DOI: 10.31038/IDT.2023413
Abstract
Background: Malaria is a potentially fatal disease caused by parasites transmitted by the bites of infected female Anopheles mosquitoes. It is a preventable and curable disease. Thus, the use of insecticide-treated mosquito nets is a means of combating malaria. In this context, this study assessed the positivity rate of strawberry drops at the St Vincent de Paul hospital in Zogbo and the physical integrity of mosquito nets used by the population in the same locality.
Methods: In order to determine the prevalence of malaria in the Saint Vincent de Paul hospital in Zogbo, we took venous and capillary samples from patients for thick blood tests from 31 May to 19 August 2022. We then interviewed 216 households including 100 positive patients in the Zogbo district in southern Benin over a period from 8 July to 19 August on the physical condition of the nets (torn, sewn, tied, frequency of washing, drying method, etc.) in order to assess their physical integrity.
Results: Out of 863 thick drops performed, 686 were positive, representing a positivity rate of 79.49%. The household surveys revealed that the majority of respondents were uneducated married women. Indeed, all households own at least one long-lasting insecticide-treated net of three different brands, namely Dawa net and Olyset net in particular and Permanet 2 and 3. However, all the nets observed were either with holes, tied in several places, loosely tied or sewn in several places. In addition, most households washed their nets three times in three months, a percentage of 66.20%, and 100% of households dried their nets in the sun.
Conclusion: This study showed that there is a high prevalence of malaria at St Vincent de Paul Hospital, which is due to the loss of physical integrity of the nets. In addition to industry- prescribed recommendations to reduce malaria mortality and morbidity in endemic areas.
Keywords
Prevalence, Malaria, Physical integrity, Mosquito nets, Zogbo
Introduction
Malaria is a potentially fatal disease caused by parasites transmitted by the bites of infected female Anopheles mosquitoes. It is a preventable disease that can be cured. According to the WHO, in 2020, there will be an estimated 241 million cases of malaria worldwide. The WHO African Region bears a large and disproportionate share of the global malaria burden. In 2020, 95% of malaria cases and 96% of malaria deaths were recorded in this region. (WHO: Annual Malaria Report 2020) [1]. In Benin, malaria is the leading cause of hospitalization and treatment. According to the Sanitary Statistics Yearbook generated by the National Health Management Information System of the Ministry of Health for the year 2020 [2], malaria represents 44.2% and 49.5% of the reasons for consultation in the general population and in children under five years of age respectively. The parasite responsible for malaria infection in Benin is a protozoan belonging to the genus Plasmodium mainly transmitted by the Anopheles gambiae s.l complex, Anopheles funestus and Anopheles nili groups [3]. In Benin, the main means of vector control relies essentially on the use of Long-Acting Insecticide-Treated Nets (LLINs). Much effort has been made over the last decade in many African countries to increase the accessibility of LLINs to the population, particularly to children under five years of age and pregnant women. (Yadouleton et al.). Unfortunately, significant challenges remain jeopardizing the goals and sustainability of the achievements. (Raphael Kelani et al. International Journal of) [4]. Indeed, many of the LLINs distributed become ineffective after two months of use due to the appearance of large holes resulting in the total tear of the net (Toe et al. 2009). In addition, the effectiveness of LLINs decreases with fewer washes, resulting in a progressive loss of the chemical barrier role of these LLINs (Curtis C.F 2008) [4]. However, these LLINs are supposed to maintain their effective biological action without further treatment after at least 20 washes and after three years of use. (Seck et al. 2008) and (Curtis C.F 2003) [5]. This is the context of the present study, which will allow us to evaluate the positivity rate of the Thick Drops at the St Vincent de Paul clinic in Zogbo and the physical integrity of the nets used by the population.
Materials and Methods
Framework of the Study
Our study was located in the Zogbo quarter, which is situated in the 9th arrondissement of Cotonou in the littoral department. It is located near Fifadji, and northwest of Houenoussou-Sainte Rita.The present study is a descriptive cross-sectional study based on a qualitative questionnaire that was carried out during the months of June, July and August 2022 and on direct observations of the slides of Thick Drops of the patients of the Saint Vincent de Paul clinic.
Sampling
Our study population consisted of 155 persons suspected of having malaria (fever with or without other symptoms) with no distinction of age or sex. Thus, patients who visited the laboratory of the St Vincent de Paul clinic for a thick drop/blood smear examination during the study period, residing in Zogbo and having at least one mosquito net used as a means of malaria control were included in the study. The size of the representative sample was calculated using the following formula for frequency calculation.
![]()
P: prevalence of malaria in the general population; P=17%.
Z: target confidence level; Z=1.96.
I: acceptable margin of error or precision; I=5%.
N: size of the representative sample.
Using this formula, our sample size N=216 (205-158) patients.
116 households were randomly selected in Zogbo and 100 households of patients at the St.
Vincent de Paul clinic who tested positive or negative for EW/DP were also considered.
Biological Materials
The biological material used was blood. An Olympus® CX31 light microscope (Olympus, Grenchen, Switzerland) was used to read Giemsa-stained slides (Cypress Diagnostics, Hulshout, Belgium).
Data Collection
In the Zogbo neighborhood, households were randomly selected and nets were examined in each household. A total of 216 nets were collected from the households. After the consent of the head of the household, a questionnaire on the origin, date of obtaining, use and maintenance of the nets was given to the head of the household or to a member of the household who was at least 18 years old. The data were collected using a questionnaire designed for this purpose. The questionnaire collected information on socio-demographic characteristics (age, sex, marital status, occupation, religion and place of residence), frequency of use of LLINs and brand.
Physical Integrity Assessment
The number, size, and location of tears on each side of the net and on the roof were determined for each sample (26). Three categories of holes (0.5 cm ≤ size 1 ≤ 2 cm; 2 cm < size 2 ≤ 10 cm; 10 cm < size 3) previously defined by Kilian et al. were retained during this study.
Analysis of Blood Samples
We proceeded to a blood sampling on EDTA tube and then we made a thick drop and a blood smear on a slide. The slides were then dried, fixed and stained with Giemsa (Cypress Diagnostics, Hulshout, Belgium) diluted 1:10 for 10 minutes. The reading was done with an Olympus® CX31 light microscope (Olympus, Grenchen, Switzerland) at the X100 objective with a drop of immersion oil. If a parasite is identified in the microscopic field, the result is positive. If, on the contrary, no parasite is found after 100 microscopic fields, the examination is considered negative.
Statistical Analysis
A questionnaire form was designed on the Odk Collect software. The data entry as well as their processing and analysis were done on the software Excel version.2019. The frequency of modalities for each variable was expressed.
Results
Prevalence of Malaria at the Saint Vincent de Paul Clinic during the Months of June, July and August
The Figure 1 presents the prevalence of malaria at the Saint Vincent de Paul clinic during the months of June, July and August. In total, out of 863 EWTs performed, 686 were positive or a percentage of 79.49% and 177 were negative or a percentage of 20.51%. The result of these analyses is that the prevalence of malaria is 79.49%.
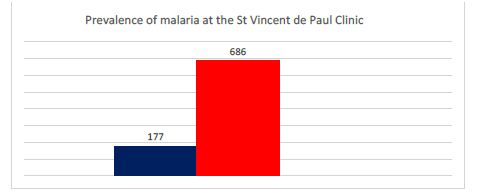
Figure 1: Prevalence of malaria at the Avé Maria hospital in Agla
Socio-demographic Characteristics
Our study was made up of 75% of women with a sex ratio (F/H) of 3. 75.93% were married at the expense of single people. The vast majority of respondents were uneducated (63.89%) and of Christian faith (81.02%). Table 1 presents the frequencies of the socio-demographic characteristics of the respondents.
Table 1: Socio-demographic parameters of patients
|
Modalities |
Effectifs (n) |
Frequency (%) |
|
| Sex | Female |
162 |
75% |
| Male |
54 |
25% |
|
| Marital Status | Single |
52 |
24,07% |
| Married |
164 |
75,93% |
|
| Religion | Christian |
175 |
81,02% |
| Muslim |
41 |
18,98% |
|
| Education level | Primary |
30 |
13,89% |
| Secondary |
22 |
10,19% |
|
| Superior |
26 |
12,03% |
|
| Not instructed |
138 |
63,89% |
|
| Total |
216 |
100 |
Prevalence of Malaria in the Surveyed Population
Figure 2 shows the prevalence of malaria in the survey population. A total of 80 patients tested positive versus 20 patients who tested negative, for a malaria prevalence of 80%.
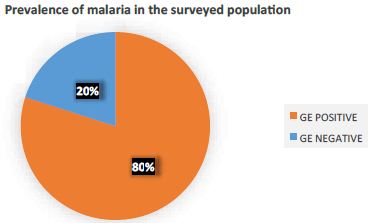
Figure 2: Prevalence of malaria in the surveyed population
Prevalence of Malaria in the Surveyed Population by Age and Sex
Table 2 presents the evaluation of malaria prevalence according to age and sex. Its analysis reveals that the most represented age group is (0-5) with a proportion of 90.6% and the most represented sex is female with a proportion of 88.9%.
Table 2: Prevalence of malaria by sex and age
|
Effectifs |
Number of positives |
Percentages |
||
| Ages of patients | [0-5] |
32 |
29 |
90,6% |
| [5-15] |
21 |
18 |
85,7% |
|
| [15-25] |
23 |
17 |
74% |
|
| [25-35] |
14 |
10 |
71,4% |
|
| ≥35 |
10 |
6 |
60% |
|
| Sex | Female |
69 |
61 |
88.9% |
| Male |
31 |
19 |
61,2% |
|
Evaluation of Parasite Densities
Table 3 shows the parasite densities of the patients. Patients with a parasite density less than or equal to 5000 Parasites/µL of blood were the most represented with a percentage of 70%. 8% and 2% have respectively their PD lower or equal to 1000 and higher than 1000 Parasites/µL.
Table 3: Evaluation of parasite densities
|
Parasite densities Parasites/µL |
Effectifs |
Percentage |
| ≤5000 |
70 |
70% |
| ≤10000 |
08 |
8% |
| >10000 |
02 |
2% |
Frequency of Use of LLINs
Figure 3 presents the frequency of LLINs use by the population of Zogbo. Of the 216 respondents, 116 people sleep under LLINs quite often, a percentage of 53%, compared to 101 people who rarely sleep under an LLINs, a percentage of 47%.
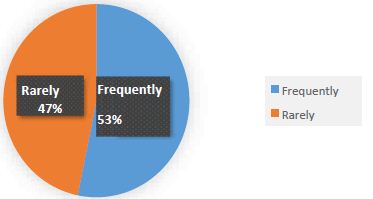
Figure 3: Frequency of LLINs use by the population of Zogbo Brands of nets used in the Zogbo area
Figure 4 below shows the different brands of nets used in the Zogbo neighborhood. After analysis of this graph, it appears that the DAWA net brand is the most used by the population 56.94%, followed by OLYSET net 29.17%, and the least used by the population permanet 2, 13.43% and permanet 3, 0.46%.
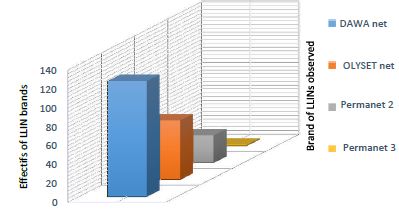
Figure 4: Different types of LLINs used by households in Zogbo
Frequency of Net Washing in Zogbo (Washing in 03 Months)
Figure 5 presents the number of times nets are washed in three months by households. The analysis shows that out of 216 households, 47 wash their nets twice in three months, 143 wash their nets three times in three months, 9 wash their nets four times in three months, and 17 wash their nets six times in three months.
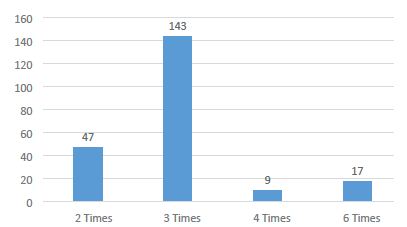
Figure 5: Frequency of net washing in three months
Physical Conditions of LLINs in Use in Surveyed Households
Table 4 presents the physical conditions of LLINs in use in the 216 households surveyed. Its analysis reveals that the population uses 90.74% of LLINs with holes of sizes T1, T2, T3 and T4.
Table 4: Physical conditions of LLINs in use in surveyed households
|
MIILDs without holes |
LLINs with holes |
Total LLINs with holes |
% LLINs with holes |
|||
|
T1 |
T2 |
T3 |
T4 |
|||
|
20 |
80 |
74 |
33 |
09 |
196 |
90,74 % |
Table 5 presents the physical conditions of LLINs being used in the patients surveyed who performed the GEs. Its analysis reveals that 80% of LLINs with holes of sizes T1, T2, T3 and T4 are used by patients whose Thick Drop is positive and the 20% of LLINs without holes are used by patients whose Thick Drop is negative. It is therefore inferred that the positivity rate of the Thick Drops is closely related to the physical conditions of the nets used.
Table 5: Physical conditions of LLINs in use in surveyed patients who performed GE
|
MIILDs without holes |
LLINs with holes |
Total LLINs with holes |
% LLINs with holes |
||||
|
T1 |
T2 |
T3 |
T4 |
||||
| Patients positifs |
00 |
55 |
38 |
10 |
07 |
80 |
80% |
| Patients négatifs |
20 |
00 |
00 |
00 |
00 |
00 |
00% |
Discussion
In the context of malaria control, prevention of mosquito bites is a crucial step not only to protect but also to control the vectors of the disease. The general objective of this study is to evaluate the positivity rate of thick drops at the St. Vincent de Paul clinic in Zogbo and the physical integrity of the nets used by the population. This study focused on an urban area of Benin. During the three months, we observed a 79.49% positivity rate for thick drops. However, out of the 100 blood samples taken from patients who were surveyed, 80% of positive cases were recorded and the most represented age group was 0 to 5 years, i.e. a percentage of 90.6%. These results are similar to those of Tokponnon et al. [6] who found a prevalence of 32% in children under 5 years of age in four hospitals in the Plateau department in 2022, taking into account the study population. The effectiveness of LLINs has been widely demonstrated over the past two decades as a vector control measure against malaria (Lindblade et al. 2005 [7]; Killian et al. 2008). This effectiveness of LLINs has been made possible by the physical and chemical barriers they provide. However, brand, conditions of use and maintenance are factors that can affect the physical integrity and biological efficacy of LLINs. During our study, three brands of LLINs (DAWA net, OLYSET net and Permanet 2 or 3) were identified in the Zogbo area. The brands DAWA net and OLYSET net were more frequently found in the households surveyed, respectively a percentage of 56.94% and 29.17%. Our study showed that this difference was due to chance, as the population itself could not recognize the difference between the different brands. However, the work of Diouf et al. 2018 in Senegal showed that this difference in brands is in the acceptability, that is to say that households often tend to keep the LLINs they prefer, those less appreciated being either redistributed to other people or used for other purposes. The integrity assessment of LLINs showed that, regardless of brand, the majority of nets found in the Zogbo neighborhood were either damaged or torn. The same finding was reported in the Uganda and Chad studies, which showed that 45% to 78% of nets in operational use were damaged and only 30% were still in good condition after one year of use, respectively. The washing of LLINs three (03) times in three months by the majority of the population of the Zogbo district surveyed with products of all kinds even corrosive detergents of the populations interviewed may be involved in the ineffectiveness of the LLINs. The same logic is followed by the results of the studies of Kelani et al. 2018 which explains that the principle of low frequency of washing (once every three months) recommended by the industry as a factor of preservation of the insecticidal effect in the LLINs fibers, certainly does not seem to be possible in community settings. Indeed, the multiple washing frequencies of LLINs in community settings have often been reported by female breastfeeders who have to wash their nets every day, due to children’s urine. This perception should be taken into account by the industry when manufacturing LLINs. Insecticide-treated mosquito nets are very important in the fight against malaria, they reduce mortality and morbidity. However, they are ineffective when their physical integrity is degraded and consequently a high prevalence of malaria despite the use of nets [8-16].
Conclusion
The positivity rate of the Thick Drops at St Vincent de Paul Hospital during the months of June, July and August is 79.49%. This positivity rate is closely related to the actual use of the nets and especially to their effectiveness, which is mainly based on their physical integrity, an important indicator of their durability in households. Our research results demonstrate that the physical barrier provided by LLINs can be significantly altered during the normal course of use. The national malaria control program must therefore consider physical integrity performance under local conditions when selecting the types of LLINs to distribute.
References
- WHO: Malaria Annual Report 2020.
- Ministry of Health: Health Statistics Yearbook 2020.
- Rock Aikpon, Razaki Ossè, Renaud Govoetchan, Arthur Sovi, Frédéric Oké-agbo, et al. (2013) Entomological baseline data on malaria transmission and susceptibility of anopheles gambiae to insecticides in preparation for indoor residual spraying (IRS) in attacora, (Benin). Academic Journals 5: 102-111.
- Tokponnon Filémon, Aholoupke Bruno, Denon Eric, Gnanguenon Virgile, Bokossa Alexis, et al. (2013) Evaluation of the coverage and effective use rate of long lasting insecticide treated nets after the national scale up of their distribution in bnin. Parasites & Vectors 6. [crossref]
- Curtis CF (2003) Improving and scaling up vector control,the impact of insecticide resistance and possible means of resistance managment.in WHO /TDR, 2003, report of the scientific working group on malaria, annex 7, geneva, 71-82.
- Tokponnon TF, Ossè R, Arthur S, Wakpo A, Hounto OA, et al. (2022) Evaluation at the level of health facilities, of the protective efficacy of LLINs children under 5 years old from localities of low and high reisitance of vectors to pyrethroid inecticides in Benin in west africa, 12: 57-73.
- Kim A Lindblade, Ellen Dotson, William A Hawley, Nabie Bayoh, John Williamson, et al. (2023) Evaluation of long-lasting insecticidal mats after 2 years of household use. Trop Med and Int Hlt.
- WHO: Malaria, December 6, 2021.
- Mansiangi P, Kalonji A, Izale B, Nsiala A, Phanzu F, et al. Evaluation of the sustainability of LLINs distributed in the Democratic Republic of Congo through mass campaigns from 2011 to 2014.
- Ahogni Idelphonse, Durability and impact on Plasmodium falciparum infection and anemia in children under 5 years of age of eight types of nets in eight communes in Benin, West Africa, December 2020. (PhD thesis at the University of Abomey-calavi)
- Pryce J, Richardson M, Lengeler C (2018) Insecticide-treated nets for malaria prevention, December 6.
- Nopono FN, Enama L Offono, Tsila HG, Mbida A, Tonga C, et al. (2020) Evaluation of the efficacy of impregnated mosquito nets 36 months after their distribution in Southern Cameroon.
- Lafont Françoise (2016) Determining the sample size, October 28.
- Bambenongama Norbert Mandana (2022) Evaluation of the use of long-lasting insecticide-treated nets among pygmies in the Democratic Republic of Congo, April 30, 2022.
- Djegui (2006) Distribution of impregnated mosquito nets throughout Benin-Partners and initiators of the project consult each other, Benin, September 2006.
- Albert Kilian, Wilson Byamukama, Olivier Pigeon, Francis Atieli, Stephan Duchon et al. Long-term field performance of a polyester based long-lasting insecticidal mosquito net in rural Uganda. Malaria J 7.