Abstract
Objective: To assess the prevalence and factors associated with dysglycemia (diabetes and prediabetes) in older people living with HIV infection.
Method: This was a cross-sectional, analytical study with 59 older people living with HIV and using antiretroviral therapy, recruited by convenience sampling in two HIV referral hospitals in Recife (PE), between May/2018 and February/2020. The prevalence and factors associated with dysglycemia were analyzed by Chi-square, Fisher Exact, Kruskal-Wallis and Mann-Whitney tests.
Results: The mean age of the 59 older people 64.3 years and 66.1% were male. The prevalence of diabetes and prediabetes was 20.3% and 35.6%, respectively, and the significant risk factors were physical activity, coronary disease, risk of cardiovascular disease in ten years, HDL cholesterol levels and glycemia.
Conclusion: A high prevalence of diabetes and prediabetes was observed in older people living with HIV. Interventions aimed at older people with HIV and the risk of diabetes and prediabetes are necessary, especially those with a sedentary life style, with a relevant cardiovascular risk and biochemical changes that participate in metabolic syndrome.
Keywords
Older people with HIV, Diabetes, Prediabetes, Cardiovascular disease, Physical activity, Premature Aging
Introduction
The control of human immunodeficiency virus (HIV) infection has enabled an increase in life expectancy and has progressively incorporated chronic non-communicable diseases (NCDs), especially dysglycemia (prediabetes (PD) and type 2 diabetes (T2DM) and their complications [1,2].
Dysglycemia represents a major worldwide concern, especially when it affects older people living with the human immunodeficiency virus (OPLHIV), for whom there are specific risks such as the duration of infection, the degree of immunosuppression, cumulative exposure to antiretroviral therapy (ART) and co-infection with hepatitis C [3,4]. On the other hand, conventional risk factors have increased their participation in the impaired glucose tolerance process in this group, such as senescence, obesity, sedentary lifestyle and family history [5].
Associations have been reported between HIV infection and T2DM, particularly with the use of ART, with variation over time, mirroring an unequal repercussion among the many antiretroviral drugs that have emerged. Thus, the careful choice of ART regimens in those individuals facing a higher risk of developing T2DM and the selection and monitoring of antidiabetic medications in older people living with HIV targeted in drug interactions and possible comorbidities are challenges that should be part of the practice of those who deal with OPLHIV [6].
Chronic non-communicable diseases are more prevalent in older people, and HIV infection is on the increase in this population resulting from both new cases and a higher survival rate due to ART [7]. The process of senescence in older people shares pathways in the aging process promoted by HIV [8]. This reality faces prejudice, stereotypes and particularly invisibility among health professionals and society. The complexity of this research is to work on two public health problems in people aged 60 years or older, who, in developing countries, are considered to be old.
Therefore, the diagnosis and management of dysglycemia require a thorough understanding and approach, although the true prevalence of this disorder in older people remains uncertain [9]. More sensitive diagnostic tools are essential for the prevention of T2DM complications, since these are people submitted to conditions that promote aging through many mechanisms, thereby emphasizing their vulnerability and hindering a successful aging process [10].
Methods
This was a cross-sectional, analytical study that assessed the prevalence and factors associated with dysglycemia (PD and T2DM) in older people living with HIV and being treated with ART, attended at two of the three main referral services in Recife (PE) for patients with HIV and AIDS infection, recruited by convenience sampling, from May/2018 to February/2020.
The inclusion criteria applied were: aged 60 years or over, attended at specialized outpatient clinics at the selected tertiary hospitals, with a confirmed diagnosis of HIV infection. Exclusion criteria were: impaired cognition and/or communication (the Mini Mental State Examination applied by the researcher), untreated syphilis and neurological sequelae (data obtained from medical records). Each participant was personally interviewed by the researcher to complete the research instrument and additional information was collected from a review of their medical records.
Variables investigated for the sociodemographic profile: a) personal: gender, chronological age, self-reported skin color, fixed partner, schooling, monthly income of the participant; b) life habits: physical activity [11], classifying the participant as sedentary (no) or active (yes), alcohol consumption [12], considering abstention (no) or drinker (yes), current smoking [13] (yes or no) and current cannabis user (yes or no). Health of the older people: a) comorbidities (hypertension, coronary artery disease and hepatitis C categorized as “yes” if participants had a documented diagnosis of these conditions or were taking medications or self-reporting); b) geriatric dimension (urinary and fecal incontinence, visual and auditory deficits, sleep, fall, polypharmacy. For the evaluation of functionality, the Barthel Index for basic activities of daily living (ADL) was used, composed of ten functions (feeding, bathing, grooming, dressing, bowel control, bladder control, toileting, chair transfer, ambulation, stair climbing), with a score ranging from zero to 100, whereby a total score equal to 100 was considered independent [14]. For the cognition analysis, the Mini Mental State Examination (MSE) was used, with 19 items distributed in the following domains: orientation (time and place), memory, attention and calculation, recall and language. Because it is influenced by schooling, different cutoff points were proposed to minimize this problem: 18 points for illiterate people, 21 points for individuals with 1 to 3 years of schooling, 24 points for those with 4 to 7 years of schooling and 26 for participants with more than 7 years of schooling [15]. The nutritional status was analyzed through the Mini Nutritional Assessment (MAN), the only instrument validated in Brazil for the older population. It is divided into 2 modules: the first focuses on questions A to F, and may be considered as screening, with 14 being the maximum score. At the end of this first module, if the score is equal to or greater than 12 points, it is not necessary to proceed, since the participant is considered nourished. If it is less than or equal to 11 points, the assessment moves on to the second module, which is composed of 12 questions (G to R), with 16 being the maximum score. If ≥ 24 points- normal; 17 to 23.5 points – risk of malnutrition; < 17 points: malnourished [16].
The estimate of biological age (BA) was calculated by the researcher by applying an artificial intelligence algorithm [17] that includes 19 laboratory tests taken from the patient’s medical records (albumin, glucose, urea, total cholesterol, total protein, sodium, creatinine, hemoglobin, total bilirubin, triglycerides, HDL, LDL, calcium, potassium, hematocrit, CHCM, VCM, platelets and erithrocytes), weight, height and smoking information. The BA is the result obtained from the following mathematical subtraction operation: chronological age (CA) minus the age predicted by artificial intelligence. If the result is negative (CA lower than expected), there is premature biological aging. On the other hand, if the result is positive (chronological age greater than expected), there is no premature biological aging. To assess adherence to ART, the Morisky scale of four questions was applied by the researcher [18].
Medical records were used in order to collect data on diagnosis (HIV-positive serology), the use of statins [19] (Silva16) and results of complementary tests (viral load: the current and highest load; CD4+ T lymphocyte count: current and nadir; the most recent biochemical and hematological dosages in relation to the interview), details on ART (start date, number and types of regimens used) and HIV/AIDS-related diseases (toxoplasmosis, syphilis, tuberculosis).
A cardiovascular risk at 10 years was estimated using the Framingham online risk calculator based on age, sex, total cholesterol, HDL cholesterol, LDL cholesterol, smoking, diabetes mellitus and blood pressure. Individuals at low risk present 10% or less risk of cardiovascular disease (CVD) in 10 years, with an intermediate risk of 10-20% and a high risk of 20% or more [20] (Latufo17).
Glucose homeostasis disorders were defined by the ADA 2020 [21] criteria as PD (fasting plasma glucose level of 100-125 mg/dl) and T2DM (fasting plasma glucose level of at least 126 mg/dl) [22].
The research is in accordance with Resolution No. 466/2012 and Resolution No. 510/2016. The research was approved by the Research Ethics Committee of the Center for Health Sciences at the Universidade Federal de Pernambuco, under Report Number: 2.545.05. All participants signed an informed consent form.
For data analysis, a spreadsheet database was produced and exported to a database validation program. To characterize patients with regard to their profile: personal, socioeconomic, life habits, metabolic condition, ART use, disease time and disease inventory, frequency distributions were constructed. To assess which of these factors were associated with the classification of blood glucose level, the contingency table was constructed and the Chi-square test for independence was applied. In cases where the assumptions of the Chi-square test were not satisfied, the Fisher Exact test was applied. In assessing the influence of the blood glucose classification on the clinical dimension, health indicators, viral load and medication use, the contingency table was constructed and the Chi-square test was applied for homogeneity. For laboratory measurements, normality was assessed and, in cases where normality was not indicated, the distribution of the measure between the groups was made by the Kruskal-Wallis test, for comparison between the three blood glucose classification groups. In the comparison of measurements between the blood glucose classification groups, two to two, the Mann-Whitney test was applied. All conclusions were drawn considering a significance level of 5%.
Results
This study included 59 older people aged between 60 and 77 years, of whom 39 (66.1%) were male. All participants were on ART and 26 (44.1%) received 3 or more regimens. Most had an undetectable viral load (91.5%) and a CD4 T lymphocyte count above 350 cells/mm3 (71.2%). Hepatitis C virus co-infection was present in 6 of the 59 participants (10.2%) and the adherence rate to ART was 62.7%. Around 10.2% of the older people had received no formal education and 67.8% had no partner. Most had a monthly income ≤1 minimum wage (76.8%) and a normal nutritional status (91.5%). With regard to the ART groups used throughout the follow-up, nucleoside analogue reverse transcriptase inhibitors (NRTI) were dispensed for 98.3% of the older people, non-nucleoside reverse transcriptase inhibitors (NNRTI) for 61% and protease inhibitors (PI) for 57.6%. A total of 39% of the participants presented with more than 10 years of infection.
Table 1 demonstartes that chronological and biological ages did not present significant results regarding the prevalence of dysglycemia, but we observed that chronological age behaved with a higher prevalence of T2DM for participants aged between 66 and 70 years. With regard to biological age, in the groups with premature aging (BA>CA) the dysglycemic state of PD predominated and in the group without premature aging there was a higher prevalence of T2DM. Physical activity presented a difference (p=0.01), with the same prevalence of T2DM and PD (25.6% for both) in the sedentary group, while in those physically active, PD prevailed (62.5%). The independence test was not significant for the other factors assessed: sex, skin color, having a steady partner, schooling, and monthly income of the participant, alcohol consumption, smoking and cannabis use.
Table 1: Distribution of blood glucose classification according to the sociodemographic profile and life habits of participants
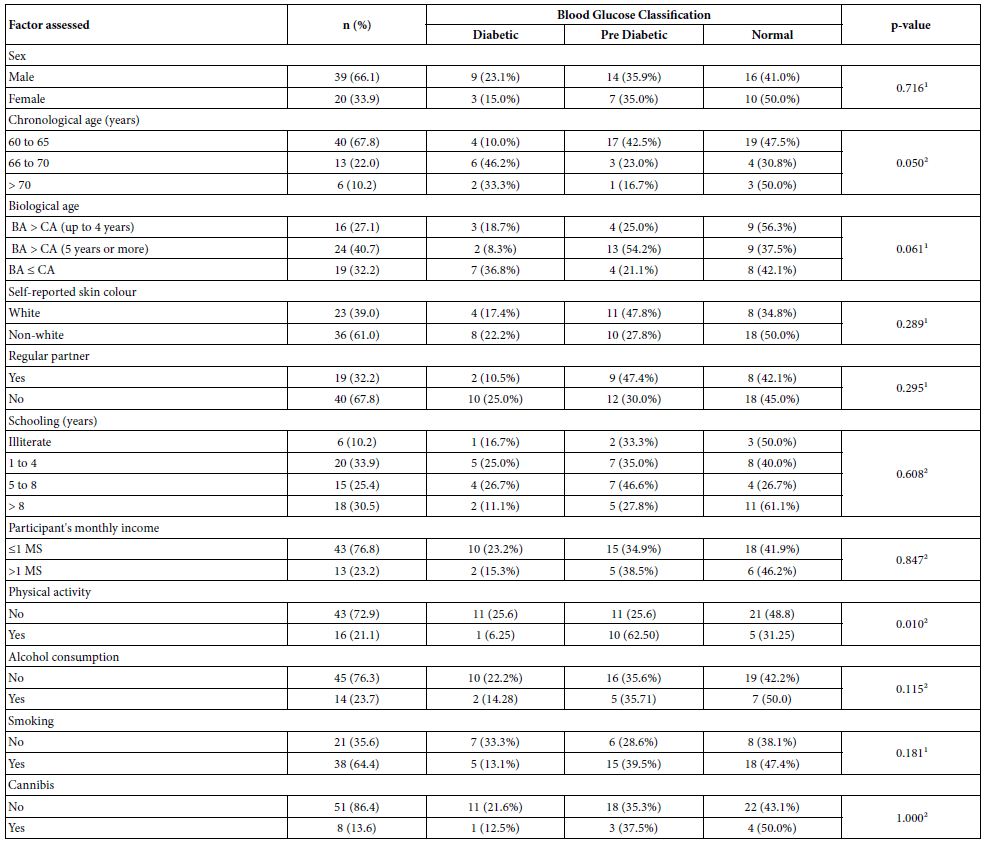
¹Qui-square test p-value for independence. ²p-value of fisher’s exact test
Table 2 presents a higher prevalence of dysglycemia in the three groups of the calendar year of initiating ART, the sum of PD and T2DM (50.0%, 57.1% and 57.1%), in relation to normal, although the homogeneity test was not significant (p-value = 0.975). For the group of patients currently using statins, there was a higher prevalence of T2DM (60%). Despite the differences in blood glucose classification for the groups of participants with certain characteristics, the independence test was not significant.
Table 2: Distribution of blood glucose classification according to disease time, ART, adect and statin
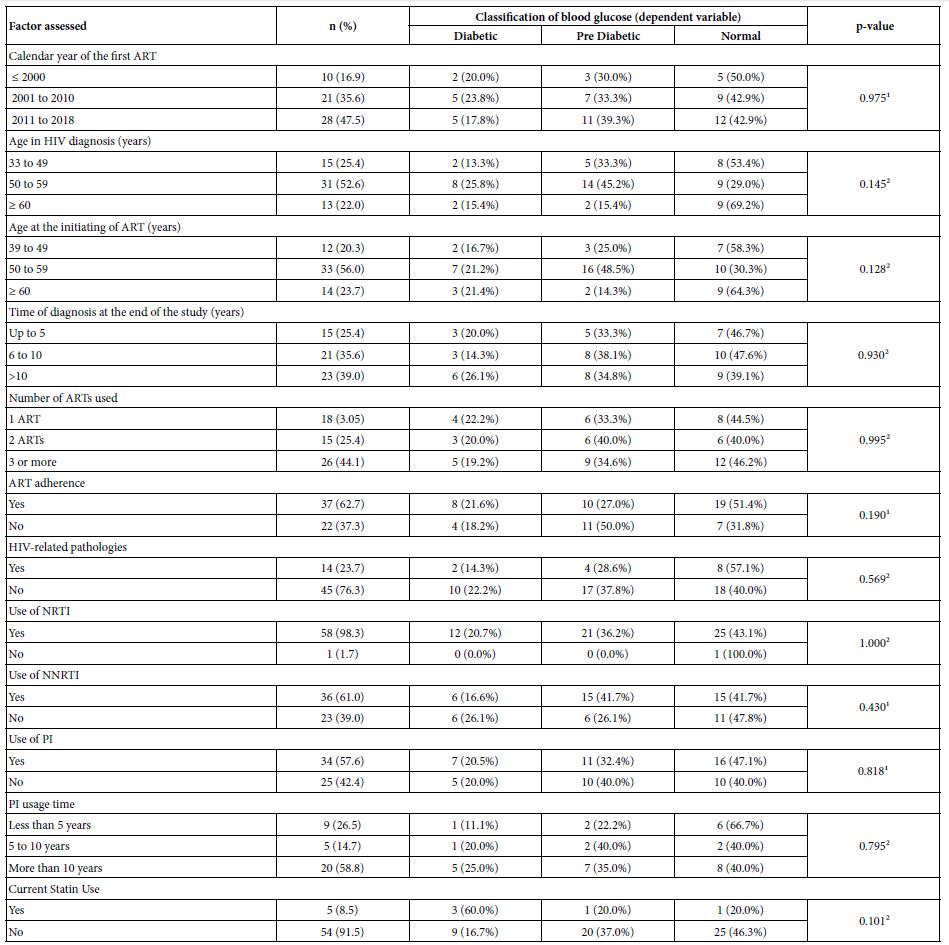
Nota: Median (Interquartile Amplitude) .¹p-value of chi-square test for independence.²p-value of fisher’s exact test. Kruskal-Wallis test ³p-value
Table 3 presents the distribution of the blood glucose classification according to the disease inventory, viral load and CD4 T lymphocyte count of the participants. The majority had normal blood glucose levels except for those with coronary heart disease, where the prevalence of diabetes was 100.0%. In the group with a history of hepatitis C, PD was more prevalent (66.6%), but was not significant. The independence test was significant only for the coronary disease factor (p-value = 0.039).
Table 3: Distribution of glycemia classification, according to the inventory of diseases of the assessed patients, viral load and CD4 T lymphocyte count
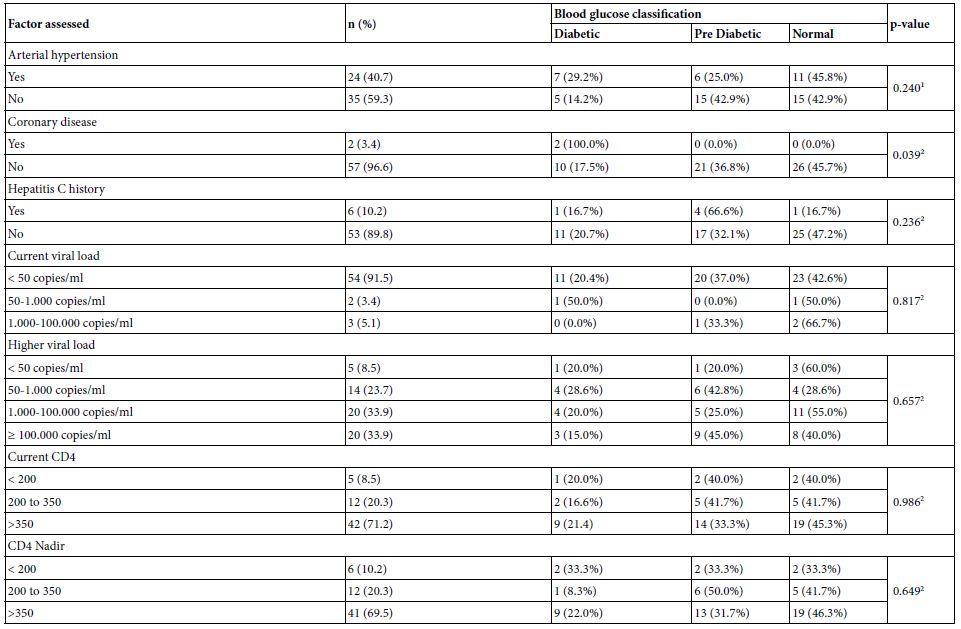
¹p-value of the chi-square test for independence. ²p-value of Fisher’s exact test
Table 4 presents the scales and geriatric clinical dimension, the Framingham score and laboratory tests of the participants according to the blood glucose classification. The Framinghan score demonstrated a higher prevalence of high-risk CVD in the T2DM (91.7%) and PD (52.4%) groups of patients. For the normal group, the highest prevalence was intermediate risk (42.3%). The homogeneity test was significant for the classification of the Framingham score (p-value = 0.020), indicating that the risk of cardiovascular events differs between the glycemic groups, being higher for those with diabetes. For the metabolic measurements, there was a difference for HDL cholesterol (p-value = 0.038) and for the last blood glucose value (p-value < 0.001). When comparing the HDL cholesterol levels between the groups, two by two, there was a significant difference only in the comparison between the group with T2DM and the normal group (p-value = 0.038). When comparing the blood glucose distribution between the classification groups, two by two, there was a significant difference between all comparisons: diabetic x pre-diabetic, diabetic x normal and pre-diabetic x normal (all comparisons with p-value < 0.001).
Table 4: Geriatric scales, geriatric clinical dimension, Framingham score and laboratory tests of participants according to blood glucose classification
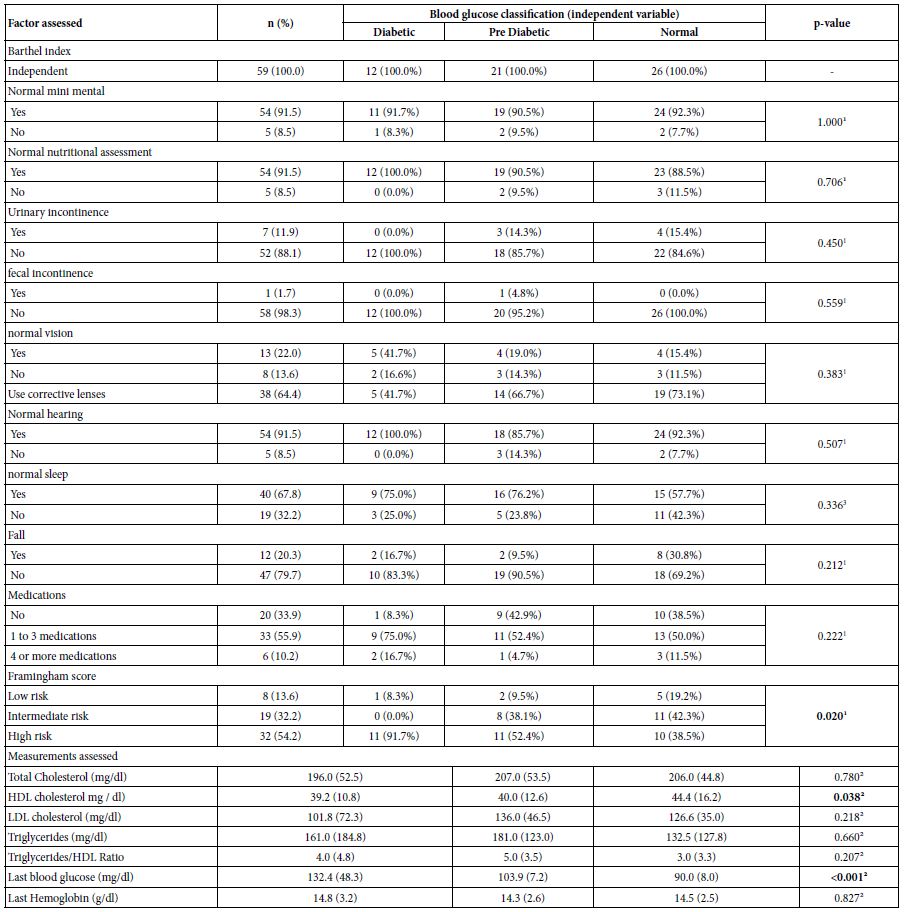
Note: Median (Interquartile Range) ¹p-value of Fisher’s exact test. ²p-value of the Kruskal-Wallis test. 3p-value of the chi-square test for homogeneity
Table 5 presents the distribution of the current ART regimen according to blood glucose classification. It appears that the most commonly used drugs by patients with diabetes are Efavirenz (NNRTI), Lavimudine (NRTI) and Zidovudine (NRTI). For the pre-diabetic groups of and normal participants, the most commonly used drugs were Lamivudine (NRTI), Ritonavir (IP) and Tenofovir (NRTI).
Table 5: Distribution of current ART regimen according to blood glucose classification
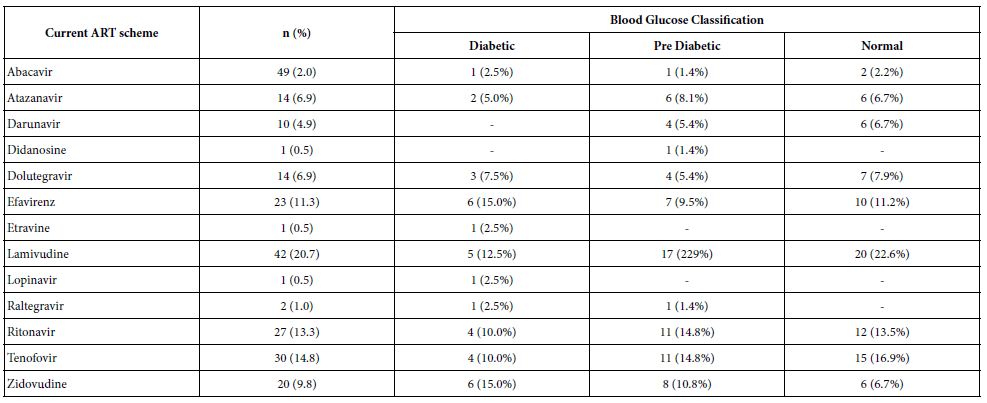
Table 6 presents the mean and standard deviation of the time (in months) of using ART according to the classification of glycemia. It was verified that in the group of participants with T2DM, the drugs that had been used for the longest mean period of time were Zidovudine (NRTI), Lamivudine (NRTI) and Ritonavir (PI). For the PD group, the drugs that had been used for the longest mean period of time were Saquinavir (PI), Ritonavir (PI) and Lamivudine (NRTI). In the normal group, the drugs that had been used for the longest mean period of time were Saquinavir (PI), Zidovudine (NRTI) and Indinavir (PI).
Table 6: Mean and standard deviation of time (in months) of using ART according to blood glucose classification
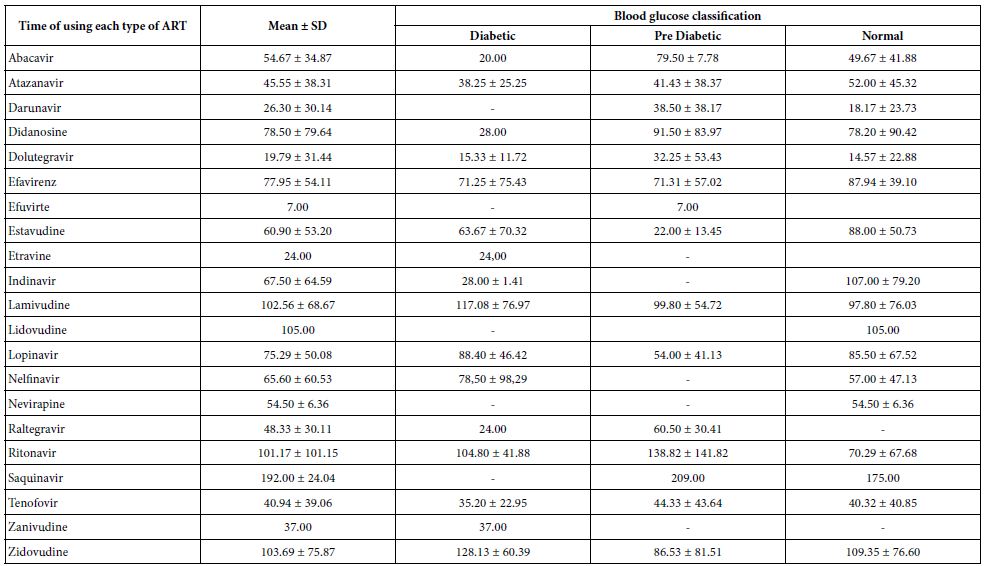
Note: Media ± standard deviation
Discussion
In this study, we evidenced a high prevalence of dysglycemia and a high risk of cardiovascular disease estimated by the Framingham score among older people living with HIV and receiving antiretroviral therapy. We observed an association between a sedentary lifestyle, coronary heart disease, HDL cholesterol levels and high current blood glucose in the T2DM and PD groups.
The prevalence of dysglycemia in older people living with HIV was 55.9%, 20.3% and 35.6% for T2DM and PD, respectively. Among adults with HIV in the US, a prevalence of diabetes was observed of 10.3%, with a higher incidence of younger individuals and no obesity [22]. Duncan, Golf et al. [23] recruited a group of ethnically diverse adults with HIV who were twice treated as outpatients in London in a cohort separated by ten years. T2DM prevalence in the initial cohort was 6.8% and 15.1% in the final cohort, with a higher risk of dysglycemia associated with time of infection, ART toxicity, increasing age and body mass index. In Africa, few studies have been conducted on the subject, with prevalences of 3.5 to 26.5% for T2DM and 20.2 to 43.5% for PD, among adults with HIV on ART [24]. In Sub-Saharan Africa, data on T2DM are scarce and the high prevalence of anemia compromises the usefulness of glycated hemoglobin in the diagnosis of dysglycemia [25]. The prevalence of T2DM and PD in our study was higher than that observed in the literature, probably because it is a sample with a CA equal to or greater than 60 years in which most presented premature aging [26]. (Pathai23).
Additionally, persistent inflammation in PLHIV (inflammaids) and senescence (inflammaging) also contribute to multiple diseases such as diabetes, CVD, kidney disease and others. Although the specific mechanisms of each process – HIV, aging, comorbidities – may be unique or shared, biomarkers of immune activation and inflammation (IL-6, CD14, CD163, D-dimer, Tumor Necrosis Factor) are known to be associated with the development and progression of pathologies in PLHIV. Inflammation is also linked to comorbidities in older people with no HIV [8,27]. A cohort assessed twice in a period separated by a peirod of 10 years, identified that the longer duration of HIV status and exposure to ART were determinants for dysglycemia [23]. In our research, the participants in the group with less biological aging and a greater frequency of T2DM had a longer period of time of a diagnosis of HIV infection and exposure to ART.
A sedentary lifestyle is a risk factor for the development of dysglycemia. In the sedentary participants of this study there was an equal prevalence of DT2 and PD, while in those physically active, the state of PD prevailed. Physical activity is linked to a reduction in the risk of diabetes in the general population, therefore, it is of express relevance for OPLHIV in view of the reduced practice of exercises observed in this population [19,23]. Segatto, Freitas et al. [28] demonstrated the protective effect of physical activity in the context of HIV, by verifying a lower incidence of lipodystrophy and an inverse relationship between physical activity and the concentration of central adiposity, which represent risk factors for the development of dysglycemia. Additionally, research conducted by Mutimura, Stewart et al. [29] reported that physically active individuals had higher CD4 levels. As in our study, Hoffmann et al. [30] assessing a cohort, concluded that there was a robust prevalence of coronary atherosclerosis in HIV patients and that glycemic levels were higher among those with atherosclerotic plaques and in the population with adequately controlled HIV, markers of immune activation were evidenced innate and arterial inflammation related to coronary artery disease (CAD). Endothelial dysfunction is the fundamental element of atherogenesis and represents the confluence of different processes. The endothelium is injured by the immunological, pharmacological release of particles secondary to the destruction of CD4+ T lymphocytes and an increased expression of adhesion molecules. Thus, an inflammatory cascade damages the vessel and promotes premature atherosclerosis. However, there are intricate specific viral mechanisms that promote sustained immunodeficiency, immune dysregulation/activation, and inflammation despite ART. Within this scenario, ART promotes a reduction of endothelial damage by controlling HIV infection, but harms this same endothelium through its involvement in glucose and lipid metabolism. Unquestionable conclusions on the role of ART in cardiovascular risk do not yet exist, since the regimens used make use of different class associations [31]. Currently, the recommendation for minimizing cardiovascular risk relies on the early initiation of ART and controlling traditional risk factors such as smoking, obesity, sedentary lifestyle, inadequate diet, among others [32].
The Framingham Risk Score is a widely used tool to estimate the absolute risk of developing cardiovascular disease over a 10-year period [33]. In this study, 91.7% of patients with T2DM and 52.4% of PD presented a high risk of CVD, according to the Framingham score, while most normal patients (42.3%) presented an intermediate risk. This finding is justified because it is a chronologically older population and with a prevalence of premature aging in 68.7% of the participants. While this score is easy to use, it may not be ideal for people with HIV because it does not include antiretroviral drugs, a fact that might generate a different risk. The duration of treatment and the large number of possible drug combinations make it difficult to assess the individual effects [34].
With regard to the metabolic measures, there was a difference for HDL cholesterol and blood glucose. Metabolic syndrome is an element of considerable importance in PLHIV, although estimates vary, partly due to the use of different diagnostic criteria and also due to the duration of the prescribed antiretroviral regimen and the differences between the populations studied. We observed a result with significance for two important components of the metabolic syndrome, with lower HDL and higher blood glucose in patients with T2DM followed by PD. Bezerra and Burgos [35], analyzing the lipid profile in PLHIV with coronary atherosclerosis, identified the protective role of HDL and its importance in preventing unfavorable early CAD outcomes, including death.
There are limitations to be observed in this study. The cross-sectional design is able to appreciate associations but frustrates the assessment of causality. The limited sample size associated with geographic restriction and male predominance generate results that cannot be extended to all OPLHIV. However, it provides a significant contribution because it is a chronologically older population, which is growing worldwide, bringing together people who are aging with HIV and those who are acquiring HIV infection from the age of 60. Another relevant point is the use of biological age estimated with the use of artificial intelligence, which confirms previous studies on premature aging in HIV carriers. Moreover, since the study was conducted at two university hospitals with a specialized HIV service, we observed a greater commitment of the participants to their treatment associated with the multiprofessional follow-up, which probably did not distort the sample and corroborated the functional and cognitive preservation of the group. In Brazil, there are few studies with national representation that indicate the prevalence of dysglycemia in older people with HIV. Thus, this work may generate perspectives on the issue.
Responding to the objectives of the study, we evidenced a high prevalence of dysglycemia among older people living with HIV infection and receiving antiretroviral therapy and the high risk of cardiovascular disease in 10 years estimated by the Framingham score. We also found differences in the variables of physical activity, coronary heart disease and levels of HDL cholesterol and blood glucose. Prospective studies are needed in order to clarify any associations, and assess the relevance of pharmacological actions and lifestyle changes to prevent the development of PD and its progression to T2DM. Faced with the great challenge of human aging, screening and preventive measures need to be created and applied to older people. Health professionals need to pay attention to the possibility of HIV in this age group, thus avoiding late diagnosis. Physicians should minimize drug interactions by understanding aspects of the geriatric prescription and the possible weaknesses of this age group.
References
- Guaraldi G, Orlando G, Zona S, et al. (2011) Premature Age-Related Comorbidities Among HIV-Infected Persons Compared With the General Clin Infect Dis. 53(11):1120-1126. [crossref]
- Kalra S, Kalra B, Agrawal N, et al. (2011) Understanding diabetes in patients with HIV/AIDS. Diabetol Metab Syndr. 3(1): 2. [crossref]
- Monroe AK, Glesby MJ and Brown TT (2015) Diagnosing and Managing Diabetes in HIV-Infected Patients: Current Concepts. Clin Infect Dis. 60(3):453-462. [crossref]
- Hulgan T (2018) Factors Associated with Insulin Resistance in Adults with HIV receiving Contemporary Antiretroviral Therapy: A Brief Update. Curr HIV/AIDS Rep. 15(3):223-232. [crossref]
- Samad F, Harris M, Puskas CM, et al. (2017) Incidence of diabetes mellitus and factors associated with its development in HIV-positive patients over the age of 50. BMJ Open Diabetes Res Care. 5(1): e000457. [crossref]
- Noubissi EC, Katte JC, Sobngwi E (2018) Diabetes and HIV. Curr Diab Rep. 18(11):1-8.
- Lopez-Otín C, Blasco MA, Partridge L, et al. (2013) The hallmarks of aging. Cell. 53(6):1194-1217. [crossref]
- Dalzini A, Petrara MR, Ballin G, et al. (2020). Biological Aging and Immune Senescence in Children with Perinatally Acquired HIV. J Immunol Res. 2020: 8041616. [crossref]
- Cunha GH, Franco KB, Galvão MTG, et al. (2020) Diabetes mellitus in people living with HIV/AIDS: prevalence and associated risk factors. AIDS Care. 32(5):600-607. [crossref]
- Coelho AR, Moreira FA, Santos AC, et al. (2018) Diabetes mellitus in HIV-infected patients: fasting glucose, A1c, or oral glucose tolerance test – which method to choose for the diagnosis?. BMC Infect Dis. 18(1):309. [crossref]
- Matsudo S, Araujo T, Matsudo V, et al. (2001) Questionario Internacional De Atividade Fisica (Ipaq): Estudo De Validade E Reprodutibilidade No Brasil. Rev Bras Atividade Física Saúde. 6(2): 5-18. [crossref]
- Defined DL. National Institute on Alcohol Abuse and Alcoholism (NIAAA). [crossref]
- Ariyothai N, Podhipak A, Akarasewi P, et al. (2004) Cigarette smoking and its relation to pulmonary tuberculosis in Southeast Asian J Trop Med Public Health. 35(1):219-227. [crossref]
- Mahoney FI and Barthel DW (1965) Functional evaluation: the barthel Md State Med J. 14: 61-65. [crossref]
- Folstein MF, Folstein SE and McHugh PR (1975) “Mini-mental state”: A practical method for grading the cognitive state of patients for the J Psychiatr Res. 12(3):189-198. [crossref]
- Vellas B, Guigoz Y, Garry PJ, et al. (1999) The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutr Burbank Los Angel Cty Calif. 15(2):116-122. [crossref]
- Mamoshina P, Kochetov K, Putin E, et al. (2018) Population Specific Biomarkers of Human Aging: A Big Data Study Using South Korean, Canadian, and Eastern European Patient Populations. J Gerontol A Biol Sci Med Sci. 73(11):1482-1490. [crossref]
- Morisky DE, Green LW and Levine DM (1986) Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 24(1):67-74. [crossref]
- Silva SP and Monteiro N (2016) Uso de estatinas e o risco de Diabetes Mellitus tipo 2: Revisão Baseada na Evidência. Rev Bras Med Fam Comunidade. 11(38): 1-8. [crossref]
- Lotufo PA (2008) O escore de risco de Framingham para doenças Rev Med. 87:232-237. [crossref]
- Association (2020) Standards of Medical Care in Diabetes-2020 Abridged for Primary Care Providers. Clin Diabetes. 38(1):10-38. [crossref]
- Hernandez-Romieu AC, Garg S, Rosenberg ES, et al. (2017) Is diabetes prevalence higher among HIV-infected individuals compared with the general population? Evidence from MMP and NHANES 2009-2010. BMJ Open Diabetes Res Care. 5(1):e000304. [crossref]
- Duncan AD, Goff LM, Peters BS (2018) Type 2 diabetes prevalence and its risk factors in HIV: A cross-sectional study. PloS One. 13(3):e0194199. [crossref]
- Rhee JY, Bahtila TD, Palmer D, et al. (2016) Prediabetes and diabetes among HIV‐infected adults in Cameroon. Diabetes Metab Res Rev. 32(6):544-549. [crossref]
- Hodel NC, Hamad A, Reither K, et al. (2020) Assessment of diabetes and prediabetes prevalence and predictors by HbA1c in a population from sub-Saharan Africa with a high proportion of anemia: a prospective cross-sectional BMJ Open Diabetes Res Care. 8(1): e000939. [crossref]
- Pathai S, Lawn SD, Gilbert CE, et al. (2013) Accelerated biological ageing in HIV-infected individuals in South Africa: a case-control AIDS Lond Engl. 27(15):2375-2384. [crossref]
- Rinaldi S, Pallikkuth S, George VK, et al. (2017) Paradoxical aging in HIV: immune senescence of B Cells is most prominent in young age. Aging. 9(4):1307-1325. [crossref]
- Segatto AFM, Freitas Junior IF, Santos VR dos, et al. (2011) Lipodystrophy in HIV/AIDS patients with different levels of physical activity while on antiretroviral Rev Soc Bras Med Trop. 44(4): 420-424. [crossref]
- Mutimura E, Stewart A, Crowther NJ, et al. (2008) The Effects of Exercise Training on Quality of Life in HAART-Treated HIV-Positive Rwandan Subjects with Body Fat Redistribution. Qual Life Res. 17(3):377-385. [crossref]
- Hoffmann U, Lu MT, Foldyna B, et al. (2021) Assessment of Coronary Artery Disease With Computed Tomography Angiography and Inflammatory and Immune Activation Biomarkers Among Adults With HIV Eligible for Primary Cardiovascular JAMA Netw Open. 4(6):e2114923. [crossref]
- Carvalho A, Valente R, Almeida-Morais L, et al. (2017) VIH e doença coronária – quando a prevenção secundária é insuficiente. Rev Port Cardiol. 36: 569. [crossref]
- Kumar S and Samaras K (2018) The Impact of Weight Gain During HIV Treatment on Risk of Pre-diabetes, Diabetes Mellitus, Cardiovascular Disease, and Mortality. Front Endocrinol. 9:705. [crossref]
- Cesarino CB, Borges PP, Ribeiro R de CHM, et al. (2013) Avaliação do risco cardiovascular de pacientes renais crônicos segundo critérios de Framingham. Acta Paul Enferm. 26(1):101-107. [crossref]
- Friis-Møller N, Thiebaut R, Reiss P, et al. (2010) Predicting the risk of cardiovascular disease in HIV-infected patients: the data collection on adverse effects of anti-HIV drugs Eur J Cardiovasc Prev Rehabil. 17(5):491-501. [crossref]
- Bezerra LA and Burgos UMMC (2021) Analise do perfil lipídico de pacientes HIV- positivo com aterosclerose coronariana/ Analysis of the lipid profile in HIV- positive patients with coronary atherosclerosis. Braz J Health Rev. 4(2):9094-9102. [crossref]