Abstract
Skeletal Class III malocclusions pose significant challenges in orthodontic treatment, often requiring a multidisciplinary approach for successful correction. Miniplates have emerged as a valuable adjunct in orthodontic therapy, offering enhanced skeletal anchorage and facilitating complex movements. This article aims to evaluate orthodontic habits and practices concerning the use of miniplates in addressing Skeletal Class III malocclusions, analyzing their efficacy, challenges, and current trends.
Introduction
The aim is to discuss the challenges associated with correcting Skeletal Class III malocclusions using traditional methods like facemasks and introduces the use of titanium miniplates by De Clerck as an alternative. The miniplate technique aims to mitigate skeletal effects while advancing the zygomaticomaxillary complex, thereby reducing undesirable impacts on facial aesthetics and dental compensationSkeletal Class III malocclusions are characterized by mandibular prognathism or maxillary retrognathism, leading to functional and esthetic concerns. The complexity of Skeletal Class III malocclusions, arising from maxillary deficiency or mandibular prognathism, influenced by genetic and environmental factors [1,2] occupates many clinicians. Traditional approaches, like the facemask, used at young age, primarily address sagittal disharmony in growing children but often lead to dentoalveolar compensations and potential skeletal effects, with significant relapse in preadolescents [3,4]. Traditional orthodontic approaches often face limitations in achieving optimal results, necessitating supplementary methods like miniplates for reinforcement. The utilization of miniplates as temporary anchorage devices has gained popularity, revolutionizing treatment strategies for Class III malocclusions [3].
Miniplates in Orthodontics
Miniplates, also known as temporary anchorage devices (TADs), are titanium implants placed into bone to provide absolute anchorage for orthodontic tooth movement. Their use in Class III correction involves strategic placement to counteract undesired skeletal growth patterns, aiding in achieving outcomes that are more predictable. De Clerck’s introduction of titanium miniplates for Class III correction represents a significant shift in treatment methodology [2,5,6]. The strategic placement of these miniplates in the maxilla and mandible, coupled with inter-arch elastics, allows for continuous application without extra-oral devices. This technique aims to advance the zygomaticomaxillary complex while minimizing adverse skeletal effects [7-10].
Advantages and Considerations of Miniplate Technique
The miniplate system offers advantages such as continuous wear without extra-oral devices and potential avoidance of undesirable skeletal and dental compensations [10]. However, the timing of mandibular plate placement is contingent upon the eruption of mandibular canines to mitigate anatomical risks [8]. Regular elastics changes and the possibility of incorporating composite bite-ramps to bypass anterior crossbites illustrate the adaptability of this technique to individual patient needs. Assessing factors that hinder the implementation of this technique could shed light on barriers to its widespread adoption and guide improvements in its application.
Evaluation of Orthodontic Habits and Practices
Clinical Efficacy
Numerous studies demonstrate the effectiveness of miniplates in Class III treatment, showcasing favorable outcomes in controlling skeletal discrepancies and facilitating complex orthodontic movements [10-12].
Challenges and Limitations
Despite their advantages, challenges exist, including potential risks of infection, implant failure, or interference with adjacent structures. Moreover, patient compliance and meticulous surgical technique are crucial for successful integration and stability.
Treatment Approaches
Diverse treatment protocols exist, ranging from unilateral to bilateral miniplate placements, depending on the severity and nature of the malocclusion. Combining miniplates with orthognathic surgery or utilizing them solely for orthodontic camouflage influences treatment approaches.
Current Trends and Innovations
Ongoing research aims to refine miniplate designs, improve insertion techniques, and explore novel materials to enhance biocompatibility and reduce potential complications.
The data presented in our recent survey (Friang et al.) sheds light on the preferences and practices of orthodontists regarding the management of Skeletal Class III malocclusions, notably focusing on the utilization of miniplates as a treatment modality. The findings encompass aspects such as practitioner experience, treatment modalities employed, obstacles encountered, treatment duration, satisfaction levels, observed effects, and potential relapses associated with miniplate usage.
Orthodontist Experience and Treatment Choices
The distribution of practitioners based on experience elucidates an interesting trend in treatment preference. Less experienced orthodontists (<5 years) exhibit a propensity towards prescribing miniplates, while those with more experience (>5 years) favor traditional methods like the facemask or orthosurgical treatments. This shift in treatment choices among practitioners with varying experience levels signifies an evolving trend in the orthodontic landscape.
Practitioner Preference and Prescription Patterns
The statistical analysis demonstrates a significant correlation between practitioner experience and the type of treatment prescribed. This includes a contrast in prescriptions between miniplates and facemasks, highlighting a divergence in approach based on experience (p=1.26 x 10-6). Moreover, practitioners with less experience seem to opt for miniplates more frequently, while those with greater experience tend to prefer facemask treatments or orthosurgical interventions (p=0.03, p=0.02 respectively, α=95%).
Obstacles and Patient-Related Factors
Obstacles hindering miniplate usage predominantly include high financial costs, perceived treatment burden, fear of pain, logistical challenges, and issues related to patient cooperation. These factors impede the widespread adoption of miniplates and warrant attention for enhancing patient acceptance and accessibility to advanced orthodontic modalities.
Treatment Duration, Satisfaction, and Observations
The active treatment duration primarily spans 6 to 18 months, with a majority of practitioners satisfied or very satisfied with the obtained results. Notably, a significant percentage (14%) expresses dissatisfaction. Most practitioners report observing skeletal effects post-miniplate usage, such as maxillary protrusion, mandibular clockwise rotation, and, to a lesser extent, mandibular setback. Additionally, observed dentoalveolar effects and relapse occurrences post-treatment are noteworthy considerations (Figures 1-10).
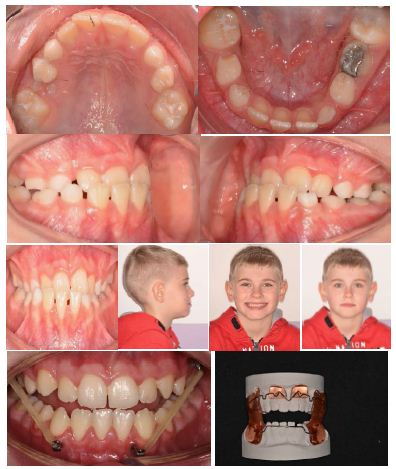
Figure 1-10: Dentoalveolar effects and relapse occurrences post-treatment
Conclusion and Implications
The study provides valuable insights into the preferences, challenges, and outcomes associated with miniplate usage in managing Skeletal Class III malocclusions. The findings underscore the impact of practitioner experience on treatment choices and highlight the multifaceted challenges influencing the adoption and execution of advanced orthodontic techniques. Addressing these obstacles could enhance patient acceptance and overall treatment outcomes, ultimately contributing to improved patient care in orthodontic practice. Further research and strategies focused on overcoming these hurdles would be instrumental in refining and expanding the use of advanced orthodontic modalities like miniplates.
The utilization of miniplates in correcting Skeletal Class III malocclusions represents a paradigm shift in orthodontic therapy. Despite challenges, they offer valuable benefits in enhancing treatment outcomes. Continued advancements in technology and research promise further refinement and optimization of miniplate utilization, ensuring improved patient care and successful management of Class III malocclusions. Studying Orthodontists’ practices and understanding potential barriers could contribute to refining and expanding the use of this technique, potentially offering more efficient and patient-friendly treatment options for individuals with moderate Skeletal Class III malocclusions.
References
- Proffit WR, Fields Jr HW, Sarver DM (2018) Contemporary orthodontics. Elsevier Health Sciences; 2018.
- De Clerck H, Nguyen T, De Mot B, Wilson M (2011) A prospective study on the effects of the biscupid intrusion appliance in the treatment of anterior open bite. European Journal of Orthodontics 33: 298-305. [crossref]
- Ngan P, Moon W (2015) Evolution of Class III treatment in orthodontics. American Journal of Orthodontics and Dentofacial Orthopedics 148: 22-36.
- Sivieri A, Manni A, Bonetti GA, et al. (2020) Treatment of Class III malocclusion with skeletal anchorage: A review of the literature. Prog Orthod 21: 9. [crossref]
- Baccetti T, Franchi L, McNamara Jr JA (2002) An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthodontist 72: 316-323. [crossref]
- De Clerck H, Geerinckx V, Siciliano S (2002) The zygoma anchor. Journal of Clinical Orthodontics 36: 455-459.
- Wilmes B, Ludwig B (2011) Uprighting mesially impacted mandibular permanent second molars using orthodontic miniscrew anchorage. Journal of Clinical Orthodontics 45: 443-448. [crossref]
- Bae SM, Park HS, Kyung HM, Kwon OW, Sung JH (2022) Clinical application of micro-implant anchorage. Journal of Clinical Orthodontics 36: 298-302. [crossref]
- Park HS, Lee SK, Kwon TG (2007) Treatment of Class III malocclusion using a non-surgical approach with microscrew implants. Angle Orthod 77: 1119-1128.
- Cha JY, Kim HJ, Hwang CJ (2018) Skeletal anchorage for orthodontic correction of severe Class III malocclusion. Am J Orthod Dentofacial Orthop 153: 321-330.
- Ludwig B, Glasl B, Bowman SJ, Wilmes B, Kinzinger GS et al. (2011) Anatomical guidelines for miniscrew insertion: Palatal sites. J Clin Orthod 2011;45: 433-441. [crossref]
- Kircelli BH, Pektas ZO, Uckan S (2011) Orthopedic protraction with skeletal anchorage in a patient with maxillary hypoplasia and hypodontia. Am J Orthod Dentofacial Orthop 139: 699-712. [crossref]