earlier investigations, showed that H. pylori is a liver carcinogen and plays a crucial role in the genesis of several liver diseases. Because it increases the risk of developing hepatocellular carcinoma (HCC), which has a high mortality and morbidity rate, hepatic cirrhosis is particularly significant [4]. Mekonnen et al. [5] state that H. pylori infection should be viewed as a liver oncogenic organism similar to HCV because it is more prevalent in HCC patients than in controls. Another study that identified H-pylori and its related groups in hepatic tissue samples from patients with cholangiocarcinoma and HCC agreed with that [6]. H-pylori infection increased HCC development passing through increased vascular mediators and inflammatory markers. Furthermore, eliminating it might lower the likelihood of these side effects [7]. CA 19-9 is also produced by ductal cells in the pancreatic and biliary system, as well as epithelial cells in the stomach, colon, uterus, and salivary glands. Although high amounts of CA 19-9 can be found in a number of gastrointestinal and gynaecological cancers, it is particularly useful as a marker for pancreaticobiliary tumours [8]. CA 19-9 is utilised to monitor pancreatic cancer patients since it is elevated in various gastrointestinal malignancies, such as colorectal, hepatic, and esophageal cancers.
Awama et al. [9] found that the relationship between Helicobacter pylori infection and levels of CA 19-9 showed no significance in patients with benign gastrointestinal diseases, another study agreed [10] and concluded that CA19.9 was unable to predict the presence of HP. In our study, CA19.9 showed unexplained significant relationship with Anti-H-pylori Ab expression in LN tissue. Anti-H. pylori Antibody Expression in Lymph Nodes and HCC in the Liver Tissue of Studied Cases were Found to Be Statistically Insignificantly Associated in This Study (p value=0.307). A study mentioned that in some conditions of benign cases of pancreatic and gastric disorders there is a notable high increase in CA 19-9 serum level that returns normal after effective treatment which may result in rapid serum CA 19-9 levels normalization. The proliferation of epithelial cells under those circumstances may explain this elevation, and that H-pylori infection-related inflammatory cytokines are a significant contributor to this elevation., specially it was noted that CA 19-9 returns to normal levels after eradication of H-pylori infection. It is challenging to detect the precise cause of the CA 19-9 elevation whether due to benign versus malignant conditions. So that CA19-9 is not considered a sensitive tumor marker on its own and combined use of other tumor markers as CEA and CA125 is recommended to overcome the confusion caused by CA19-9 elevation. But this suggestion is not widely accepted yet.
Another case report study found a significant rise of CA19.9 in a 68-year man infected with H-pylori suis [11], they mentioned that in cases of high CA19.9, in addition to H-pylori, infection with non-human H-pylori species should be considered. Its implication in carcinogenesis is also patent. While more data is required to confirm a direct relationship, this CA 19-9 elevation is assumed to be related to the same factors: gastric epithelial cells proliferation and inflammatory cytokines. After treatment and condition improvement, the biological follow-up showed CA 19-9 levels normalization.
The development of gastric mucosa associated lymphoid tissue (MALT) lymphoma is a multistep process as H. pylori infection is followed by the recruitment of immune cells to the stomach mucosa. [12]. Due to the presence of H. pylori, persistent inflammation is frequently linked to gastric MALT lymphoma. The pathophysiology of non-gastric MALT lymphomas is likewise thought to include chronic immunological activation, therefore autoimmune diseases are frequently present. Neoplastic cells present in epithelial structures and subsequent damage to the glandular architecture, resulting in lymphoepithelial lesions, are distinguishing characteristics of MALT lymphoma [13]. In the same scope, antibodies as AMA, ANA and ASMA have been associated with range of diseases that respond to these autoantibodies leading to inflammation and initiation of the hepatic tissue injury in autoimmune liver disease (AILD) patients. Earlier studies found that positive rates of ANA, AMA and SMA were higher in H-pylori infected patients than in patients with negative H-pylori infection [14]. Such findings suggest that immunological disturbances could be associated with future risk of pathogenesis and development of lymphomatous neoplasms, AILD and possible graft rejection.
In the current study, the lymph nodes of 70% of cases were having anti-H. pylori antibodies. Ito et al. [15] found that macrophages in 85% of patients’ lamina propria and in 63% of patients’ paracortical regions of their gastric LNs
Conclusion
In developing countries as Egypt, H-pylori infection is a common health problem with many well-known sequences and other undetermined ones. H-pylori must be considered as a cause of elevation of ca19-9 and ASMA titre elevation. And so, a lot of needless investigations and health care expenses could be saved. While in case of transplantation, presence of H-pylori as a carcinogen should be fully evaluated with consideration to other tumor markers and serological markers with new scoring formulation strategies.
References
- Nasser GN, Mara K, Watt KD (2021) ‘De novo colorectal and pancreatic cancer in liver‐transplant recipients: Identifying the higher‐risk populations’. Hepatology 74: 1003-1013. [crossref]
- Tempera PJ, et al. (2022) ‘Gastric cancer due to chronic H-pylori infection: What we know and where we are going’. Diseases 10: 57. [crossref]
- Zhao H et al. (2021) ‘Inflammation and tumor progression: Signaling pathways and targeted intervention’. Signal Transduction and Targeted Therapy 6: 1.
- Goo MJ, Ki MR, Lee HR et al. (2009) Helicobacter pylori promotes hepatic fibrosis in the animal model. Lab Invest 89: 1291-1303.
- Mekonnen HD, Fisseha H, Getinet T et al. (2018) Helicobacter pylori Infection as a Risk Factor for Hepatocellular Carcinoma: A Case-Control Study in Ethiopia. Int J Hepatol. [crossref]
- Nilsson HO, Mulchandani R, Tranberg KG et al, (2001) Helicobacter species identified in liver from patients with cholangiocarcinoma and hepatocellular carcinoma. Gastroenterology 120: 323-324. [crossref]
- Abdel RA, Mousa N, Elhelaly R (2020) Helicobacter pylori as an Initiating Factor of Complications in Patients with Cirrhosis: A Single-Center Observational Study. Front Med (Lausanne) [crossref]
- Lee T, Teng TZ, Shelat VG (2020) World Journal of Gastrointestinal Surgery 12: 468-490. [crossref]
- Awama M, Makhlouf S, Karamya ZA (2021) A Study of the Relationship between CA 19-9 Level and Infection with H-pylori in Patients with Benign Gastrointestinal Diseases. Journal for Research and Scientific Studies – Health Sciences Series.43: 1.
- TAŞÇI B, GÜRLER M (2022) Retrospective Evaluation of the Role of CA19 Hematological Parameters in the Prediction of Helicobacter Pylori 9, CEA and Gastritis Etiology and Endoscopic Lesions. Ulutas Med J 8: 1.
- Capirchio L, Huang TD, De C, Witte, et al. (2022) Elevated carbohydrate antigen 19-9 following helicobacter suis gastritis and normalization after eradication: first case report and review of the literature. Acta Gastroenterol Belg 85: 403-405. [crossref]
- Navsaria L, Badillo A, Wang M (2020) ‘Second cancers in a patient with gastric malt lymphoma’, Case Reports in Medicine 1-4.
- Troppan K, et al. (2015) Molecular pathogenesis of Malt Lymphoma, Gastroenterology research and practice. [crossref]
- Ito T, Kobayashi D, Uchida K et al. (2008) Helicobacter pylori invades the gastric mucosa and translocates to the gastric lymph nodes.664-681. [crossref]
- Beretta-Piccoli BT, Mieli-Vergani G, Vergani D (2021) Autoimmune hepatitis: Serum autoantibodies in clinical practice. Clinical Reviews in Allergy & Immunology 63: 124-137. [crossref]
- Pilotto A, Franceschi M (2014) Helicobacter infection in older people. World J Gastroenterol 20: 6364-6373. [crossref]
- Chakrani Z, Robinson K, Taye B et al. (2018) Association between ABO Blood Groups and Helicobacter pylori Infection: A Meta-Analysis. Sci Rep 8: 17604.