DOI: 10.31038/PEP.2021232
Abstract
Background: Tanzania is implementing Infection Prevention and Control (IPC) in health care settings using Standard Based Management and Recognition model. The country has developed standards that are used to assess compliance of IPC best practices in health facilities. In order to compare country’s standards with international standards of IPC achievement, the World Health Organization checklist has been used to assess six hospitals.
Aim: To evaluate the Infection Prevention and Control compliance mean scores by using national Standard Based Management and Recognition tool and WHO’s IPC Assessment Framework at Facility Level (IPCAF – Facility tool).
Methods: A comparative cross-sectional evaluation on IPC compliance using national SBM-R tool and IPCAF Facility (WHO tool) was done in January and May 2020 respectively. We conducted evaluation in six hospitals – four regional referral hospitals (RRHs) namely Bukoba RRH, Maweni RRH, Sekou Toure RRH, Temeke RRH, and two zonal referral hospitals which are Benjamin Mkapa Hospital and Mbeya Zonal Referral Hospital.
Results: Temeke Regional Referral Hospital showed the highest infection prevention and control compliance scores with difference in scores when using SBM-R tool and IPCAF Facility WHO tool of 28 (CI 27.74-28.26) p<0.0001; while the lowest difference mean score was from Sekou Toure RRH, which was 1 (CI 0.74 – 1.26) p<0.0001.
Conclusion: There was a significant difference between the mean scores when evaluation was done using SBM-R tool and the WHO-IPCAF tool in all health care facilities. Generally the scores were average in all cases.
Key words
Infection Prevention and Control, Standards Based Management and Recognition, IPCAF Facility WHO
Background
Compliance with Infection Prevention and Control (IPC) guidelines and standards in low-and middle- income countries (LMICs) continues to be a challenge [1]. This has been attributed to inadequate resources, poor infrastructure and other contextual factors which call for more research to identify approaches that work well in LMICs [2, 3]. Gaps in knowledge of IPC implementation strategies among Nurses in sub-Saharan Africa have been reported mainly on “understanding of which, in what combination, and in what context implementation strategies should be best utilized to ensure their safety and that of their patients” [4]. Analysis of a global situation on implementation of the IPC core components at national level reveal that “most countries have IPC programmes and guidelines, but have not invested adequate resources and neither have they translated them in to implementation and monitoring [5].
The COVID-19 pandemic caused by Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) underscores the need to strengthen IPC practices [2]. Infection Prevention and Control interventions are key in preventing COVID-19 and Healthcare Associated Infections (HAIs). Such interventions include hand hygiene and other hospital- based IPC practices and approaches which are highly required in limited resource settings especially in LMICs [6]. However, a study in the Cochrane Database of Systematic Reviews [7] found variability in certainty of evidence on which approach is better for improving hand hygiene compliance between multimodal and simpler interventions, hence calling for more robust studies. In the area of hand hygiene, Tanzania has been cited as an example of countries in Africa with hand hygiene policies embedded in the IPC policies, i.e., national IPC guidelines, standards and tools [8].
Information available regarding HAIs do not portray the real situation in African countries [9]. Some studies have outlined effective measures which can be implemented in settings where resources are inadequate in order to improve IPC compliance and prevent HAIs. These include developing and implementing policies and procedures on HAIs accompanied with rigorous monitoring and feedback mechanism; and regular education and training of health care workers, patients and visitors on the policies and procedures [10]. A position statement of the International Society for Infectious Diseases in 2020 regarding surveillance of surgical site infections (SSIs) in LMICs noted that the burden of SSIs ranges from 8% to 30% of procedures making it the most common HAI. The statement gives key areas to address in preventing HAIs based on surveillance (collecting valid, high-quality data; linking HAIs to economic incapacity; implementing SSI surveillance within IPC programs; prioritizing IPC training for healthcare workers in LMICs to conduct broad-based surveillance; and developing a highly accurate and objective international system for defining SSIs, which can be translated globally in a straightforward manner) [11].
In October 2015, the world adopted “the 2030 Agenda for Sustainable Development”, in which goal 3 is on “ensuring healthy lives and promoting well-being for all at all ages” with a target (target 3.8) to “achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all” [12]. The target on universal health coverage (UHC) contains, as one of its pillars, the quality aspect which includes IPC. Through the lens of UHC and learning from the COVID-19 pandemic, Karamagi and colleagues have proposed a framework for health systems functionality towards UHC in the WHO African Region in which compliance of standard precautions for IPC is one of proxy indicators for vital sign “patient safety” in the domain “effective demand for essential services” [13]. This puts further emphasis to member states to strengthen compliance of IPC guidelines, standards and tools. Likewise, Storr, et al, (2016) worked to propose key points for building a policy case for IPC in the context of quality UHC as well as support and guidance to national governments. They also described the eight (8) WHO IPC core components [14]. The compliance to the WHO IPC core components in Tanzania in the past two decades is shown in Table 1.
Table 1: Compliance with the WHO- IPC core components in Tanzania: 2004 to 2021
| WHO IPC core component (Storr, et al, 2016) | Description of status in Tanzania: 2004-2021 |
| Organisation of IPC Programmes
|
There is a sub-unit responsible for IPC within the Health Quality Assurance Unit at the Ministry of Health, Community Development, Gender, Elderly and Children [32]; with qualified staff with clear roles and responsibilities. Funding for IPC activities comes from Development Partners, Implementing Partners and the Government of Tanzania. Startup IPC programme in 2003 was funded by the US – PEPFAR [33].
|
| Technical Guidelines
|
National IPC Guidelines were developed in 2004 (MoH, 2004) and revised in 2018 to accommodate new scientific developments and recommendations by the WHO [17]. IPC standards:hospital standards, 2012; health centre standards, 2015, and dispensary standards, 2015 were revised in 2020 [34]. IPC Communication Strategy was developed in 2012 covering a period of 2012-2017 [3]. Dissemination of the revised guidelines, standards and standard operating procedures is ongoing. |
| Human Resources Education and Training
|
Training of health care workers has been the main component which included training of Tutors in health training institutions as a way of addressing gaps in pre-service curricula. There are IPC focal persons at health facilities both at regional and council levels. Generally, in the country the ministry had coordinated building the capacity of 2544 healthcare workers on IPC countrywide. |
| Surveillance of infections and assessment of compliance with IPC practices
|
The Ministry has developed tools to conduct surveillance on Surgical Site Infection (SSI). The tools are already in use in all six health facilities and some other hospitals in the country. The Ministry is also developing Monitoring and Evaluation system for IPC in which surveillance of SSIs is part of. |
| Microbiology Laboratory
|
Tanzania is complying with the WHO’s recommendations on Antimicrobial Resistance (AMR) interventions. IPC is one of the technical working groups that aimes to address AMR in the country. AMR surveillance is done through laboratories by conducting culture and sensitivity. |
| Built Environment, Material and Equipment
|
In the Ministry, there is an Environmental Health and Sanitation Section responsible for water, sanitation and hygiene (WASH) interventions under Division for Preventive Services. There are guidelines on WASH in health care facilities [36]; and guidelines for supervision of environmental health and sanitation are in place [37]. Patient placement, isolation facilities and storage of sterile |
| Monitoring and Evaluation of programmes | Ministry of Health, through the IPC programme, has developed IPC indicator matrix and is currently developing monitoring and evaluation system whereby all health facilities will be required to report on monthly basis. |
| Multimodal Strategies | IPC programme in Tanzania employs multimodal strategies such that various modalities are used to make IPC a continuous practice and agenda in health facilities. Some of the models used are frequent training, mentorships, supervisions, posters, job aids, and SoPs |
The MoHCDGEC, in collaboration with partners reviewed the National IPC Guidelines of 2004 [15] to a new version of 2018. Also, in 2019 the MoHCDGEC reviewed the IPC standards for hospitals, 2012 [16] and updated to a new version [17] that is in line with the revised national guideline, 2018. The MoHCDGEC has also embarked into countrywide dissemination of the revised national IPC guideline (2018) to health facilities [18] in order to improve IPC practices as one of key pillars to fight threats of emerging and reemerging infectious diseases including Ebola Virus Disease (EVD) that had been affecting the neighboring country of the Democratic Republic of Congo (DRC) [19]; and the recent pandemic of coronavirus disease of 2019 (COVID-19) which is caused by severe acute respiratory Syndrome coronavirus 2 (SARS-CoV-2) that was first reported in Wuhan city of China in December 2019 [20, 21].
In Tanzania, the standard based management recognition (SBM-R) tool has been mainly used to ensure compliance of IPC standards in hospitals [16]. The SBM‐R “consists of systematic utilization of detailed performance standards for rapid and repeated assessments of health facilities, including both clinical and support systems; identification of gaps in compliance with these standards; implementation of corrective interventions; and rewarding of achievements through recognition mechanisms” [22]. Quality Improvement Teams (QITs) are responsible for overall governance of quality improvement issues in hospitals. They provide advice to the Hospital Management Team (HMT) on matters related to quality, and supervise Work Improvement Teams (WITs) in departments [23, 24].
Strengthening compliance of IPC practices in health facilities is of utmost importance in this era of increasing emerging and re-emerging infectious diseases [25, 26]. Emerging and re-emerging diseases are global threats towards human existence. In Tanzania, the trend for emerging and reemerging diseases is increasing; and this is attributed to several factors including changes in ecology, climate and human demographics. Infectious diseases which are on the rise in Tanzania include Cholera, Rift Valley Fever, Plague, Anthrax, Swine Flu, and Dengue [27]. Among the notable emergency events in the country is the Cholera epidemic of August 2015 – July 2017, in which 30,269 cases were reported with 475 deaths (CFR of 1.6%) [28].
Tanzania has been affected by COVID-19 pandemic [29], which is an ongoing crisis all over the world. Moreover, Tanzania remains to be at high risk of EVD as neighboring DRC continues to suffer from repeated outbreaks since 2018 [30]. Hence, the need to implement effective and timely IPC measures is of paramount importance [31].
Tanzania has limited capacity of healthcare staffs in responding to potential infectious disease outbreaks. Also, HAIs prevention systems have not been effectively implemented at health facility levels; and there is limited coordination and collaboration between QITs and Working Improvement Teams (WITs) in addressing HAIs and eventually emerging and re-emerging diseases [23]. Also, in Tanzania the functionality of QITs in RRHs have been demonstrated to be inadequate, which may affect implementation of quality improvement activities [24]. Improving mentorship on prevention of HAIs offers an opportunity for optimal use of the limited resources in reducing of negative impacts on animal and human health. This paper aims at documenting the experience of IPC standards compliance in six hospitals using SBM-R approach and assesses the factors that are responsible for improved functionality of QITs and WITs as well as IPC sub-committee in the hospitals.
Objectives
The overall objective of the study was to gauge compliance with infection prevention and control in six referral hospitals by using National and World Health Organization checklists.
Specifically, the objectives of the study were to:
- Determine compliance score of IPC Standards using national IPC standards checklist in six referral hospitals;
- Determine compliance score of IPC Standards using WHO’s IPCAF- tool) in six referral hospitals; and
- Compare compliance scores between national IPC standards tool and WHO’s IPCAF- tool in six referral hospitals.
Hypothesis
It was hypothesized that mentorship would improve compliance with IPC standards and measures through: (1) strengthening the functionality of quality governance structures (QITs and WITs) by providing members with opportunity for more hands-on practice; (2) building capacity of frontline workers in various departments and wards; and (3) clarification of challenging issues observed during assessments and observations in the service areas. Conceptual framework in the implementation of IPC activities in Tanzania is shown in figure 1.
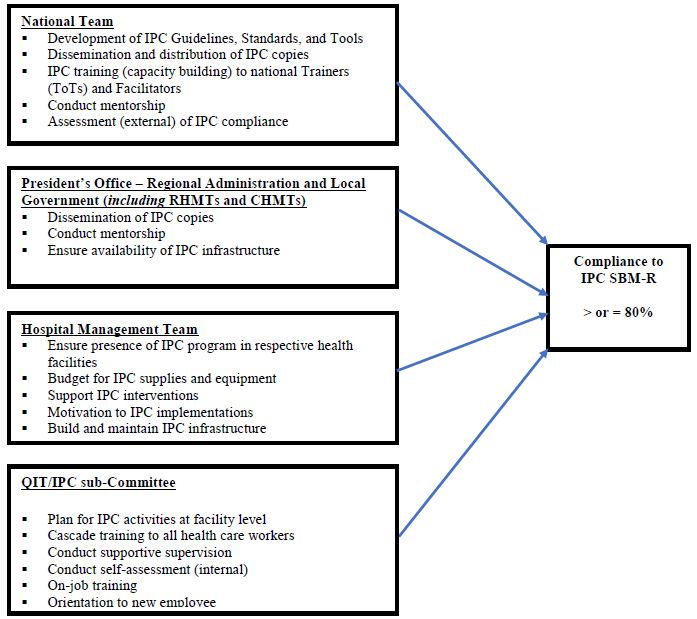
Figure 1: Conceptual framework in implementation of IPC activities in Tanzania (Credit: Bahegwa, R. P. (2021))
Methodology
Study design: A comparative cross-sectional study on IPC compliance using SBM-R tool and IPCAF – Facility WHO tool.
The national SBM-R tool has been used in Tanzania for assessment of IPC [38]. It is structured based on the functional areas within the health care facility like operating theatre, labour ward, etc. The checklist captures all standard and transmission-based precautions of IPC in all functional areas. Each functional area can score a maximum of hundred percent (100%). At the end the facility is assigned average score of all functional areas. The scores assigned are interpreted as follows: 0%-49%-poor: the facility needs a lot of work to improve; 50%-79%-moderate: needs to improve at some areas; and 80%-100%- acceptable and more investment is needed to sustain the compliance.
The IPCAF – Facility WHO tool was tested using a robust global study (in 46 countries, 181 hospitals and 324 individuals) and revised as necessary and then approved as an effective tool for IPC improvement in healthcare facilities [39]. The assessment of the facility through the use of IPCAF – Facility WHO tool focuses on eight (8) main core components of the IPC namely the IPC programme; IPC guidelines; IPC education and training; HAI surveillance; Multimodal strategies; Monitoring/audits of IPC practices and feedback; Workload, staffing and bed occupancy; and Built environment, materials and equipment for IPC at the facility level) which are then addressed by a total of 81 indicators. These indicators are based on evidence and expert consensus and have been framed as questions with defined answers to provide an orientation for assessment. Based on the overall score achieved in the eight sections, the facility is assigned to one of four levels of IPC promotion and practice: Inadequate (0-200): IPC core components implementation is deficient. Basic, (201-400): Significant improvement is required, some aspects of the IPC core components are in place, but not sufficiently implemented. Further improvement is required. Intermediate (401-600): Most aspects of the IPC core components are appropriately implemented. The facility should continue to improve the scope and quality of implementation and focus on the development of long-term plans to sustain and further promote the existing IPC programme activities. Advanced (601-800): The IPC core components are fully implemented according to the WHO recommendations and appropriate to the needs of the facility.
The assessment using SBM-R tool was conducted in January 2020 and the assessment using WHO’s IPCAF-Facility tool was done in May 2020. Prospective documentation of IPC compliance in the six hospitals – four regional referral hospitals (RRHs) namely Bukoba RRH, Maweni RRH, Sekou Toure RRH, Temeke RRH, and two zonal referral hospitals which are Benjamin Mkapa Hospital and Mbeya Zonal Referral Hospital, was done from January to May 2020.
Target population: All operating referral health care facilities in the country (regional, zonal and national hospitals) regardless of their ownership, i.e. public or private.
Study population: Prospective documentation of IPC implementation in the six hospitals –Bukoba RRH, Maweni RRH, Sekou Toure RRH, Temeke RRH, Benjamin Mkapa Hospital and Mbeya Zonal Referral Hospital, was done. The Assessment using SBM-R tool in those hospitals was followed by implementation of developed action plans by Hospital’s QIT through an IPC Focal Person who chairs an IPC sub-committee that reports to QIT.
Assessment by using the IPCAF – Facility WHO Tool was done in May 2020, as part of efforts to institutionalize IPC skills among the hospital’s IPC sub-committee to oversee IPC implementation. Also, the QITs conducted IPC assessment in the hospital on quarterly basis and the WITs in each department (functional area) conducted assessment in their functional area on monthly basis as part of SBM-R implementation in the respective hospital. In between the assessments, there have been mentorship visit in which IPC standards implementation was assessed using the IPC Hospital Standards Assessment Tool. The mentors worked as facilitators to the QITs, WITs and IPC sub-Committees in helping them to get hands-on knowledge and skills on IPC standards, standard operating procedures, as well as scoring using the tools; which ultimately helped the members of the teams to become champions. Also, qualitative information on the functionality of the QIT, WITs, IPC sub-Committee, as well as Hospital Management Team support to and commitment to IPC practices strengthening was documented, to help understand about possibility of sustaining the teams’ performance [24].
In order to ensure that decisions for strengthening IPC practices both at the facility as well as at national coordination levels are guided by the data collected, both mentors and the QITs and WITs emphasized on the importance of ensuring data quality [40].
Data management and analysis
Data was cleaned and checked for completeness and outliers before analysis. The established scores for compliance of IPC Standards were tested for normality by using the Shapiro Wilk test. We used Wilcoxon Signed-Ranks test for related samples to determine whether there was mean score differences between assessment done using national SBM-R tool and assessment done using IPCAF– Facility WHO Tool [41].
Descriptive statistics, tables and charts were used to summarize the data. Comparison between compliance mean scores between assessments done using the SBM-R tool and IPCAF- Facility WHO Tool were tested by T test; results were considered significant at p < 0.05.
Results
Compliance score of IPC Standards using national IPC standards checklist and IPCAF-Facility WHO tools.
The IPC compliance using the national Tool has revealed 2(33.34%) out of six hospitals had poor compliance of IPC best practices. The remaining 4(66.66%) had moderate compliance. No facility achieved the excellent level; the maximum score of health facilities by using national tool was moderate. Upon using the IPCAF – Facility WHO tool, three hospitals (50.00%) were found to meet the basic compliance level; while two hospitals (33.34%) were on intermediate level and one hospital (16.67%) met the advanced compliance level. The details are shown in figure 2 and table 2 below.
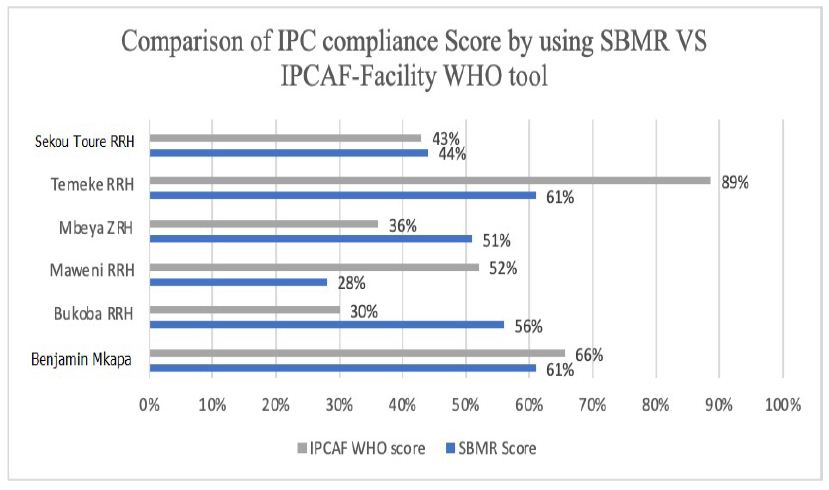
Figure 2: Scores of IPC compliance using national IPC SBM-R tool and IPCAF – Facility WHO tool
Table 2: Scores of IPC compliance using national IPC SBM-R tool and IPCAF – Facility WHO tool
| SN | Health Facility | Score of IPC assessment using Hospital IPC SBM-R standards (TZ) 20-24 January 2020 | Score of IPC Assessment by using IPCAF -Facility WHO Tool) 18 – 23 May 2020 |
| 1 | Bukoba RRH | 56% (Moderate) | 30% (Basic) |
| 2 | Maweni RRH | 28% (Poor) | 52% (Intermediate) |
| 3 | Sekou Toure RRH | 44% (Poor) | 43% (Basic) |
| 4 | Temeke RRH | 61% (Moderate) | 89% (Advanced) |
| 5 | Benjamin Mkapa ZRH | 61%(Moderate) | 66% (Intermediate) |
| 6 | Mbeya ZRH | 51%(Moderate) | 36% (Basic) |
ZRH = Zonal Referral Hospital
Comparison of compliance scores between national IPC standards tool and IPCAF-Facility WHO tool
There was a significant difference between the mean scores done by using national SBM-R tool and IPCAF – Facility WHO tool in all facilities. The details are shown in table 3.
Table 3: Comparison of scores of IPC compliance using national IPC SBM-R tool and IPCAF – Facility WHO tool
| Health Facility | Scores when using IPC SBM-R tool | Score while Using IPCAP WHO tool | Difference Score | 95% Confidence Interval | P-Value |
| Bukoba RRH | 56% | 30% | 26 | 24.74-26.26 | P < 0.0001 |
| Maweni RRH | 28% | 52% | 24 | 23.74-24.26 | P < 0.0001 |
| Sekou Toure RRH | 44% | 43% | 1 | 0.74 – 1.1.26 | P < 0.0001 |
| Temeke RRH | 61% | 89% | 28 | 27.74 – 28.26 | P < 0.0001 |
| Benjamin Mkapa Hospital | 61% | 66% | 5 | 4.74%-5.26 | P < 0.0001 |
| Mbeya Zonal Referral Hospital | 51% | 36% | 15 | 14.74-15.26 | P < 0.0001 |
Discussion
General outcome based on both national SBM-R and the IPCAF for facility-WHO tools
Assessment of IPC practices is key to monitor compliance, provide recommendations and hence improve quality of health care services delivery. Our assessments have delivered valuable insights into the state of art on implementation of key IPC structures and processes in Tanzania. Overall, the data gathered demonstrated that IPC is generally at a moderate level as demonstrated from the national SBM-R and IPCAF-Facility WHO tools. However, the use of IPCAF-Facility WHO tool in some areas revealed presence of all score levels: basic, poor and advanced.
Generally moderate level of IPC implementation was expected by both tools, as Tanzania is classified among the lower middle-income countries according to the World Bank classification. Even though, a considerable low number of participating hospitals which were only six (6), four 66.67% were allocated to merely an “intermediate/moderate” IPC level. This rather surprising finding could either be explained by a very strict interpretation of both National and IPCAF tools.
Besides the differences observed among the six participating referral hospitals in Tanzania with regard to the overall national and IPCAF tool scores, we noticed pronounced differences between facility scores of the respective national and IPCAF sections. Scores for Temeke RRH and Benjamin Mkapa were generally high as gauged by both tools. However, specific questions focusing on low scores of IPC compliance revealed mixed results. Maweni RRH scored low by using national SBM-R tool while Bukoba RRH scored low when using IPCAF -Facility tool.
Outcome based on the national SBM-R tool
The national SBM-R tool, which was structured based on standard and transmission-based precautions, was used to assess the following areas: hand hygiene; decontamination; safe waste management; safe handling of sharps; use of PPE; consider every person is potentially infectious and has risk to succumb infection;
These six hospitals did not consider every person (patient/clients or staff) as potentially infectious and susceptible to infection, hence the health care workers considered only those with clinical features as infectious. That was a risk not only to the healthcare workers but also to other patients/clients, community and the environment.
In healthcare settings, healthcare workers are required to use appropriate hand hygiene techniques. In these six facilities the critical moments to practice hand hygiene was not complied as per the requirement of WHO and the MoHCDGEC [42]. This finding compares with the study in Ethiopia which found that only 14.9% of health care providers in Central Gondar zone public primary hospitals, Northwest Ethiopia, had good hand hygiene compliance [43].
In addition to hand hygiene, healthcare workers are required to wear appropriate Personal Protective Equipment (PPE) whenever they provide healthcare services. However, in all the six hospitals visited, adherence was very low. This assessment is in-line with the study by Okello, et al (2017) which was conducted at St. Mary’s Hospital Lacor in Northern Uganda which found that 2% of healthcare workers do not know the purpose of PPE, 23.7% do not know how to don and doff PPEs, 13.6% do not use PPE even when indicated and 10% are not using an appropriate PPE [44].
In terms of management of sharps. healthcare workers in all the six hospitals visited were compliant in handling sharps appropriately. This includes use of sharps only once, avoiding recapping, and safe disposal in the sharp boxes. A study by Tariku, et al (2016) at Gondar University Comprehensive Specialized Hospital, Northwest Ethiopia found that 76.4% never bent needles with hands, 54.3% avoided removing used needles from disposable syringes, 87.2% placed used sharps in puncture-resistant container at point of use and 58.7% never recapped needles [45]. Handling of waste was low in all six facilities which were similar with the findings found at Gondar University Comprehensive Specialized hospital where level of adherence was 30.2% in segregation of noninfectious wastes in black color-coded dust bin, 34.4% in segregation of infectious medical wastes in yellow color-coded dust bin [45]. Appropriate patient management, and maintaining environmental cleanness, (eg. prompt and careful cleaning up spills of blood and other body fluids after the spill event) is also an area which was assessed and found to have fairly lower score in these six facilities which also happen to be similar to findings from Gondar University Comprehensive Specialized hospital which scored 38.3% [45].
In the six hospitals assessed, processing of instrument was good from cleaning to either sterilization or high-level disinfection; and this was consistent with the findings by Tariku and colleagues who reported compliance with sterilization of all reusable equipment before being used on another patient to be 73.7%. However, processing of linen was not following the standards and hence the linen used in these facilities is changing color from white to brown [45].
Cough etiquette to patients, caregivers and visitors with signs and symptoms of respiratory illness improved a lot. This was due to COVID-19 pandemic where all health facilities were implementing IPC and it was mandatory for everyone going to health facilities to wear a mask and observe cough etiquette.
Implementation of pre- and post-exposure prophylaxis (PEP): In Tanzania, the pre-exposure prophylaxis in the context of IPC in health provision setting is not recommended; however, (PEP) is recommended. The score in this area is low in terms of reporting and use of PEP which is comparable to finding by Maria, et al, (2016) in Tanzania that found that out of 357 health care workers who had a blood exposure in the previous 6 months, only 34% reported it and only 58% were offered PEP [46]. Provision of hepatitis B vaccination is the only vaccine which is given as far as the IPC is concerned. The challenges identified during assessment were lack of vaccine in the facilities and some of the health workers did not complete all the three doses, others had one and others had two doses and only a few had completed all the three as per schedule.
Outcome based on the IPCAF for facility-WHO tool
All the six hospitals were found to have IPC programmes/committees in place that are responsible for overseeing the IPC. In Tanzania these teams are QITs and IPC committees. The IPC subcommittee is a subunit of the Quality Teams. These teams were found to be actively supporting the IPC activities. However, doctors were not active and majority were nurses in these six hospitals. The other challenge of these teams is lack of advanced knowledge of IPC as recommended by WHO [47].
According to data from the assessment using IPCAF tool, the six hospitals had on-site trainers for conducting basic IPC training, as almost all hospitals reported having staff capable of performing basic IPC training. However, the trainers of basic IPC training revealed gaps especially with regard to the regularity of training and the understanding of complicated issues of IPC. The importance of consistent IPC training has been demonstrated in various publications, and given the presence of capable staff on-site, appears feasible in Tanzania hospitals [48].
The IPC guidelines were available in all six facilities. Tanzania has revised its IPC national guidelines to align with the WHO guidelines and other international updates. The guidelines have emphasized the emerging and reemerging infections as well as AMR [17]. The challenges concerning the guidelines were that not all functional areas within the health facilities were provided with the guidelines; and those that had the guidelines had limitations in terms of translating them into practice.
All the six hospitals reported documenting HAIs specifically SSIs. The documentation of the SSIs was an early inception of SSIs surveillance given the increase in awareness on the subject, following recommendations from WHO on the burden of HAIs. We found the area of surveillance to be a big gap in all the six facilities. The data from documentation of SSIs were not analyzed and used in these six facilities as recommended by the WHO [1].
Efforts to strengthen IPC in middle lower-income countries should place emphasis on multimodal strategies [49]. The concept of multimodal strategies is new in Tanzania. Effective implementation of IPC is needed to improve healthcare delivery. However, given the rather low scores obtained by the six hospitals in terms of implementing multimodal strategies in IPC interventions, it appeared that awareness for and implementation of multimodal strategies were not yet fully achieved.
Monitoring/audits of IPC practices and feedback is the area which scored lowest in all facilities. In Tanzania, the QITs /IPC teams are required to do internal assessment, supervision and mentorship. In these six facilities neither monitoring/audits of IPC practices and feedback nor assessments, supervisions and mentorships were done.
No health facility among the six hospitals had achieved standard workload, staffing and bed occupancy. As in many other sub-Saharan African countries, the ratio of healthcare staff to patients, staff work load, and bed occupancy are significantly below standard.
In the hospitals assessed, beds are arranged less than one meter apart and, in some wards, one bed was occupied by more than one patient.
These six hospitals have built environment, materials and equipment for IPC at the facility level though not at the level that national and international standards would require. However, the facilities had ongoing improvement strategy so as to attain the required standards.
Conflict of Interests
There were no conflicts of interest amongst authors.
Disclaimer
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
References
- Rasa, K. and Kilpatrick, C (2020) Implementation of World Health Organization Guidelines in the Prevention of Surgical Site Infection in Low- and Middle-Income Countries: What We Know and Do Not Know. Surg Infect (Larchmt) Sep;21(7):592-598. doi: 10.1089/sur.2020.163. http://doi.org/10.1089/sur.2020.163 Epub 2020 Jun 1. PMID: 32478641. [crossref]
- Sadler, S.J. and Fuller, A.T. (2020) Reframing infection control approaches in low-resource healthcare settings: A nod to the emic perspective. Journal of Global Health 10(2): 020340 (5 pages).[Online Publication Date: 11 August 2020]. Available at: http://www.jogh.org/documents/issue202002/jogh-10-020340.htm Accessed on 03 April, 2021. [crossref]
- Sastry, S., Masroor, N., Bearman, G., Hajjeh, R., Holmes, A., Memish, Z., et al. (2017) The 17th International Congress on Infectious Diseases workshop on developing infection prevention and control resources for low- and middle-income countries. International Journal of Infectious Diseases 57:138-143. DOI: https://doi.org/10.1016/j.ijid.2017.01.040 [crossref]
- Barrera-Cancedda, A.E., Riman, K.A., Shinnick, J.E., et al. (2019) Implementation strategies for infection prevention and control promotion for nurses in Sub-Saharan Africa: a systematic review. Implementation Sci14, DOI: https://doi.org/10.1186/s13012-019-0958-3 [crossref]
- Tartari, E., Tomczyk, S., Pires, D., Zayed, B., Coutinho Rehse, A.P., Kariyo, P., Stempliuk, V., Zingg, W., Pittet, and Allegranzi, B (2021) Implementation of the infection prevention and control core components at the national level: a global situational analysis. Journal of Hospital Infection 108:94-103. https://doi.org/10.1016/j.jhin.2020.11.025
- Cobb, N., Papali, A., Pisani, L., Schultz, M.J. and Ferreira, J.C., (2021) for the COVID-LMIC Task Force and the Mahidol-Oxford Research Unit (MORU). Pragmatic Recommendations for Infection Prevention and Control Practices for Healthcare Facilities in Low- and Middle-Income Countries during the COVID-19 Pandemic. J. Trop. Med. Hyg 104(Issue 3_Suppl):25–33. doi:10.4269/ajtmh.20-1009. https://doi.org/10.4269/ajtmh.20-1009 [crossref]
- Gould, D.J., Moralejo, D., Drey, N., Chudleigh, J.H. and Taljaard, M. (2017) Interventions to improve hand hygiene compliance in patient care. Cochrane Database of Systematic Reviews Issue 9, Art. No.: CD005186. DOI: 10.1002/14651858.CD005186.pub4. https://doi.org/10.1002/14651858.CD005186.pub4 Accessed 20 March 2021. [crossref]
- Loftus, M.J., Guitart, C., Tartari, , Stewardson, A.J., Amer, F., Bellissimo-Rodrigues, F., et al. (2019) Hand hygiene in low- and middle-income countries. International Journal of Infectious Diseases 86: 25–30. DOI: https://doi.org/10.1016/j.ijid.2019.06.002 [crossref]
- Sengupta, S., Barman, P. and Lo, J (2019) Opportunities to Overcome Implementation Challenges of Infection Prevention and Control in Low-Middle Income Countries. Curr Treat Options Infect Dis11, 267–280. DOI: https://doi.org/10.1007/s40506-019-00200-w
- Manchanda, V., Suman, U. and Singh, N (2018) Implementing Infection Prevention and Control Programs When Resources Are Limited. Curr Treat Options Infect Dis10, 28–39. DOI: https://doi.org/10.1007/s40506-018-0142-3
- Mehtar, S., Wanyoro, A., Ogunsola, F., Ameh, E.A., Nthumba, P., Kilpatrick, C., et al. Implementation of Surgical Site Infection Surveillance in Low- and Middle-Income Countries A Position Statement for the International Society for Infectious Diseases.
International Journal of Infectious Diseases (IF 3.202 ) Pub Date : 2020-07-24 , DOI: 1016/j.ijid.2020.07.021 [crossref] - United Nations General Assembly. 70/1. Transforming our world: the 2030 Agenda for Sustainable Development. Seventieth session Agenda items 15 and 116. A/RES/70/1 Resolution adopted by the General Assembly on 25 September 2015 [without reference to a Main Committee (A/70/L.1)] Distr.: General 21 October 2015. Available at: https://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E Accessed on 05th April, 2021.
- Karamagi, H.C., Tumusiime, P., Titi-Ofei, R., et al. (2021) Towards universal health coverage in the WHO African Region: assessing health system functionality, incorporating lessons from COVID-19. BMJ Global Health 6:e004618. doi:10.1136/ bmjgh-2020-004618 Available at: https://gh.bmj.com/content/6/3/e004618 Accessed on 03April, 2021. [crossref]
- Storr, J., Kilpatrick, C., Allegranzi, B. and Syed, S.B. (2016) Redefining infection prevention and control in the new era of quality universal health coverage. Journal of Research in Nursing 21(1):39-52. DOI: 1177/1744987116628328
- Ministry of Health. National Infection Prevention and Control Guidelines for Healthcare Services in Tanzania. (November 2004) Dar es Salaam, The United Republic of Tanzania. Available at: at/wzNQV Accessed on 04th April, 2021.
- Ministry of Health and Social Welfare. National Infection Prevention and Control Standards for Hospitals in Tanzania. Standards-Based Management and Recognition for Improving Infection Prevention and Control Practices – An Assessment Tool, 2012. Dar es Salaam, The United Republic of Tanzania. Available at: at/isvK1 Accessed on 04th April 2021.
- Ministry of Health, Community Development, Gender, Elderly and Children. National Infection Prevention and Control Guidelines for Health care Services in Tanzania (June, 2018). Dodoma, The United Republic of Tanzania.
- Management Science for Health. (2020) Fiscal Year 2020 Quarter 1 (October–December 2019) Report. USAID Medicines, Technologies, And Pharmaceutical Services (MTAPS) Program. Available at: https://www.msh.org/sites/default/files/mtaps_fy20q1_quarterly_report_final.pdf Accessed on 05th May, 2021.
- World Health Organization (2018) Tanzania launches training for national rapid response teams with focus on Ebola. WHO – United Republic of Tanzania, Available at: https://www.afro.who.int/news/tanzania-launches-training-national-rapid-response-teams-focus-ebola Accessed on 05th May 2021.
- AdnanShereen, M., Khan, S., Kazmi, A., et al (2020) COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research 24 (2020): 91–98. https://doi.org/10.1016/j.jare.2020.03.005 [crossref]
- Fauci, A.S., Lane, H. C. and Redfield, R.R. (2020) Covid-19 — Navigating the Uncharted. Engl J Med 382(13):1268-1269. DOI: 10.1056/NEJMe2002387. Available at: https://www.nejm.org/doi/full/10.1056/nejme2002387 Accessed on 05th April, 2021.
- Necochea, E., Tripathi, V., Kim, Y-M., Akram, N., Hyjazi, Y., da Luz Vaz, M., et al. (2015). Implementation of the Standards-Based Management and Recognition approach to quality improvement in maternal, newborn, and child health programs in low-resource countries. International Journal of Gynaecology and Obstetrics 130:S17-S24. DOI: http://dx.doi.org/10.1016/j.ijgo.2015.04.003 [crossref]
- Ministry of Health and Social Welfare (2011). The Tanzania Quality Improvement Framework in Health Care (2011–2016), October, 2011. Dar es Salaam, Tanzania. Available at: at/auFJK Accessed on 05th May 2021.
- Kacholi, G. and Mahomed, O.H. (2020). Sustainability of quality improvement teams in selected regional referral hospitals in Tanzania. International Journal for Quality in Health Care, mzaa032, DOI: https://doi.org/10.1093/intqhc/mzaa032 [crossref]
- Branch-Elliman, W., Price, C.S., Bessesen, M.T. et al. (2015) Using the Pillars of Infection Prevention to Build an Effective Program for Reducing the Transmission of Emerging and Reemerging Infections. Curr Envir Health Rpt2, 226–235. DOI: https://doi.org/10.1007/s40572-015-0059-7 [crossref]
- Weber, D.J., Sickbert-Bennett, E.E., Kanamori, H. and Rutala, W.A. (2019). New and emerging infectious diseases (Ebola, Middle Eastern respiratory syndrome coronavirus, carbapenem-resistant Enterobacteriaceae, Candida auris): Focus on environmental survival and germicide susceptibility. American Journal of Infection Control 47:A29−A38. DOI: https://doi.org/10.1016/j.ajic.2019.03.004 [crossref]
- Devaux, C.A. (2012) Emerging and re-emerging viruses: A global challenge illustrated by Chikungunya virus outbreaks. World J Virol 1(1):11-22. DOI: https://dx.doi.org/10.5501/wjv.v1.i1.11 [crossref]
- World Health Organization Regional Office for Africa. Weekly Bulletin on Outbreaks and other Emergencies. Week 31: 29 July-04 August 2017. Data reported by 17:00; 04 August 2017. Available at: http://apps.who.int/iris/bitstream/handle/10665/258688/OEW31-2970482017.pdf?sequence=1 Accessed on 30th April, 2021
- World Health Organization Regional Office for Africa. Weekly Bulletin on Outbreaks and other Emergencies. Week 22: 25 -31 May 2020. Data as reported by: 17:00; 31 May 2020. Available at: https://apps.who.int/iris/bitstream/handle/10665/332246/OEW22-2531052020.pdf Accessed on 30th April, 2021.
- World Health Organization Regional Office for Africa. Weekly Bulletin on Outbreaks and other Emergencies. Week 16: 12-18 April, 2021.Data as reported by: 17:00; 18 April, 2021. Available at: https://apps.who.int/iris/bitstream/handle/10665/340903/OEW16-1218042021.pdf Accessed on 30th April, 2021.
- Mangu, C. D., Manyama, C. K., Msila, H., Sudi, L., Chaula, G., Ntinginya, N. E., Sabi, I., and Maboko, L. (2016). Emerging viral infectious disease threat: Why Tanzania is not in a safe zone. Tanzania Journal of Health Research 18(3). https://doi.org/10.4314/thrb.v18i3.
- President’s Office – Public Service Management and Good Governance (PO-PSMGG). The Approved Functions and Organization Structure of The Ministry of Health, Community Development, Gender, Elderly and Children (Approved by the President on 7th July, 2018). July, 2018. Dodoma, The United Republic of Tanzania. Available at: at/uNW24 Accessed on 04th April, 2021.
- Fauci, A.S. and Eisinger, R.W. (2018) PEPFAR – 15 Years and Counting the Lives Saved. N Engl J Med 378(4):314-316. DOI: 1056/NEJMp1714773. PMID: 29365298. [crossref]
- Hokororo, J., Eliakimu, E., Ngowi, R., et al. (2021) Report of Trend for Compliance of Infection Prevention and Control Standards in Tanzania from 2010 to 2017 in Tanzania Mainland. Microbiol Infect Dis 5(3): 1-10. Available at: https://scivisionpub.com/pdfs/report-of-trend-for-compliance-of-infection-prevention-and-control-standards-in-tanzania-from-2010-to-2017-in-tanzania-mainland-1598.pdf Accessed on 04th April, 2021.
- Ministry of Health and Social Welfare. National Communication Strategy for Infection Prevention and Control 2012 – 2017. (December 2012). Dar es Salaam, The United Republic of Tanzania. Available at: at/oSVX6 Accessed on 04th April, 2021.
- Ministry of Health, Community Development, Gender, Elderly and Children. The National Guidelines for Water, Sanitation and Hygiene in Health Care Facilities (October, 2017). Environmental Health and Sanitation Section, Directorate of Preventive Services, Dodoma, The United Republic of Tanzania. Available at: https://www.moh.go.tz/en/guidelines?start=60 Accessed on 04th April, 2021.
- Ministry of Health, Community Development, Gender, Elderly and Children (July, 2020). National Environmental Health, Sanitation and Hygiene Supervision Guidelines. Environmental Health and Sanitation Section, Directorate of Preventive Services, Dodoma, The United Republic of Tanzania. Available at: https://www.moh.go.tz/en/guidelines?start=10 Accessed on 04th April, 2021.
- Ministry of Health, Community Development, Gender, Elderly and Children (August 2020). National IPC Standards for Hospitals in Tanzania.
- Tomczyk, S., Aghdassi, S., Storr, J., Hansen, S., Stewardson, A.J., Bischoff, P., Gastmeier, P. and Allegranzi, B (2020) Testing of the WHO Infection Prevention and Control Assessment Framework at acute healthcare facility level. J Hosp Infect 105(1):83-90. DOI:https://doi.org/10.1016/j.jhin.2019.12.016 Epub 2019 Dec 21. PMID: 31870887. [crossref]
- Wagenaar, B.H., Hirschhorn, L.R., Henley, C. et al.(2017). Data-driven quality improvement in low-and middle-income country health systems: lessons from seven years of implementation experience across Mozambique, Rwanda, and Zambia. BMC Health Serv Res 17, 830 (2017). DOI: https://doi.org/10.1186/s12913-017-2661-x [crossref]
- World Health Organization (2018) Infection Prevention and Control Assessment Framework at the Facility Level. https://www.who.int/infection-prevention/tools/core-components/IPCAF-facility. Accessed on 21st May 2021
- World Health Organisation, 2009. WHO Guidelines on Hand Hygiene in Health Care: a Summary. https://www.who.int/gpsc/5may/tools/who_guidelines-handhygiene_summary.pdf. Accessed on 22nd April 2021
- Garedew Tadege Engdaw, Mulat Gebrehiwot& Zewudu Andualem (2019) Hand hygiene compliance and associated factors among health care providers in Central Gondar zone public primary hospitals, Northwest Ethiopia. https://aricjournal.biomedcentral.com/. Accessed on 22nd April 2021. [crossref]
- R Okello1, Kansime2 , J Odora3 , J A Apio4 , I Pecorella (2017) Barriers and Factors Affecting Personal Protective Equipment Usage in St. Mary’s Hospital Lacor in Northern Uganda. https://dx.doi.org/10.4314/ecajs.v22i1.8. Accessed on 23rd April 2021.
- Tariku Gebre Haile, Eshetu Haileselassie Engeda, and Abdella Amano Abdo (2016) Compliance with Standard Precautions and Associated Factors among Healthcare Workers in Gondar University Comprehensive Specialized Hospital, Northwest Ethiopia. https://downloads.hindawi.com/journals/jeph/2017/2050635.pdf. Accessed on 23rd April 2021. [crossref]
- Maria Lahuerta, Dejana Selenic, Getachew Kassa, Goodluck Mwakitosha, Joseph Hokororo, Henock Ngonyani, Sridhar V Basavaraju, Cari Courtenay-Quirk, Yang Liu, Koku Kazaura, Daimon Simbeye, Naomi Bock, et al. (2016) Reporting and case management of occupational exposures to blood-borne pathogens among healthcare workers in three healthcare facilities in Tanzania. https://doi.org/10.1177%2F1757177416645343. Accessed on 24th April 2021.
- World Health Organization. (2018). Leadership and programme management in infection prevention and control. https://www.who.int/infection-prevention/tools/core-components/advanced-training-leadership.pdf? Accessed on 21st May 2021.
- Constantinos T., Gabriel B., Erik B., Aleksander D, Lenny ten H., Enrique C. et (2020) Education and training programmes for infection prevention and control professionals: mapping the current opportunities and local needs in European countries. https://aricjournal.biomedcentral.com/ Accessed on 22nd April 2021. [crossref]
- Kritsotakis, E. orcid.org/0000-0002-9526-3852, Astrinaki, E., Messaritaki, A. et al. (2018) Implementation of multimodal infection control and hand hygiene strategies in acute-care hospitals in Greece: a cross-sectional benchmarking survey. American Journal of Infection Control. ISSN 0196-6553 https://doi.org/10.1016/j.ajic.2018.04.217. Acessed on 22nd April 2021.