Abstract
Objective: COVID-19 became a pandemic and has caused a global emergency in the healthcare sector. Dental professionals pose high risk of viral spreading. This systematic review focused on COVID-19 infection control protocols in oral and dental medicine to derive an evidenced-based guideline.
Method: An electronic and manual search was performed for articles related to the outbreak of COVID-19 published between 2019/11/01 and 2020/03/31.
Results: Of the 53 titles retrieved by the systematic search, a total of 6 full-texts were included for data extraction.
Conclusions: Dental treatment must be limited to emergencies during the pandemic. Strict adherence to the hygiene chain is a prerequisite for the control of further transmission and protection of dental professionals. The use of aerosol-producing therapies must be minimized. Establishing regional dental emergency centers can help maintain the necessary capacities for society while maintaining appropriate hygiene standards. Personal protective equipment must be used in a resource-saving manner for dental emergencies of infectious patients.
Keywords
Corona virus, SARS-CoV-2, Pandemic, Dentistry, Public health
Introduction
The previously unknown coronavirus disease 2019 (COVID-19) and the pathogen SARS-CoV-2 (severe acute respiratory syndrome) with its specific virulence and pathogenesis quickly became a global pandemic [1]. The rapid spread from human-to-human through saliva, blood, and other body fluids have made it difficult to precisely determine its transmission pattern, extent of spread, and dangerousness. These factors, along with the fact that symptoms of COVID-19 infection are similar to types of viral influenza, led to an initial underestimation of the scale of the problem [2,3].
COVID-19 emerged in Wuhan City – capital of Hubei Province in China – and rapidly spread through South Korea, Japan, and Australia, then to Europe and the Middle-East, and recently North and South America [4]. The outbreak has spiraled into a global emergency for the healthcare sector, with wider economic damage and social restrictions, and unpredictable consequences in the future [5,6]. The most important characteristics of a pandemic are the spreading dynamics in time and space, the transmission rate and pathways, the incubation period, and the proportion of severe cases and mortality rate. The apparently high virulence of SARS-CoV-2, including the asymptomatic incubation period (up to 14 days), is a particular problem in this age of globalization [7,8].
Individuals with jobs that put them in close physical contact with many other people are at the greatest risk of becoming infected by
SARS-CoV-2 and for transmitting the infection onwards. The New York Times calculated the risk to be infected by SARS-CoV-2 for various occupations based on the risk of “exposure to disease” and “proximity to other humans” [9]. Healthcare workers were found to be at the greatest risk of encountering diseases and infections and typically work in close relationship to one another and their patients. In particular, dental care providers had the highest overall risk for SARS-CoV-2 infection, based on both exposure and physical proximity to others [9]. This clearly reflects the facts that dental care providers work directly with one of the known transmission routes of SARS-CoV-2, the oral cavity, and this is exacerbated by the use of rotating instruments or ultrasonic tips with aerosol production.
The key questions currently facing dental care workers are therefore: how should we act upon the COVID-19 crisis? And what are the adequate standards required for the well-being of patients and dental staff, considering different job groups, and also for the wider protection of society?
This review aimed to systematically screen the current literature on COVID-19 infection control protocols in oral and dental medicine to derive an evidenced-based guideline for stakeholders in the dental healthcare sector.
Methods and Meterials
The systematic review was conducted in accordance with the guidelines of Preferred Reporting Items of Systematic Reviews and
Meta-Analyses (PRISMA) [10]. An electronic search strategy of PubMed was performed for all types of publications reporting on COVID-19 in the oral medicine setting. The search was limited to articles published from around the time of the start of the outbreak to the present day (2019/11/01 to 2020/03/31). All types of publications were included. Search syntax comprised a combination of Medical Subject Headings [MeSH-Terms] and free-text words in simple or multiple conjunctions: ((“COVID-19” [All Fields] OR “2019-nCoV” [All Fields] OR “SARS-CoV-2” [All Fields] OR “coronavirus” [All Fields] OR “corona” [All Fields]) AND (“dentistry” [All Fields] OR “dental medicine” [All Fields] OR (“dental” [All Fields] AND “medicine” [All Fields]) OR “oral medicine” [All Fields] OR (“oral” [All Fields] AND “medicine” [All Fields]) OR “oral healthcare” [All Fields] OR (“oral” [All Fields] AND “healthcare” [All Fields]))) AND (“2019/11/01” [PDAT] : “2020/03/31” [PDAT]). An additional manual search of the bibliographies of all retrieved full-text articles and related reviews, selected from the electronic search, was conducted.
Two reviewers (T.J. and N.U.Z.) independently reviewed the titles of articles retrieved by the systematic literature search. Following this, the abstracts of all agreed titles were screened to identify articles that reported COVID-19 infection control protocols in oral medicine. The full texts of selected articles were obtained and data were extracted independently by the two reviewers using a data extraction form. Disagreements at each stage of the screening process were resolved by discussion. The following information was collected from the full text articles: a) authors including year of publication; b) country; c) publication type; and c) details of the COVID-19 infection control protocols reported in the articles.
Results
Of the 53 titles retrieved by the systematic PubMed search, 25 abstracts were further screened, and the full text of nine potentially relevant articles were obtained and reviewed. A total of six full-texts were included for data extraction, comprising four full-texts obtained from the electronic search plus one additional full-text obtained from the manual search (Figure 1) [11-16].
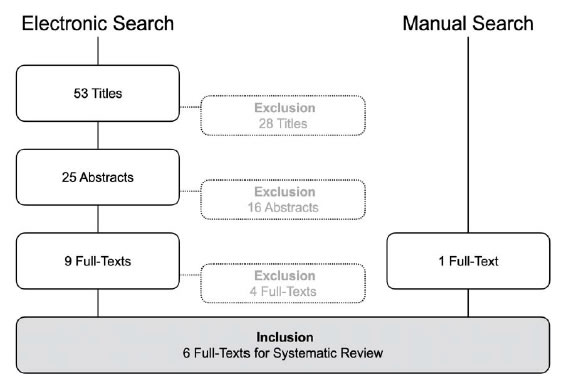
Figure 1. Systematic search strategy.
Included publications were categorized as four Narrative Reviews (Li & Meng 2020; Peng et al. 2020; Tang et al. 2020; Yang et al. 2020), one Discovery Report (Meng et al. 2020), and one Letter to the Editor (Sabino-Silva et al. 2020). Key recommendations for the management of COVID-19 infection control from each publication were summarized and tabulated along with the first author name, year of publication, and country of publication (Table 1).
|
Table 1: Data extraction for included studies (n=6). |
|||
|
Authors (year) |
Country |
Study design |
COVID-19 infection control protocol |
|
Li and Meng (2020) [11] |
China |
Narrative Review |
• Use of effective and strict disinfection measures in both clinical settings and public area. |
|
Meng et al. (2020) [12] |
China |
Discovery Report |
• Dental care provider should measure the temperature of every staff and patient as a routine procedure. |
|
Peng et al. (2020) [13] |
China |
Narrative Review |
• Dental professional should be able to identify patients with suspected COVID-19 infections. |
|
Sabino-Silva et al. (2020) [14] |
Canada/ Brazil |
Letter to the Editor |
• It is crucial for dentists to refine preventive strategies to avoid the COVID-19 infection by focusing on patient placement, hand hygiene, all personal protective equipment (PPE), and caution in performing aerosol-generating procedures. |
|
Tang et al. (2020) [15] |
China |
Narrative Review |
• Dental professionals play great role in preventing the transmission of COVID-19 by following infection control measures during dental practice to block the person-to-person transmission routes. |
|
Yang et al. (2020) [16] |
China |
Narrative Review |
• Use of and strict personal disinfection of maxillofacial professionals in a huge hospital. • Responsible handling of infectious consumables and sterilization of contaminated instruments. |
Discussion
COVID-19 is a newly identified respiratory disease. The first case can be tracked back to 17 November 2019, according to Chinese government data [17]. Therefore, this systematic PubMed search was limited to publications reporting on infections caused by SARS-CoV-2 that were published after 1 November 2019. Publications focused on other SARS-related diseases were excluded.
Considering the recent and rapid development of the COVID-19 outbreak, it was not surprising that the identified publications from the systematic search were not clinical studies, but rather reports on self-learned experiences and trial and error management, mainly from research groups in China (five publications out of six) [11-16]. As COVID-19 continues to spread globally, it is assumed that confirmatory and/or new recommendations, and retrospective analyses of the effectiveness of different infection control protocols, will continue to be published from Europe and then from the USA [1,6,13].
The oral healthcare sector in particular has been hit hard by COVID-19 [12]. Confusion prevails due to the flood of information from policy stakeholders, statements from national dental associations, and press releases, accompanied by various (fake) posts on social media [17-21]. What infection control protocols should dental care provider follow during the COVID-19 crisis? And what lessons can the dental society learn from the COVID-19 pandemic to guide the precautions and preventative measures that may be required for future infectious diseases?
Based on the findings of this systematic review [11-16] and involving the expertise and experience of colleagues at the University Center for Dental Medicine in Basel (UZB), Switzerland, an evidence- based guideline was developed (Figure 2). This guideline was implemented on 2020/03/31 and will be reviewed and updated as new information on the COVID-19 outbreak comes to light. This guideline considers both the external and the internal dental ecosystems. On the one hand, the institutional infrastructures of dental care providers must be differentiated from an external point of view: i) Single Offices;Clinical Centers; and iii) Dental Hospitals with/without University setting including under- and postgraduate education, and clinical trials with voluntary participants and patients under dental treatment. On the other hand, possible routes of microbial transmission within the dental environment must be analyzed internally: i) dental and oral diagnostics including maxillofacial radiology and in particular aerosol-producing treatments; ii) patient flows plus accompanying relatives in waiting areas, restrooms and toilet facilities; as well as iii) employees’ facility rooms of daily use.
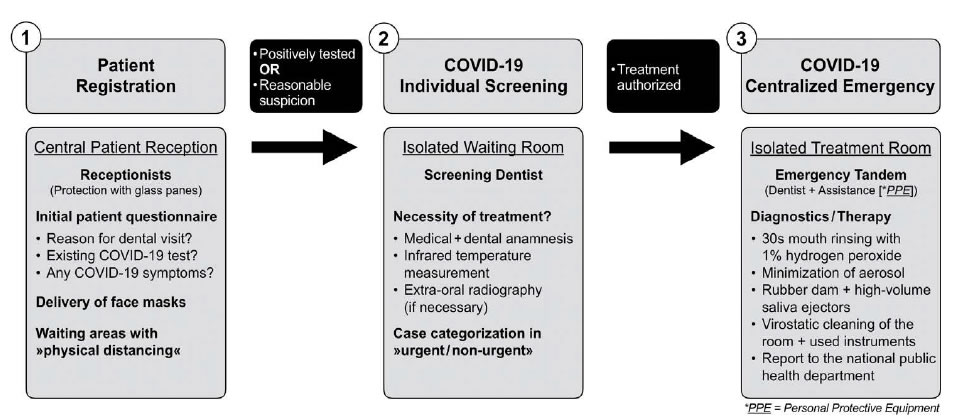
Figure 2. Patient flow in a centralized setting of a Dental Hospital.
In common with the rest of society, “physical distancing” is the top priority. In this context, the catchment radius of potential patients and dental staff must be taken into account for the decision who should maintain the dental care mandate during a crisis. Reducing the number of employees needed to deliver emergency dental treatments is the ultimate goal to reduce contact between people and diminish the risk of viral spreading. This will also help to preserve the supply of personal protective equipment for the protection of the high-risk group of dental care providers. Moreover, the range of dental treatments that will be delivered during the pandemic should be transparently communicated to both the dental society and to patients.
Centralization of dental emergency treatments in regional Dental Hospital settings is the key for maintain dental healthcare standards during pandemic crisis. In contrast to primary healthcare, dental procedures are usually elective. All non-urgent dental treatments must be postponed. Supplies of personal protective equipment needed by clinical staff who are treating critically ill patients in General Hospitals are critically low. If all dental care providers store and use these items for non-urgent treatments, frontline healthcare workers will be left unprotected. In case of COVID-19, it is not possible to reliably identify patients who are asymptomatically infected and most of the dental treatments produce aerosols that is known to increase exposure potential if patients are infected.
We recommend that dental care providers should focus on the management of conditions that require immediate attention to relieve severe pain and/or risk of infection and to alleviate the burden on hospital emergency departments. These comprise:
• Severe dental pain from pulpal inflammation;
• Acute exacerbation of chronic apical periodontitis;
• Acute necrotizing ulcerative gingivitis or periodontitis;
• Painful mucosal changes;
• Pericoronitis of third molars;
• Post-operative osteitis and dry-socket phenomenon;
• Infections with intra-/extra-oral swelling or abscess, particularly those potentially compromising the patient’s airway;
• Facial and/or dental trauma with avulsion, dislocation and/ or fracture;
• Uncontrolled bleeding;
• Dental treatment required prior to critical medical procedures;
• Fixation or removal of broken prosthodontic or orthodontic appliances to avoid injuries or foreign body aspiration.
If dental diagnostics and/or treatments cannot be delayed and have to be carried out related to the above list of indications, strict adherence to the hygiene chain is mandatory. In addition to the routine patient history, contactless temperature measurement using infrared thermometers should now be employed as an initial step to identify patients who are potentially infected with SARS-CoV-2.
For essential emergency treatment of patients with confirmed COVID-19, or patients with a strong suspicion of an acute infection, the following protocol should be applied by the dental care providers:
• Patients should wear masks in public and in the hospital setting;
• Patients with suspected or confirmed infection should wait in separate rooms and use indicated rest-rooms;
• Dental treatment should be conducted in an isolated and well- ventilated room (100% fresh air supply of the ventilation or air condition system instead of recirculating air is pursued);
• Use of personal protective equipment is mandatory, comprising respirators for filtering inspired air, face masks and goggles, double-layered gloves, and protective clothing, including safe disposal of used consumables;
• Patients should use pre-operative antimicrobial mouth rinse with 1% hydrogen peroxide for 30 seconds (peroxide dissolves the virus protein);
• Extra-oral dental radiographs can be used as alternatives to intra-oral imaging during the outbreak of COVID-19 to avoid any coughing of the patients;
• Emergency treatments should be as minimally invasive as possible and reduced in length and in spread of oral fluids (rubber dam and high-volume saliva ejectors to minimize aerosol);
• Treatment rooms and other areas, and used instruments, should be cleaned with appropriate virostatic agents;
• The number of dental care providers in the facility should be limited; and staff should work in weekly shifts and should be separated from household family members if they are at risk;
• Tele-healthcare should be used (whenever possible).
In addition, human resource management should consider different scenarios for work deployment plans in the Dental Hospital settings during the crisis. Tandems consisting of one dentist and one dental assistant should work together in blocks of weekly shifts to reduce interactions with other colleagues and the risk of infection. If a member of a team becomes infected, or an infection is suspected, the team should be replaced by a new tandem. Those dental personnel who have previously been infected with SARS-CoV-2, and have evidence of immunity in the form of antibodies to the virus, could take over the emergency treatments to protect the susceptible colleagues. Moreover, it must be considered whether routine testing of the dental staff should or could be carried out to clarify the infectious status of the staff in order to help prevent further transmission of the virus.
Conclusion
What lessons can dental stakeholders learn from the current COVID- 19 pandemic?
The dental profession and its special environment pose high risk of viral spreading and cross infections between patients and dental care providers. Strict adherence to the hygiene chain is a prerequisite for the control of further transmission. Dental treatment must be limited to emergencies during the pandemic. Positively tested patients or symptomatic patients with a strong suspicion of an acute infection must be treated under personal protective conditions of the dental professionals. Any aerosol-producing therapy must be reduced to a minimum.
After the successful fight against the pandemic, international standards need to be defined by a task force with experts from the public health sector, health economists, and politicians, in order to develop standard operating procedures for quickly coordinating and coping with future public health emergencies. Dental treatments are usually elective procedures. During a pandemic, it is important to establish regional dental emergency centers as quickly as possible to provide the necessary capacities for society and to ensure appropriate hygiene standards. Personal protective equipment must be used for dental emergencies of infectious patients and in a resource-saving manner.
Author Contributions
Conceptualization, Methodology, Writing-Original Draft, Writing-Review and Editing, Supervision and Project Administration:
T.J. and N.U.Z.; both authors have read and agreed to the published version of the manuscript.
Declaration of Interests
The authors declare no conflict of interest.
Acknowledgements
The authors express their gratitude to Mr. James Ashman for proofreading the final manuscript. This research received no external funding.
References
- Tuite AR, FismanDN(2020) Reporting, Epidemic Growth, and Reproduction Numbers for the 2019 Novel Coronavirus (2019-nCoV) Epidemic. Ann Intern Med,[Crossref]
- Cheng, ZJ,ShanJ (2020) 2019 Novel coronavirus: where we are and what we know. Infection, [Crossref]
- Habibzadeh P,StonemanEK (2020)The Novel Coronavirus: A Bird’s Eye View. Int J Occup Environ Med, 11(2): 65-71. [Crossref]
- Hui DS(2020)The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health – The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis, 91: 264-266. [Crossref]
- Dey SK(2020) Analyzing the epidemiological outbreak of COVID-19: A visual exploratory data analysis approach. J Med Virol, [Crossref]
- Wu, JT, LeungK, LeungGM(2020) Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet, 395(10225): 689-697. [Crossref]
- Yang W(2020) Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19):A multi-center study in Wenzhou city, Zhejiang, China. J Infect, 80(4): 388-393. [Crossref]
- Zhou F(2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet, [Crossref]
- Gamio L (2020)The workers who face the greatest coronavirus risk. The New York Times,
- Moher D(2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med, 6(7):e1000097. [Crossref]
- Li ZY,MengLY (2020) [The prevention and control of a new coronavirus infection in department of stomatology]. Zhonghua Kou Qiang Yi XueZaZhi, 55(0): E001. [Crossref]
- Meng L,Hua F,BianZ (2020) Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res. [Crossref]
- Peng X(2020) Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci, 12(1): 9. [Crossref]
- Sabino-Silva R,JardimACG, SiqueiraWL (2020) Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin Oral Investig,
- Tang, HS, YaoZQ,WangWM (2020) [Emergency management of prevention and control of novel coronavirus pneumonia in departments of stomatology]. Zhonghua Kou Qiang Yi XueZaZhi, 55(0): E002. [Crossref]
- Yang Y(2020) Experience of Diagnosing and Managing Patients in Oral Maxillofacial Surgery during the Prevention and Control Period of the New Coronavirus Pneumonia. Chin J Dent Res, 23(1):57-62. [Crossref]
- Davidson H (2020) First Covid-19 case happened in November, China government records show. Guardian Weekly,
- COVID-19 Infection Control Protocols and Procedures. 2020; Available from: https://www.ada.org/en/member-center/coronavirus-resource-toolkit-for-ada-members/covid-19-infection-control-protocols-and-procedures-webinar?utm_source=adaorg&utm_medium=vanityurl&utm_content=safety&utm_campaign=covid-19.
- Zhejiang University School of Medicine C, Handbook of COVID-19 Prevention and Treatment. 2020.
- Coronavirus disease (COVID-19) Pandemic. 2020; Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- Dossier: AktuelleInformationenzum Coronavirus. 2020; Available from: https://www.sso.ch/home/coronavirus.html.