Abstract
The first recorded human case of the Monkeypox virus occurred in the Democratic Republic of the Congo in 1970. Over the past six decades, human Monkeypox has remained endemic in Western and Central Africa and emerged as a global public health threat since 2022 [1,2]. The Africa Centers for Disease Control and Prevention (Africa CDC) classified the escalating Mpox outbreak across 15 countries in the World Health Organization (WHO) African Region as a Public Health Emergency of Continental Security. In response, WHO Director-General Dr. Tedros Ghebreyesus declared a Public Health Emergency of International Concern (PHEIC) on 14 August 2024. This global outbreak has affected over 120 countries since 2022. Addressing this prolonged endemic requires global collaboration and concerted efforts. Given the similarities between smallpox and Mpox, valuable lessons can be drawn from the successful eradication of smallpox in 1980. The global vaccination model and eradication of smallpox in 1977 are compared with lessons from the ongoing Mpox endemic since 1970.
Keywords
Poxvirus vaccination, Monkeypox, Vaccine awareness, Vaccine inequity, Vaccine monopoly, Vaccine subsidy
The Global Vaccination Model and Eradication of Smallpox
The eradication of smallpox in 1980 was the result of a highly successful global vaccination campaign led by the World Health Organization (WHO). This effort demonstrated an unparalleled level of global collaboration among WHO, health agencies, epidemiologists, and international workers. The intensified smallpox eradication program successfully implemented six key components, which played a pivotal role in eradicating smallpox in Africa by 1977 [2]. As depicted in Figure 1, these components included international funding for the eradication program and collaboration efforts, vaccine production, technology transfer, vaccine donations, vaccine distribution, and vaccination mobilization.
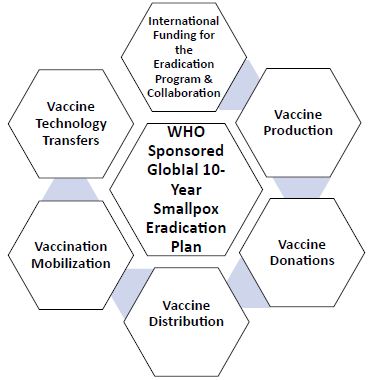
Figure 1: Global Vaccination Model and Eradication of Smallpox in 1980.
International Funding for the Eradication Program and Collaboration
The intensified smallpox eradication program was funded by the WHO, the World Health Assembly, and endemic countries. The World Health Assembly mobilized member nations to commit resources, with two-thirds of the funding coming from donations. Maintaining the program over a decade depended on strong collaboration among eradication staff at WHO headquarters, supervisory personnel at national and provincial levels, and local health workers [2]. This multi-level global partnership and pooled resources were essential for the effective coordination of large-scale surveillance and containment initiatives [2,3].
Vaccine Production and Vaccine Technology Transfers
A key aspect of the vaccination efforts in the 1970s was the production of higher-quality freeze-dried vaccines and the large-scale manufacture of user-friendly bifurcated needles. Additionally, vaccine technology transfers enabled higher-risk countries to produce their freeze-dried vaccines and serve as suppliers [2].
Vaccine Donations
Many endemic countries, being developing nations, lacked sufficient health budgets to fund a smallpox eradication program. Vaccine donations played a crucial role, with the U.S. and Soviet Union leading as major contributors, providing over 450 million doses of vaccine. Other donor countries, including the U.K., France, Canada, and Cuba, also contributed vaccines, which were distributed by the WHO [2,4].
Vaccine Distribution and Vaccination Mobilization
Higher-quality freeze-dried vaccines, which were easier to store and administer, facilitated the mass distribution and mobilization of vaccines. This advancement supported universal childhood immunization programs and mass vaccination efforts, even in regions with underdeveloped health systems and significant logistical challenges. The global smallpox vaccination campaigns achieved remarkable success through targeted surveillance-containment strategies and robust collaboration among health personnel and surveillance officers [5].
Lessons from the Ongoing Mpox Endemic Since 1970
As discussed in the preceding section, the WHO played a pivotal role in the successful implementation of the global intensified smallpox eradication program by securing collaborative resources and driving mass vaccination efforts. Unfortunately, the strategies that proved effective in eradicating smallpox have not been adequately applied to combat Mpox. Since 1970, the Democratic Republic of Congo has experienced endemic Mpox cases. A WHO-sponsored global Mpox vaccination campaign remains largely absent due to significant barriers to vaccine access, despite the creation of the Mpox Strategic Preparedness, Readiness, and Response Plan (SPRP) [6,7]. As shown in Figure 2, six key components highlight the global disparities in Mpox vaccination efforts.
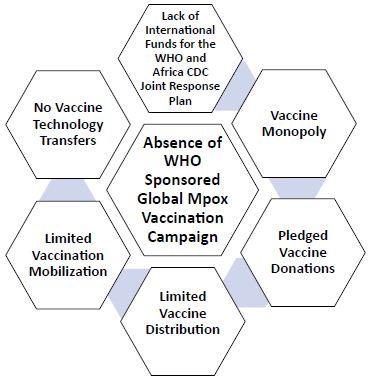
Figure 2: Lessons from the Ongoing Mpox Endemic Since 1970.
Lack of International Funds for the WHO and Africa CDC Plan
Although Mpox has persisted as an endemic issue in Western Africa for decades, international funding to combat this pandemic has been insufficient. As demonstrated by the global smallpox eradication campaign, international funding and collaborative efforts are critical for the success of the SPRP. The WHO should take a leading role in securing increased financial support from member nations to fund the WHO and Africa CDC Plan, complementing the U.S.’s pledge of at least $500 million [8].
Vaccine Monopoly and No Vaccine Technology Transfers
Compared to the AIDS and COVID-19 pandemic, Mpox endemic is experiencing more severe vaccine inequities due to the Mpox vaccine manufacturing monopoly [9]. The Danish Bavarian Nordic is the only Mpox vaccine manufacturer in the U.S. and the European Union. Deadweight loss occurs in a monopoly as its price is above the competitive price with an inefficient lower output. The significantly high price of the Mpox vaccine at $141 quoted by the WHO poses a high pricing barrier to low-income countries and poses challenges in securing millions of shots for Africa [10]. International agencies including UNICEF are trying to secure as many as 12 million doses for African countries by 2025 [10]. Africa’s vaccine manufacturing capacity remains limited, and the uncertainty surrounding future demand for vaccines in the region discourages vaccine technology transfers [10].
Pledged Vaccine Donations
High-income countries have secured the majority of available Mpox vaccine doses, leaving endemic African countries unable to afford vaccination for their populations due to high costs and limited supply. To effectively contain Mpox outbreaks in these regions, vaccine donations and subsidies for low-cost vaccines are crucial. More than 5.4 million vaccine doses have been pledged for the Mpox response, with 3 million doses committed by Japan and 2.34 million doses contributed by the U.S., Canada, EU Member States, the European Commission Health Emergency Preparedness and Response Authority, Gavi, the Vaccine Alliance, and Bavarian Nordic [11].
Limited Vaccine Distribution and Vaccination Mobilization
Significant barriers hinder Mpox vaccine distribution in African nations, including unaffordable pricing, limited supply, logistical challenges in storage and delivery, and the limited proximity of vaccination sites [12]. Socioeconomic and cultural factors further impede vaccination mobilization, such as mistrust of vaccines and cultural opposition [13,14]. At the community level, vaccine advocates and opinion leaders should work together to reduce stigma, raise awareness, and spread accurate vaccination information.
Conclusion
The successful eradication of smallpox was achieved through an unprecedented level of global collaboration, fully implementing the intensified smallpox eradication program. The WHO played a central role by mobilizing funding, coordinating targeted surveillance and containment efforts, and leading vaccination campaigns. Vaccine donations and technology transfers significantly expanded vaccine availability, while vaccines that were easy to store and administer facilitated mass immunization efforts. In contrast, the Mpox vaccine manufacturing monopoly is severely limiting access to vaccines in African countries hardest hit by the endemic. These nations also face infrastructural, logistical, economic, and cultural barriers. To address this, the WHO and Africa CDC must mobilize collaborative resources to bring the Mpox endemic under control. Bridging vaccine disparity gaps is critical, drawing lessons from past global health efforts [15]. Global coordinated actions are increasingly necessary to combat the rising threat of infectious disease outbreaks. High-income nations should support preventive measures in resource-poor countries by investing in healthcare infrastructure, water treatment, sanitation, waste management, and transportation systems.
References
- Abbara A, Rao B, Titanji B, Boum Y, Zumla A (2022) The monkeypox outbreak must amplify hidden voices in the global discourse. The Lancet. [crossref]
- Son BWK, Wambalaba OW, Wambalaba WF (2024) A Multi-pronged Approach to Addressing Global Poxviruses Vaccine Inequity: A Case of Monkeypox. In: Rezaei, N. (eds) Poxviruses. Advances in Experimental Medicine and Biology, vol 1451. Springer, Cham. [crossref]
- Henderson, D, Klepac P (2013) Lessons from the eradication of smallpox: an interview with D. A. Henderson. Philosophical Transactions of the Royal Society of London. Series B, Biological sciences 368(1623): 20130113. [crossref]
- Haynes J, Li C (2020) The US cooperated with the Soviets on smallpox – it should do the same with China on COVID-19 vaccine distribution.
- Henderson DA, Moss B. (1999) Public Health. In: Plotkin SA, Orenstein WA, editors. Vaccines. 3rd edition. Philadelphia: Saunders.
- WHO (2022) Monkeypox Strategic Preparedness, Readiness, and Response Plan (SPRP).
- Yang Z, Gray M, Winter L (2021) Why do poxviruses still matter? Cell Biosci 11, 96. [crossref]
- HHS (2024) Announces Mpox Vaccine Donations, Boosting Domestic and International Supply. [crossref]
- Hart R (2024) Mpox Vaccine Maker Bavarian Nordic Shares Soar Amid Concern Over Virus Outbreak. Forbes.
- Wass S, Kew J (2024) Higher price of mpox vaccine to pose key hurdle in Africa order talks. Business Standard.
- WHO (2024) Donors making a difference: United against mpox, swift and effective response in action.
- Molteni M, Branswell H, Joseph A, Mast J (2022) 10 key questions about monkeypox the world needs to answer.
- Lancet Editorial Board (2022) Monkeypox: a global wake-up call. [Editorial]. The Lancet 400: 337. [crossref]
- Son B, South-Winter C (2018) Human Behavior Impacts on Health Care. Journal of International & Interdisciplinary Business Research 5(8): 138-146.
- Son BWK (2023) A Multipronged Approach to Combat COVID-19: Lessons from Previous Pandemics for the Future. In: Rezaei, N. (eds) Integrated Science of Global Epidemics. Integrated Science, vol 14. Springer, Cham.