Abstract
Objective: Severalatient-, and operator related factors have been confirmed to be of importance for blood loss in orthognathic surgery, e.g., type of surgical intervention and operative time. However, the surgeon´s impact has been studied only to a limited extent. Thus, the primary aim of this study was to evaluate the surgeon´s impact on intraoperative blood loss.
Methods: Clinical data was gathered retrospectively for all osteotomies performed by three different experienced surgeons between January 1, 2013 to December 31, 2016 at a regional centre for orthognathic surgery at the Sahlgrenska University hospital, Gothenburg, Sweden.
Results: A total of 179 patients (92 women and 87 men) who underwent Le Fort I osteotomy, Bilateral Sagittal Split osteotomy, or Bi-maxillary osteotomy were included. No statistically significant difference was seen between the three surgeons for intraoperative blood loss. Conclusions: Intraoperative blood loss during orthognathic surgery is not operator dependent when experienced surgeons are compared.
Keywords
Bimaxillary surgery, Bilateral sagittal split osteotomy, Le Fort I
Introduction
Orthognathic surgical procedures are used to correct a wide range of malocclusions and maxillofacial deformities. Novel standardised planning modalities and surgical methods are generally safe and severe complications are rare but can be substantial if encountered [1]. Bleeding, intra-, and/or postoperatively is among the most recognised complication in conjunction with orthognathic surgery and is frequently documented in both operator and nursing reports [2].
During Le Fort I (LFI) osteotomy, i.e., down-fracturing and mobilising of the maxillary segment of the viscerocranium, bleeding can occur by rupture of the maxillary artery and its collateral branches (descending palatine artery, sphenopalatine artery) or by damage to vessels in the pterygoid venous plexus [3,4]. The maxillary artery along with its terminal branches are commonly damaged in LFI osteotomy, especially during separation of the pterygomaxillary junction [5]. In contrast, haemorrhages associated with mandibular osteotomies, e.g., intra-, or extraoral vertical ramus osteotomy, or bilateral sagittal split osteotomy (BSSO), occur less frequently [3]. Nevertheless, once they ensue the haemorrhages are likely to originate from the maxillary artery or vessels in its dispersed vascular network [3].
There are several patient-, and operator related factors that are of importance for blood loss. However, in previous studies a direct correlation between the complexity of the surgical interventions and intraoperative blood loss has been demonstrated. Patients who are treated with Bi-maxillary osteotomy (LFI + BSSO) have a significantly higher blood loss compared to those who receive LFI or BSSO [2,6]. Other studies have promoted that intraoperative blood loss differs with the operative time [3,7-9]. It has further been speculated, but only investigated to a lesser extent whether the surgeon has an impact on the intra operative blood loss during the aforementioned surgical procedures.
Thus, the primary aim of this study was to evaluate the surgeon´s impact on intraoperative blood loss. Secondary aims were to evaluate the difference in blood loss between surgical procedures, and operative time (OT) for each surgical procedure.
Methods
Study Design
This study was a retrospective review of medical charts and databases at the Department of Oral and Maxillofacial Surgery, a regional centre for orthognathic surgery at the Sahlgrenska University hospital, Gothenburg, Sweden. We retrospectively analysed the patient records of all orthognathic surgery cases between January 1, 2013 to December 31, 2016, employing Melior (Siemens Healthineers AG, Erlangen, Germany), a digital record and documentation system used by healthcare facilities in Sweden today. The surgical procedures were carried out by three independent maxillofacial surgeons (A, B, C) with ≥ 15 years of experience in orthognathic surgery. As part of the clinical routines established for orthognathic surgery at our unit, one gram of Tranexamic acid solution was administered intravenously at start of the operation.
Study Population
Patients in the data base included in this study were: a) ≥ 18 years of age; b) had been treated with LFI, BSSO, or LFI + BSSO; c) the procedure had been carried out under hypotensive anaesthesia, defined as 20-30% reduction of mean arterial pressure (MAP). Patients were excluded: a) if the osteotomies were performed with additional genioplasty; or b) if the osteotomies were carried out for trauma, tumours, or cyst removals; c) smokers.
Data Collection
All the procedures in this retrospective study were conducted at the Department of Oral and Maxillofacial Surgery by the two investigators (MH, KW). The search strategy of the investigators had been previously calibrated to efficiently extract information, limit missing data and thus maintain standardisation in the study design. Specific information contained in the medical charts and databases for each patient included: i) gender, age; ii) medications prescribed which could potentially affect bleeding time; iii) surgical procedures (LFI, BSSO, LFI + BSSO); iv) principal surgeon; v) irrigation (sodium chloride 0.9%) and the total volume of blood collected in the suction unit, vi) OT, defined as the time from first incision to complete wound closure. The information obtained under paragraph v) was subsequently used to calculate the intraoperative blood loss, defined as estimated blood loss (EBL) in millilitre (mL) [2].
Objectives
The primary objective was:
(i) To evaluate the surgeon´s impact on EBL, for the procedures combined (EBL-total) and for each surgical procedure separately (EBL-LFI; EBL-BSSO; EBL-LFI + BSSO).
The secondary objectives were:
(ii-a) To investigate the difference in EBL between LFI, BSSO, LFI + BSSO.
(ii-b) To investigate the OT for LFI, BSSO, and LFI + BSSO, respectively.
Statistical Analysis
A power analysis (a priori) was performed for sample size estimation, based on data from a previous study [2] with similar measures. The effect size in this study was means (x̄ = 271 mL); standard deviations (SD = 149 mL). With an α-significance level = 0.05 and power = 0.8, the projected sample size needed with this effect size was n = 179 (G*power version 3.1.9.4; University of Düsseldorf, Germany).
Normality assumption was controlled using the Shapiro-Wilk test and a Gaussian distribution was confirmed for the tested variables. Descriptive data was presented with means (x̄) and standard deviations (SD). The primary, and secondary objectives were analysed using one‐way analysis of variance (ANOVA) followed by a Tukey correction for multiple comparisons. A p-value ≤ 0.05 was considered statistically significant. The analyses were employed using the IBM SPSS Statistics software package (IBM SPSS Statistics version 25, IBM Corp., Armonk, NY).
Ethical Considerations
All the procedures in this study including research on identifiable human data were performed in accordance with the ethical principles established in the WMA Declaration of Helsinki (Fortaleza, October 2013). The study was also reviewed and approved by the clinical lead at the Department Oral and Maxillofacial Surgery, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden. An ethical approval by the Swedish Ethical Review Authority itself was not requested since this was a coded data base study. Identification numbers of all patients were encrypted and transformed using a random number sequence.
Results
In total, 208 case records of patients treated with orthognathic surgery were identified during this study, of whom 208 patients met the inclusion criteria. Following a systematic evaluation of the collected records, 29 out of the 208 included patients were excluded, and the remaining 179 patients were carried forward for the statistical analyses. The foremost reason for exclusion was osteotomy with additional genioplasty surgery, 59% (n = 17/29). Other reasons for exclusion were osteotomy carried out to for trauma, tumours, or cysts, which together made up the remaining 41% (n = 12/29) of the excluded patients.
Among the 179 included patients 51% (n = 92/179) were women and 49% (n = 87/179) were men. The vast majority of the patients (91%; n = 163/179) consumed no medications that were of significant importance from a bleeding point of view whereas 9% (n = 16/179) were found to expend drugs that could affect the patient’s bleeding time. These drugs were non-steroidal anti-inflammatory drugs or oral contraceptives.
Bi-maxillary osteotomy, i.e., LFI + BSSO accounted for the highest proportion ofosteotomies (40%), followed by LFI (35%) and BSSO (25%), respectively. Table 1 provides a summary of the patient characteristics, osteotomies, and distribution of osteotomies among the three surgeons.
Table 1: Summary of patient characteristics, osteotomies, and distribution of osteotomies among the three surgeons
| Patient characteristics | ||||
| Age |
[years] |
23 | ± |
8 |
| Gender |
[F:M] |
92 | : |
87 |
|
51 |
% |
49 |
||
| Medications |
[Y:N] |
16 | : |
163 |
|
9 |
% |
91 |
||
| Osteotomies: | ||||
| LFI |
[Freq] |
62 | % |
35 |
| BSSO |
[Freq] |
44 | % |
25 |
| LFI + BSSO |
[Freq] |
73 | % |
40 |
| Total |
[Freq] |
179 | % |
100 |
| Osteotomies/surgeon: | ||||
| Surgeon A: | ||||
| LFI |
[Freq] |
21 | % |
34 |
| BSSO |
[Freq] |
5 | % |
11 |
| LFI + BSSO |
[Freq] |
25 | % |
34 |
| Total |
[Freq] |
51 | % |
28 |
| Surgeon B: | ||||
| LFI |
[Freq] |
17 | % |
27 |
| BSSO |
[Freq] |
24 | % |
55 |
| LFI + BSSO |
[Freq] |
34 | % |
47 |
| Total |
[Freq] |
75 | % |
42 |
| Surgeon C: | ||||
| LFI |
[Freq] |
24 | % |
39 |
| BSSO |
[Freq] |
15 | % |
34 |
| LFI + BSSO |
[Freq] |
14 | % |
19 |
| Total |
[Freq] |
53 | % |
30 |
LFI Le Fort I; BSSO Bilateral Sagittal Split Osteotomy; F Female; M Male; Freq Frequency. Y Yes; N No
When the volume of irrigation was subtracted from the total volume of blood collected in the suction unit, mean EBL-total for the entire study population was 354 ± 258 mL. Nevertheless, it varied considerably ranging from 20-1500 mL per operation. For the majority of all patients 75% (n = 135/179), an EBL between 100-500 mL was registered. The corresponding figures for the remaining 25% (n = 44/179) of the patients were as follows: 4% (8/179) < 100 mL; 15% (n = 26/179) 501-899 mL; and 6% (n = 10/179) ≥ 900 mL (Table 2).
Table 2: Distribution of estimated blood loss among the entire study population, including all three types of osteotomies
| Estimated blood loss (mL) | ||||
| < 100 |
[Freq] |
8 | % |
4 |
| 100-500 |
[Freq] |
135 | % |
75 |
| 501-899 |
[Freq] |
26 | % |
15 |
| ≥ 900 |
[Freq] |
10 | % |
6 |
The surgeon´s impact on EBL-total (mL; x̄ ± SD) revealed the following numbers for surgeon A (397 ± 294); B (372 ± 261); and C (287 ± 200). However, no statistically significant difference was seen for EBL-total between the three surgeons (Figure 1). A similar outcome was observed when the corresponding comparison was carried out to compare the three surgeons for EBL-LFI; EBL-BSSO; and EBL-LFI + BSSO (Table 3).
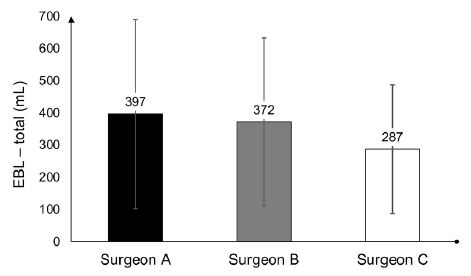
Figure 1: The surgeon´s impact on EBL – total. Datasets are presented as mean ± SD
Table 3: Analysis of the surgeons’ impact on EBL-LFI; EBL-BSSO; and EBL-LFI + BSSO. Datasets are presented as mean ± SD. A p-value ≤ 0.05 was considered statistically significant
|
Surgical procedures |
Estimated blood loss (mL) |
p–values |
||
|
Surgeon A |
Surgeon B |
Surgeon C |
||
| LFI |
330 ± 202 |
388 ± 268 | 307 ± 195 |
Ns |
| BSSO |
220 ± 244 |
213 ± 120 | 161 ± 80 |
Ns |
| LFI + BSSO |
489 ± 342 |
477 ± 280 | 389 ± 236 |
Ns |
LFI Le Fort I; BSSO Bilateral Sagittal Split Osteotomy; EBL Estimated Blood Loss; Ns Not significant
Furthermore, when mean EBL was calculated and subsequently compared between the three surgical procedures, the following figures were obtained (mL; x̄ ± SD): LFI (337 ± 218); BSSO (196 ± 126); and LFI + BSSO (464 ± 294). The ANOVA showed a statistically significant difference in mean EBL for all comparisons, i.e., [LFI] and [BSSO] (p = 0.008); [LFI] and [LFI + BSSO] (p = 0.006); and [BSSO] and [LFI + BSSO] (p < 0.001) (Table 4).
Table 4: The impact of the three surgical procedures, LFI; BSSO; and LFI + BSSO on EBL. Datasets are presented as mean ± SD. A p-value ≤ 0.05 was considered statistically significant
|
Comparisons of the surgical procedures |
Mean difference in EBL (mL) |
p–values |
|||
|
LFI |
BSSO | 141 |
0.008 |
||
|
337 |
± | 218 | LFI + BSSO | -127 |
0.006 |
|
BSSO |
LFI | -141 |
0.008 |
||
|
196 |
± | 126 | LFI + BSSO | -268 |
< 0.001 |
|
LFI + BSSO |
LFI | 127 |
0.006 |
||
|
464 |
± | 294 | BSSO | 268 |
< 0.001 |
LFI Le Fort I; BSSO Bilateral Sagittal Split Osteotomy; EBL Estimated blood loss
Ultimately, when OT was calculated for the three surgeons [A-C] individually, for each of the surgical procedures (LFI; BSSO, LFI + BSSO), the following figures were obtained (min; x̄ ± SD): LFI-[A]129 ± 58, [B] 103 ± 41, [C] 117 ± 30; BSSO-[A]104 ± 18, [B] 81 ± 18, [C] 109 ± 17; and LFI + BSSO-[A] 202 ± 71, [B] 172 ± 46, [C] 191 ± 24. A statistically significant difference was reached when OT was compared for BSSO between surgeon B and A (p = 0.031) as well as surgeon B and C (p < 0.001) (Table 5).
Table 5: Operative time for the three surgeons for each surgical procedure. Datasets are presented as mean ± SD. A p-value ≤ 0.05 was considered statistically significant
|
Surgical procedures |
Operative time (min) |
p–values |
||
|
Surgeon A |
Surgeon B |
Surgeon C |
||
| LFI |
129 ± 58 |
103 ± 41 | 117 ± 30 |
Ns |
| BSSO |
104 ± 18 |
81 ± 18 | 109 ± 17 |
0.031X and < 0.001Y |
| LFI + BSSO |
202 ± 71 |
172 ± 46 | 191 ± 24 |
Ns |
LFI Le Fort I; BSSO Bilateral Sagittal Split Osteotomy; Ns Not significant; [X] significant difference between surgeon B and A; [Y]significant difference between surgeon B and C
Discussion
The maxillofacial region is highly vascularised and even minor disruptions of the vessels in conjunctions with orthognathic surgery can jeopardise the blood supply to the actual region. Hence, seriously hamper the post-operative medical rehabilitation of the patient. In fact, severely damaged vessels constitute such a risk which may lead to a potentially fatal condition [10]. Over the past decades, a number of studies have been published investigating the potential association between patient-, or operator related factors and intraoperative blood loss [8,11]. Surprisingly, the impact of the surgeon on intraoperative blood loss has been studied only to a limited extent and needs to be further elucidated. This was the rationale for the conducting this four-year retrospective study.
The ANOVA showed no statistically significant difference between the three surgeons for EBL-total or for any of the surgical procedures separately. This was anticipated as the three surgeons were experienced and well-practised on the procedures performed in this study. However, it is worth mentioning that even if differences exist between operators with regards to EBL, it may be difficult to quantify. This for several reasons. First, extensive bleeding seldom occurs in conjunction with orthognathic surgery [10]. In fact, it has been shown that intraoperative blood loss is comparably low even when surgical residents are compared to experienced surgeons [11]. Second, all patients were given tranexamic acid prior to the surgical interventions, which is well-known to reduce the risk for bleeding [12,13] and improve the quality of the surgical field [13-15]. Third, the number of osteotomies were unequally distributed among the operators which may have influenced the outcome of this study. The latter however can be explained by the nature of retrospective studies where uneven cohorts may be encountered. Prospective, randomized studies where the number of patients and procedures are equally distributed among the operators is therefore warranted.
When the secondary objective (ii-a) was analysed, a statistically significant difference was found for EBL between all the surgical procedures. The maxillary osteotomies were bleeding significantly more as compared to the mandibular counterparts. This can be attributed to the fact that the maxilla encompasses a higher vascular density. Hence, entails a greater risk for bleeding [2]. In addition, some maxillary osteotomies were reported to bleed excessively, mainly due to aberrant anatomy, which had resulted in perforation of larger vessels. Some cases also reported a significant bleeding from the nasal mucosa during down fracturing-, or posterior repositioning of the maxilla. Bi-maxillary osteotomy as a group showed the highest EBL of the three surgical interventions, which is not surprising since it is the sum of both procedures. Taken together our findings seem reasonable and they are in accordance with previously published studies [2,6].
As for the secondary objective (ii-b), a statistically significant difference was seen when OT was compared for BSSO between surgeon B and A as well as surgeon B and C. However, although a statistically significant was observed, the clinical relevance remains questionable. Most likely, the additional time of approximately 25 min for operator A and C as compared to B will not lead to an increased EBL in clinical settings. This is supported by a study in which surgical residents required longer OT for their osteotomies as compared to the experienced surgeons, yet the EBL did not vary significantly [11].
Conclusions
Intraoperative blood loss during orthognathic surgery is not operator dependent when comparing experienced surgeons. However, both surgical procedure per se and operative time seem to be of relevance.
References
- Silva I, Suska F, Cardemil C, Rasmusson L (2013) Stability after maxillary segmentation for correction of anterior open bite: a cohort study of 33 cases. Journal of Cranio-maxillo-facial surgery: Official Publication of the European Association for Cranio-Maxillo-Facial Surgery 41: 154-8. [crossref]
- Salma RG, Al-Shammari FM, Al-Garni BA, Al-Qarzaee MA (2017) Operative time, blood loss, hemoglobin drop, blood transfusion, and hospital stay in orthognathic surgery. Oral and Maxillofacial Surgery 21: 259-266. [crossref]
- Pineiro-Aguilar A, Somoza-Martin M, Gandara-Rey JM, Garcia-Garcia A (2011) Blood loss in orthognathic surgery: a systematic review. J Oral Maxillofac Surg 69: 885-892. [crossref]
- Choi BK, Yang EJ, Oh KS, Lo LJ (2013) Assessment of blood loss and need for transfusion during bimaxillary surgery with or without maxillary setback. J Oral Maxillofac Surg 71: 358-365. [crossref]
- Apinhasmit W, Methathrathip D, Ploytubtim S, Chompoopong S, Ariyawatkul T (2004) Anatomical study of the maxillary artery at the pterygomaxillary fissure in a Thai population: its relationship to maxillary osteotomy. Journal of the Medical Association of Thailand 87:1212-1217. [crossref]
- Moenning JE, Bussard DA, Lapp TH, Garrison BT (1995) Average blood loss and the risk of requiring perioperative blood transfusion in 506 orthognathic surgical procedures. J Oral Maxillofac Surg 53: 880-883. [crossref]
- Yu CN, Chow TK, Kwan AS, Wong SL, Fung SC (2000) Intra-operative blood loss and operating time in orthognathic surgery using induced hypotensive general anaesthesia: prospective study. Hong Kong medical journal 6: 307-311. [crossref]
- Rummasak D, Apipan B, Kaewpradup P (2011) Factors that determine intraoperative blood loss in bimaxillary osteotomies and the need for preoperative blood preparation. J Oral Maxillofac Surg 69: 456-60. [crossref]
- Shetty V, Sriram SG (20150 Effectiveness of intravenous haemocoagulase on haemorrhage control in bi-maxillary orthognathic surgery-A prospective, randomised, controlled, double-blind study. Journal of Cranio-maxillo-facial surgery: Official Publication of the European Association for Cranio-Maxillo-Facial Surgery 43: 2000-2003. [crossref]
- Thastum M, Andersen K, Rude K, Norholt SE, Blomlof J (2016) Factors influencing intraoperative blood loss in orthognathic surgery. International Journal of Oral and Maxillofacial Surgery 45: 1070-1073. [crossref]
- Kretschmer W, Koster U, Dietz K, Zoder W, Wangerin K (2008) Factors for intraoperative blood loss in bimaxillary osteotomies. J Oral Maxillofac Surg 66: 1399-1403. [crossref]
- Zellin G, Rasmusson L, Pålsson J, Kahnberg KE (2004) Evaluation of hemorrhage depressors on blood loss during orthognathic surgery: a retrospective study. Journal of Oral and Maxillofacial Surgery 62: 662-666. [crossref]
- Lin S, McKenna SJ, Yao CF, Chen YR, Chen C (2017) Effects of Hypotensive Anesthesia on Reducing Intraoperative Blood Loss, Duration of Operation, and Quality of Surgical Field During Orthognathic Surgery: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Oral Maxillofac Surg 75: 73-86. [crossref]
- Barak M, Yoav L, Abu el-Naaj I (2015) Hypotensive anesthesia versus normotensive anesthesia during major maxillofacial surgery: a review of the literature. The Scientific World Journal 2015: 1-7. [crossref]
- Ervens J, Marks C, Hechler M, Plath T, Hansen D, (2010) Effect of induced hypotensive anaesthesia vs isovolaemic haemodilution on blood loss and transfusion requirements in orthognathic surgery: a prospective, single-blinded, randomized, controlled clinical study. International Journal of Oral and Maxillofacial Surgery 39: 1168-74. [crossref]