Abstract
Dentine hypersensitivity (DH) and enamel demineralisation are prevalent oral health concerns. BioMin toothpaste, containing fluoro-calcium phosphosilicate (FCPS), has emerged as a potential alternative to conventional toothpastes for remineralisation and DH management. This literature overview analyses the efficacy of a BioMin F toothpaste compared to selected conventional toothpastes in addressing DH and remineralisation. The review examines in vitro and clinical studies (in vivo) to assess the relative benefits and limitations of both approaches. Analysis of controlled clinical trials utilising VAS scores, Schiff Cold Air sensitivity scores (SCASS), and SEM imaging revealed BioMin F exhibits a distinctive temporal efficacy gradient: modest immediate tubular occlusion (18.1% sensitivity reduction at one-minute) but superior long-term efficacy (61.1% reduction at 6 weeks). Scanning electron microscopy confirmed progressive mineralisation within the dentinal tubules (50% occlusion at three weeks increasing to 75% at 6 weeks) through formation of acid-resistant fluorapatite crystals. This overview concludes that BioMin F may be appropriate for sustained rather than immediate relief, although it is recognised that more standardised long-term studies are required to validate its efficacy.
Introduction
DH is a prevalent clinical condition defined short, sharp pain that arises from exposed dentine in response to thermal, tactile, evaporative, osmotic, or chemical stimuli, in the absence of any other dental disease [1]. The pain is usually localised and self-limiting but can significantly impact an individual’s quality of life by affecting routine oral functions such as eating, drinking, and toothbrushing [2]. The average global prevalence from all studies reported by Zeola et al. [3] is around 33.5% (ranging from 4.8% to 62.3% with an estimated prevalence of 11.5%) in adults. West et al. [4] also reported that 41.9% of participants experienced DH in a multi-centre European study of young adults. DH occurs when the dentinal tubules become exposed due to loss of enamel via erosion, abrasion, abfraction or gingival recession. This allows external stimuli to affect the pulpal nerve endings resulting in a pain response. Brannstrom and Astrom’s hydrodynamic theory is the widely accepted mechanism, which proposes that movement of tubular fluid within the open dentinal tubules activates nociceptors near the pulp, resulting in pain. Management strategies for DH therefore aim to occlude the dentinal tubules, prevent fluid movement, or by nerve desensitisation which ultimately reduces their responsiveness to stimuli. Over the counter (OTC) desensitising toothpastes are the most accessible and commonly used form of treatment, and their efficacy depends on the active ingredients and mechanism of actionof the individual toothpaste formulations. BioMin F (Biomin Technologies Limited UK) is a novel bioactive glass toothpaste containing 5% fluoro-calcium phosphosilicate (FCPS), which slowly releases calcium, phosphate, and fluoride ions to promote acid-resistant fluorapatite (FAP) crystals, leading to sustained occlusion of the dentinal tubules and potential long-term relief from DH [5]. Although other desensitising toothpastes are available in the UK market, long term comparative clinical efficacy comparing the formulations are limited. Several studies have reported short term (<6 months) improvements in DH but variations in methoodology is somewhat problematic when drawing direct comparisions between the toothpastes used for DH management. DH therefore presents a persistent clinical challenge due to its high prevalence and effects on patients’ quality of life and currently there does not appear to be one ideal desensitising product for everyone [6]. Various methods have been adopted to manage DH symptoms; however, the multifactorial nature and complexity of its aetiology, coupled with the rising global prevalence, underscore the need for research and development of more effective and long-term solutions
Conventional Treatment Approaches
The primary aims of conventional DH management in the industry aims to mitigate pain symptoms by reducing fluid movement within the exposed dentinal tubules. This is achieved through physical and chemical tubule occlusion, nerve desensitisation and emerging techniques such as photobiomodulation [7]. Despite these available treatments, a gold standard treatment is not established due to the complexity of DH’s multifactorial aetiology.
Grossman [8] statedthe ideal characteristics ofa dentine desensitising agent to be one that has a rapid onset of action, sustained long term efficacy and minimal pulpal irritation. Additionally, factors such as ease of use, painless application and free from causing discolouration to the tooth are also of benefit to patients. These characteristics were updated by Gillam [9] from the clinical perspective and more recently from a chemical viewpoint by Hill and Gillam [10] (Table 1).
Table 1: An Ideal Desensitiser based on Chemical Characteristics.
| Rapid apatite formation (<6 Hrs) in the mouth |
| Formation of FAp rather than HCA |
| Particle size distribution that includes small <3 micron particles for entering the dentine tubules that give rise to tubule occlusion and larger particles for more sustained release |
| Strontium for its caries inhibition and re-mineralizing potential as well as for its possibility of binding to the odontoblast surface. |
| Fluoride releasing |
| Potassium releasing to reduce nerve sensation. |
| pH rise <8.0. |
| No harder than enamel at 3.5 GPa. |
| Inexpensive to produce (Note that strontium compounds are expensive) |
Focusing on over the counter (OTC) toothpastes (dentifrices), which include potassium salts, sodium fluoride, strontium chloride, dibasic sodium citrate, formaldehyde, sodium monofluorphosphate and stannous fluoride. Their mechanisms of action are designed to address dentine hypersensitivity by targeting specific pathways [11] (Table 2).
Table 2: Mechanisms of action of active ingredients in over-the-counter toothpastes for dentin hypersensitivity[12]
|
Active Ingredient |
Mechanism of Action |
| Potassium salts | Increase extracellular potassium ion concentration, reducing nerve excitability by depolarizing nerve endings, thereby minimizing pain transmission. |
| Sodium fluoride | Enhances enamel remineralization by promoting the formation of fluorapatite, which reduces tubule exposure and strengthens tooth surfaces. |
| Strontium chloride | Replaces calcium ions in hydroxyapatite with strontium, accelerating mineralization and forming less soluble strontium apatite to occlude dentinal tubules. |
| Tricalcium phosphate | Mimics natural remineralization by depositing calcium and phosphate within dentinal tubules, forming apatite minerals and effectively sealing tubules at a deeper level. |
| Stannous fluoride | Combines tubule occlusion through precipitation with antimicrobial activity, reducing plaque and associated sensitivity triggers. |
| Dibasic sodium citrate | Precipitates proteins within the dentinal tubules to reduce fluid movement and alleviate sensitivity. |
| Formaldehyde | Forms protein coagulates within dentinal tubules, creating a barrier that reduces fluid flow and sensitivity. |
There are several commercially available over the counter (OTC) toothpastes directed towards the reduction of DH which utilise various formulations for efficacy, including toothpastes incorporating strontium acetate and Pro-Argin™ technology. These have a varied mechanism which ultimately aim to occlude the dentinal tubules and have fast-acting desensitising properties. The effect of strontium salts has been attributed to their ability to absorb onto the connective tissue of dentine and to form strontium apatite, which may occlude the dentine tubules although the action of dentine tubule occlusion by strontium salts has not been proven [13]. Pro-Argin technology combines both calcium carbonate and arginine to create a positively charged complex that binds to the negatively charged dentine surface, effectively resulting in the occlusion of the dentinal tubules [14]. These agents provide varying levels of DH relief but may have limitations such as requiring multiple applications or exhibiting short-term effects. The emergence of a new toothpaste BioMin F toothpaste employs an advanced mechanism for managing DH by leveraging its fluoride releasing bioactive glass technology, with the active ingredient of 5% fluoro-calcium phosphosilicate (FCPS) [15]. FCPS gradually dissolves to release calcium, phosphate, and fluoride ions, which combine to form acid-resistant fluorapatite (FAP) crystals. These crystals lead to occlusion within the exposed dentinal tubules, reducing fluid movement and alleviating sensitivity. Additionally, this formulation has three times higher phosphate content and a much lower silica content with smaller particles, which aims to infiltrate into the tubules to alleviate DH symptoms [16]. Hence the use of a BioMin F toothpaste could prove to be a highly effective option in the long-term management for DH as well as in the treatment of the early carious lesion (e.g. white spots) (remineralisation).
Considering the rising prevalence of DH, this present study will attempt to evaluate and compare the efficacy of BioMin F with other commercially available toothpastes by analysing the temporal efficacy patterns at various time intervals to establish the optimal application in DH management.
Methods
Aims of the Study
This literature overview attempts to evaluates the long-term efficacy of BioMin F toothpaste in managing dentine hypersensitivity (DH) compared to conventional desensitising agents. It explores mechanisms of action, clinical effectiveness and identifies gaps in research to inform future studies.
Search Strategy
A structured literature search was conducted using PubMed, ScienceDirect, and Google Scholar to identify clinical trials, systematic reviews, and in vitro studies published from 2013 to 2025. Search terms included “BioMin F”, “bioactive glass toothpaste”, “dentine hypersensitivity”, and “desensitising agents”. No language restrictions were applied, and reference lists of key articles were screened for additional relevant studies. Grey literature was excluded to ensure the inclusion of only peer-reviewed sources.
Inclusion Criteria
Studies were selected based on the following criteria:
- Inclusion Criteria: Peer-reviewed clinical trials, systematic reviews, and in vitro studies (2013–2025). Research comparing BioMin F with conventional desensitising
- Studies evaluating tubule occlusion, DH relief, and remineralisation
Exclusion Criteria:
- Non-peer-reviewed sources, case reports, and anecdotal
- Studies on non-dental applications of bioactive glass. Research on in-office treatments unless directly comparing BioMin F with conventional
PICO Criteria
A structured framework was applied to guide the selection of the published literature (Table 3).
Table 3: PICO Criteria.
|
PICO Component |
Description |
| Patient and Population (P) | Adults (≥18 years) diagnosed with dentine hypersensitivity (DH) due to mechanical or thermal stimuli. |
| Intervention (I) | Use of a BioMin F toothpaste containing fluoro-calcium phosphosilicate (FCPS) for DH management. |
| Comparator or Control (C) | Conventional desensitising toothpastes containing potassium nitrate, fluoride (stannous/sodium), or strontium chloride, or a placebo, |
| Outcomes (O) | Reduction in dentine hypersensitivity, assessed using Schiff Cold Air sensitivity scores (SCAS/ SCASS), visual analogue scales (VAS), and scanning electron microscopy (SEM) analysis of tubule occlusion. |
Results
In Vitro Studies
To supplement the clinical evidence of the efficacy of Biomin F toothpastes in the management of various clinical conditions such as dentine hypersensitivity, remineralisation and the early carious lesion as well in bleaching sensitivity, tables were constructed to compare the effectiveness of Biomin F with other recognised toothpastes (Table 4).
Table 4: Comparison of selected in vitro studies evaluating the effectiveness of desensitising products.
|
Study No |
Author | Study design |
Conclusion |
|
1 |
Alhussain et al.2018 |
The aim of this study was to assess the efficacy of a toothpaste based on novel fluoride incorporated bioactive glass in remineralizing artificial carious lesions in human enamel and compare it with a standard fluoride-containing toothpaste. Twenty-four human extracted teeth were sectioned at the cementoenamel junction to obtain enamel blocks. These blocks (n=24) were randomly divided into 3 groups, with each group containing 8 specimens: group 1 (negative control group; distilled water), group 2 (positive control group; fluoride toothpaste) and group 3 (test group; BioMin™ F toothpaste). |
The BioMin F group outperformed the other two groups in terms of remineralizing the demineralized enamel structure. |
|
2 |
da Cruz et al. 2018 |
The aim of the present study, therefore, was to compare several bioactive glass formulations to investigate their effectiveness in an established in vitro model. A 45S5 glass was synthesized in the laboratory together with several other glass formulations: (1) a mixed glass (fluoride and chloride), (2) BioMinF, (3) a chloride glass, and (4) an amorphous chloride glass. |
The dentine samples were analyzed using scanning electron microscopy (SEM), and observation of the SEM images indicated that there was good surface coverage following artificial saliva immersion. Furthermore, although the acid challenge removed the hydroxyapatite layer on the dentine surface for most of the samples, except for the amorphous chloride glass, there was evidence of tubular occlusion in the dentine tubules. The conclusions from the study would suggest that the inclusion of bioactive glass into a toothpaste formulation may be an effective approach to treat DH. |
|
3 |
Pereira et al, 2018 |
In-vitro, 45 dentine specimens
The purpose of this study was to evaluate the in vitro effectiveness of two different bioglass- containing commercial desensitizing toothpastes together with a fluoride containing toothpaste as a control on dentinal tubule occlusion before and after a citric acid challenge and immersion in artificial saliva. Forty-five dentine specimens with patent tubules were randomly divided into 3 groups (n=15), Group A: brushing with Biomin (Elsenz®); Group B: brushing with Novamin (Sensodyne Repair®); and control Group C: brushing with fluoride (Colgate Total®). In each group, treated specimens were further subdivided into Subgroup A: directly underwent SEM, Subgroup B and C soaked in 0.3% citric acid and artificial saliva (Wet mouth®) for 5 minutes respectively. The percentage of tubule occlusion (%OCT) of representative images from each group was analyzed using an environmental scanning electron microscopy and were scored by blind review. |
The %OCT with BioMin® containing toothpaste was significantly higher than NovaMin® and a control i.e., fluoride containing toothpaste. Biomin ® and Novamin® containing toothpastes showed significant citric acid resistant compared to the fluoride containing toothpaste although the BioMin® containing toothpaste significantly showed better resistant to a citric acid challenge than the NovaMin® containing toothpaste. Immersion in artificial saliva resulted in an increase in tubular occlusion for all groups which was insignificant. |
|
4 |
Farooq et al. 2021 |
This study aimed to analyze the enamel remineralization efficacy of a novel fluoridated bioactive glass (F-BG) toothpaste compared to a standard fluoride toothpaste. Seventy-two enamel blocks (N=72) were divided into groups of twenty-four blocks according to the toothpaste exposure— group 1: brushed with distilled water, group 2: brushed with fluoride toothpaste (Colgate™), and group 3: brushed with F-BG toothpaste (BioMinF™). |
The F-BG toothpaste, in comparison to fluoride toothpaste, showed greater surface micro-hardness (VHN), a smoother enamel surface (low surface roughness), and better enamel volume restoration (remineralization) within the limitations of the experiment. Future in vitro studies and in vivo trials validating the formation of FAP and clinical remineralization potential of F-BG toothpaste are recommended. |
|
5 |
Khare et al. 2022 |
The aim of the study was to compare and evaluate the efficacy of BioMin F and Propolis containing toothpastes on dentinal tubule occlusion with and without the use of an adjunct 810 nm Diode Laser. Forty-five freshly extracted teeth were extracted of which thirty were sectioned into halves and divided into four test groups BioMin F, Propolis, BioMin F + Laser, and Propolis + Laser and control group. All the specimens were treated twice a day for 7 days and then evaluated under scanning electron microscope for partial and complete dentinal tubule occlusion | A significantly higher number of completely occluded tubules were seen in BioMin F + laser group followed by Propolis + laser, Biomin F, and Propolis. A combination approach of desensitizing agent and laser provided a better result than the desensitizing agent alone and when compared individually Biomin F was a more effective desensitizer as compared to Propolis. |
|
6 |
Chen et al. 2023 |
The crowns of 23 extracted sound teeth were removed leaving their roots only. Subsequently, each root was divided into four parts. A total of 15 sound root dentine (SRD) was left untreated as baseline. The ARCLs were developed for the remaining roots using a demineralisation solution (pH-4.8). 15-ARCLs samples were then left untreated. The rest of samples were divided into four groups (n=15 each) and treated with Group-1(BG with 540 ppm-F); Group-2(5000 ppm-F); Group-3(1450 ppm-F) and Group-4(deionised water) | All toothpastes were promising in fluorapatite formation. BG with a 540 ppm-F toothpaste released more ions (Ca2+and P) and reharden the artificial root carious lesions when compared to other groups. However, 1450 ppm-F toothpaste showed more fluoride- substituted apatite formation whereas 5000 ppm-F toothpaste had more fluorapatite formation. |
|
7 |
Ergucu et al 2023 |
This study investigated the application of toothpaste either containing calcium sodium phospho- silicate bioglass (NovaMin) or calcium fluorosilicate bioglass (BioMinF) on the surface mineral composition and morphology of enamel after bleaching procedure. Thirty extracted noncarious human teeth were allocated into five groups (n=6). Group 1: Bleaching using 40% hydrogen peroxide (HP) and fluoridated toothpaste containing bioactive glass (1450 ppm fluoride). Group 2: Bleaching using 40%HP and toothpaste containing calcium fluorosilicate bioglass (540 ppm fluoride). Group 3: Bleaching using 40%HP and fluoridated toothpaste (1450 ppm fluoride). Group 4: Bleaching alone using 40%HP. Group 5: Negative control with distilled water alone. | Within the limitations of this laboratory-based study, there was no significant decrease in the Ca%, P% values and surface properties of enamel after the bleaching procedure following the use of different formulations of toothpastes for a period of 45 days. However, the Ca% and P% values were significantly high for the toothpaste containing calcium fluorosilicate bioglass (BioMinF) on the bleached enamel. |
|
8 |
Chen et al. 2024 |
The aim of this study was to investigate the potential mineral exchange and fluorapatite formation within artificial root carious lesions (ARCLs) using different toothpastes containing 5,000 ppm F, 1,450 ppm F or bioactive glass (BG) with 540 ppm F. The crowns of three extracted sound tooth were removed. The remaining roots were divided into four parts (n = 12). Each sample was randomly allocated into one of four groups: Group 1 (Deionised water); Group 2 (BG with 540 ppm F); Group 3 (1,450 ppm F) and Group 4 (5,000 ppm F). | Within the limitation of this laboratory-based study, all toothpastes were potentially effective to increase the mineral density of artificial root caries on the surface, however there was evidence of mineral loss within the subsurface for Groups 1(Deionised water), 3 (1,450 ppm F) and 4 (5,000 ppm F). |
|
9 |
Doura Alomari et al 2024 |
This in vitro study was accomplished to demonstrate the antibacterial efficacy of BioMin F and NovaMin toothpastes against the recently isolated Streptococcus Mutans in comparison with a commonly used fluoride toothpaste. |
BioMin F toothpaste showed superior antibacterial effect against Streptococcus mutans to Signal and NovaMin toothpastes.
Novamin showed the lowest antibacterial effect. This in vitro study suggests that BioMin F toothpaste shows encouraging potential to be recommended as a preventive measure to reduce the caries risk. |
|
10 |
Eldeeb et al. 2024 |
This in vitro study was conducted to assess the combined effect of Biomin F toothpaste and Diode laser on remineralization of white spot lesions. 30 premolars were divided into three groups: Group A (Biomin F Toothpaste), Group B (Biomin F with laser application for 30 sec), Group C (Negative control) | Within the limitation of the present study, we concluded that Biomin F toothpaste is promising in the repairing of white spot lesions on the surface of the demineralized enamel. Th diode laser did not affect the remineralizing ability of Biomin F toothpaste. |
|
11 |
Thoutam et al 2024 |
To assess and compare the remineralization potential of Elsenz™ and Shy-NM™ toothpaste on artificially induced carious lesions on permanent teeth, using the Vickers microhardness measuring method and scanning electron microscope (SEM) connected to energy dispersive X-ray analysis after laboratory stimulation of the oral environment employing the pH cycling model. A total of 30 sound human premolar teeth were divided into six groups for both parameters. Group I-Elsenz™ toothpaste, group II-Shy-NM™ toothpaste, and group III-control. | Within the scope of this study, the incorporation of fluoride in bioactive glass (BAG) in Elsenz™ had the potential to remineralize enamel better than Shy-NM™ toothpaste. It can, therefore, be concluded that Elsenz™, when compared with Shy-NM™, would be effective in inhibiting demineralization. |
|
12 |
Poopirom et al. 2025 |
This study aimed to compare the remineralization effect of a fluoride bioactive glass (FBG) toothpaste with different concentrations of sodium fluoride toothpaste based on the surface microhardness (SMH) in artificial enamel carious lesions of primary teeth. Fifty sound primary incisors were allocated into five groups (n=10): Group DI (deionized water); Group FBG (Biomin® F); Group 500 ppmF (Jordan®); Group 1000 ppmF (Kodomo®); and Group 1500 ppmF (Systema®) | The remineralization effect of the FBG toothpaste was comparable to that of 1500 ppmF toothpaste and had a greater efficacy than those of 500 and 1000 ppmF based on SMH testing on enamel carious lesions in primary teeth. It offers an effective alternative option for toothpaste with a lower risk of systemic fluoride toxicity, offering a safer, effective option for caries prevention in children. |
Comparative Clinical Efficacy
Immediate Effects (1 Minute – 24 Hours)
To evaluate the immediate effects of BioMin F toothpastes on DH reduction Arshad et al. demonstrated that at immediate application of one minute, when BioMin was applied. The first post-treatment measures were accessed using the Schiff Cold Air Sensitivity Score (SCASS) and VAS scores, where the group BioMin F displayed a reduction of 18.1% in the mean SCASS score compared to the baseline [17]. Whereas there was a greater reduction of 45.7% with Pro-Argin™ and strontium acetate showed the lowest reduction at 8%. These results indicated that Pro-Argin™ provided the most immediate relief within one minute of application indicating it was the most effective for rapid symptom relief compared to BioMin F, although BioMin F demonstrated a lower immediate reduction in DH compared to the other toothpastes within the first minute, its longer exposure to saliva significantly enhances its effectiveness. This observation was supported by the results from Da Cruz et al., which showed that after one hour of immersion in artificial saliva, BioMin F exhibited almost complete dentinal tubule occlusion (Figure 1).
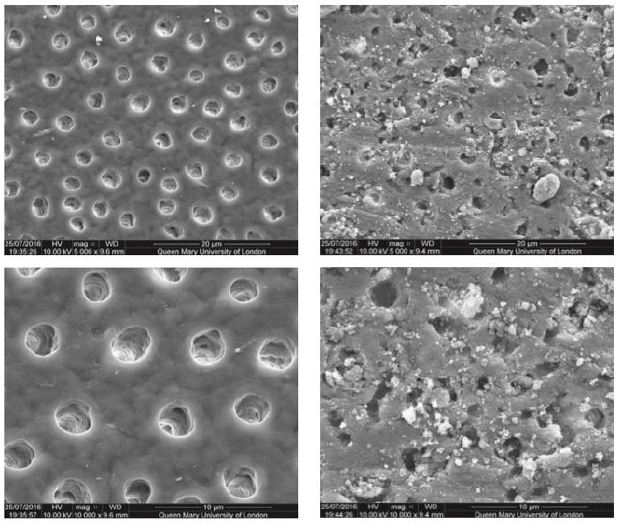
Figure 1: SEM images of dentine before and after BioMin F treatment. At 5000× (top) and 10,000× (bottom) magnifications, control images (left) show open dentinal tubules, while the images on the right are treated with BioMin F followed by 1-hour immersion Adapted from Da Cruz et al. (2018).
Short-Term Effects and Long-Term Effects
Hussain et al. [18] conducted a study comparing the efficacy of a 5% fluoro-calcium phosphosilicate (FCPS) toothpaste compared with a calcium sodium phosphosilicate (NovaMin) and a fluoride- based toothpaste in managing DH. The study assessed VAS scores at 15 days, 30 days, and 60 days, with results demonstrating BioMin F’s superior short-term effects. By 15 days, there was a greater reduction in mean VAS score for the FCPS group when compared to the calcium sodium phosphosilicate and fluoride group, with patients reporting immediate improvement in sensitivity to thermal stimuli. By way of comparison, Hamouda et al. evaluated the efficacy of BioMin F toothpaste in the management of DH in patients with non-carious cervical lesions (NCCL). The study compared BioMin F with other specialist desensitising agents over a 12-week period. DH reduction was assessed using the Schiff Cold Air Sensitivity Scale (SCASS) Scores, VAS and Scanning Electron Microscopy (SEM) to evaluate tubule occlusion. Interestingly at the 3-week interval the group using BioMin F showed only a slight reduction in hypersensitivity, with VAS scores and SCASS score remaining comparable to the baseline. The mean SCASS score remained the same at 2.14, while the mean VAS score showed a marginal decrease from 4.71 to 4.14. The SEM analysis revealed at three weeks there was partial occlusion of tubules with 50% occlusion. However, at six weeks there was a notable difference to the baseline scores for BioMin F with SCASS scores decreasing significantly to 0.71 and VAS scores decreasing to 2.71. With SEM analysis also confirming occlusion of 75% of tubules (Table 5).
Table 5: Summary of selected clinical studies evaluating the effectiveness of Desensitising toothpastes.
|
Study No |
Author |
Study design |
Conclusion |
|
1 |
Gautam, & Halwai, 2017 |
To compare the clinical efficacy of four different commercially available toothpastes in the management of dentinal hypersensitivity. 160 patients clinically diagnosed with dentinal hypersensitivity (93 males and 67 females) participated in this study. The participants were randomly divided into four groups: Group 1 – toothpaste containing 5% potassium nitrate; Group 2 – toothpaste containing 5% fluoro calcium phosphosilicate; Group 3 – toothpaste containing 10% strontium chloride; and Group 4 – a herbal formulation. ie patients’ DH scores for tactile, thermal, and evaporative stimuli were recorded on a visual analogue scale at baseline, 2 weeks, 1 month, and 2 months. |
This study demonstrated that the fluoro calcium phosphosilicate group showed significantly better results compared to either potassium nitrate, strontium chloride, or a herbal toothpaste in reducing dental hypersensitivity symptoms. |
|
2 |
Ashwini et al, 2018 |
Two months’ randomized clinical trial compared the desensitizing efficacy of toothpaste containing 5% fluoro calcium phosphosilicate versus 5% calcium sodium phosphosilicate in participants with sensitive teeth. A total of 60 participants above 18 years of age with a history of DH who displayed a visual analogue scale (VAS) score of ≥ 4 to both subjective and thermal sensitivity in at least two teeth at the qualifying as well as baseline visit were considered eligible. Participants were randomly allocated to one of the following toothpastes: 5% fluoro calcium phosphosilicate; 5% calcium sodium phosphosilicate; and a standard toothpaste containing fluoride. Sensitivity scores (VAS) were measured at baseline, immediately after scaling and root planning, at 15, 30, and at 60 days. | The fluoro calcium phosphosilicate group showed a higher degree of effectiveness in reducing DH, followed by calcium sodium phosphosilicate then standard fluoride toothpastes. Under the conditions of a clinical trial, the fluoro calcium phosphosilicate group showed a comparable reduction in the symptoms of DH. |
|
3. |
Aggarwal et al, 2019 |
This study aimed to evaluate and compare the clinical effectiveness of toothpastes containing fluoro calciumphosphosilicate, calcium sodium phosphosilicate, and strontium chloride hexahydrate for the treatment of dentin hypersensitivity (DH) when applied twice daily.: Participants with a history of DH and with visual analogue scale (VAS) scoreof ≥5 to a painful test stimuli response (dental explorer) in at least one tooth at the qualifying baseline visit were enrolled in this four-week randomized study. Participants (n=93) were randomly allocated to one of the following groups: Group 1––fluoro calciumphosphosilicate (BioMin™), Group 2––calcium sodium phosphosilicate (NovaMin®), and Group 3––strontium chloride hexahydrate. Clinical effectiveness (VAS), perceived sensation score (verbal rating scale [VRS]), participants’ subjective assessment (four-item questionnaire) and oral health-related quality of life (Oral Health Impact Profile-14 [OHIP-14]) questionnaire) were assessed |
Fluoro calcium phosphosilicate bioactive glass containing desensitizing toothpaste treatment may provide better treatment response for the treatment of DH because of its early onset of action in relieving hypersensitivity symptoms as compared with other toothpastes |
|
4. |
Hussain et al, 2019 |
This study was designed as randomized clinical trial to compare the efficacy of Biomin and Novamin in reducing the subjective and provoked (thermal) experience of dentinal hypersensitivity. Sixty subjects were randomly prescribed three toothpastes after oral prophylaxis Group A (20 patients): toothpaste containing 5% fluoro calcium phosphosilicate (Biomin); group B (20 patients): toothpaste e containing 5% calcium sodium phosphosilicate (Novamin); Group C (20 patients): standard toothpaste containing fluoride.
Subjective and thermal sensitivity was assessed using a 10-point VAS score at baseline, at 15 days, 30 days and 60 days of treatment. |
Within the limitations of this study, it can be concluded that flouro calcium phosphosilicate is a promising agent for the management of dentinal hypersensitivity, as evidenced by the earlier reduction in patient perceived as well as objective experience of sensitivity as compared to the conventionally used calcium sodium phosphosilicate. |
|
5 |
Patel et al, 2019 |
A randomised clinical trial compared and evaluated the efficacy of 5% fluorocalcium phosphosilicate with an 8% arginine and calcium carbonate and placebo toothpaste. 75 patients clinically diagnosed with DH were randomly divided into three groups: Group A, 5% fluorocalcium phosphosilicate; Group B, 8% arginine and calcium carbonate; and Group C, placebo. The DH was evaluated by tactile and evaporative stimuli, and a visual analogue scale (VAS) was used for evaporative stimuli at pre-baseline, baseline (15 days) and post-baseline (1 month). |
5% fluorocalcium phosphosilicate showed a better reduction of DH than arginine and calcium carbonate & placebo. The results showed symptoms of DH were reduced in all three groups. However, Group A showed a better reduction of DH than the other two groups. The toothpaste containing 5% fluorocalcium phosphosilicate was reported to be more efficacious than the other two toothpastes in managing DH. |
|
6 |
Reddy et al, 2019 |
To compare the efficacy of four commercially available toothpastes in the treatment of dentinal hypersensitivity (DH). In a single-centered clinical trial, a total of 160 subjects were divided equally into four groups: group 1 – a toothpaste containing 5% fluoro calcium sodium phosphosilicate with fused silica (Biomin); group 2 – a toothpaste containing 5% CSPS (NovaMin); group 3 – herbal formulation; and group 4 – a toothpaste containing 5% potassium nitrate. Patient’s DH scores for tactile, evaporative stimuli were recorded on a visual analogue scale at baseline, 2 weeks, and at the end of 4 weeks. |
All the four desensitizing toothpastes containing different active agents were effective in relieving DH. However, the Biomin group showed a better clinical response at the end of 4 weeks when compared with others. The Biomin group showed significantly better results compared with either NovaMin, herbal, and potassium nitrate toothpastes in the treatment of dental hypersensitivity symptoms. |
|
7 |
Arshad et al, 2021 |
A randomised, controlled, triple-blinded clinical trial was conducted with 140 participants clinically diagnosed with DH and equally randomized into four groups with parallel treatment assignment of FCPS, Pro-Argin™, 8% strontium acetate, and sodium fluoride-based OTC toothpastes, and tested for DH with air blast, mechanical, and water jet stimuli on SCHIFF cold air sensitivity scale (SCASS) and visual analogue scale (VAS) at interim efficacy intervals of one minute, three days, two, four, and six weeks, subsequently. | OTC toothpastes with Pro-argin™ and strontium acetate are effective for immediate pain relief from DH, and FCPS could be the best possible treatment option for long term management of DH. |
Aggarwal et al. [19] conducted a randomised, single-blind clinical study to evaluate the effectiveness of BioMin F in reducing DH compared to NovaMin and strontium chloride over a four-week period. At Week 2, BioMin F exhibited a 58.19% reduction in VAS scores, showing greater short-term relief than NovaMin (49.18%) and strontium chloride (52.69%). The results suggested that BioMin F provided faster relief than NovaMin and comparable long-term efficacy to strontium chloride, making it a promising treatment for DH. Saha et al. [20] also compared BioMin F with strontium chloride in dentinal tubule occlusion. The study measured tubule occlusion at Day 7 and Day 14 using SEM. The results at Day 7 for BioMin F alone revealed moderate occlusion, with 33.85% of tubules completely sealed, indicating limited short-term efficacy. However, by Day 14, tubule occlusion had significantly increased to 51.14%, suggesting a progressive remineralisation effect. BioMin F however exhibited lower occlusion compared to strontium chloride (SC), which reached 63.07% occlusion by Day 14) (see also Table 5).
The Arshad et al. (2021) study reported after three days that the BioMin F toothpaste demonstrated a 22.9% reduction in SCASS scores, which is slightly lower than Pro-Argin™ (25.5%) and strontium acetate (24.4%), indicating limited short-term efficacy. However, by week 2, the group using BioMin F observed a significant increase in DH reduction with a 48.9% change from baseline and now exceeding Pro Pro-Argin™ (46.9%) and strontium acetate (37.2%). And similarly for weeks 4 and 6, BioMin F continued to outperform the other dentifrices in DH reduction, reaching 61.1% at the end of the six-week period. Additionally, Patel et al. [21] conducted a randomised clinical trial to evaluate the efficacy of 5% FCPS (BioMin F) in comparison to 8% Pro-Argin and a placebo toothpaste for the management of (DH). After one month of use, BioMin F demonstrated the greatest reduction in DH, with VAS scores decreasing from 5.58 to 0.51, a reduction of 90.86% (Patel et al., 2019). Whereas, Pro-Argin showed moderate improvement, reducing VAS scores from 5.42 to 2.36 (56.46%), while the placebo had minimal effect (5.25 to 4.02), reinforcing the need for active desensitising agents in DH management. Finally, a randomised Controlled Study Trial (RCT) by Reddy et al. [22] reported on BioMin F, NovaMin, herbal-based, and potassium nitrate-based dentifrices for DH reduction over four weeks. At the Week 4 interval, BioMin F demonstrated the greatest reduction in DH, with VAS scores decreasing from 7.58 to 1.74 (76.6%), outperforming NovaMin (61.2%), herbal (37.5%), and potassium nitrate-based toothpaste (27.0%). Similar trends were observed for air blast sensitivity reduction, with BioMin F reducing scores from 8.24 to 2.16 (73.8%) (See also Table 5).
Discussion
The results of this review demonstrate that BioMin F displays a distinct pattern of efficacy in managing DH, characterised by gradually increasing effectiveness over time rather than immediate relief. This temporal pattern supports BioMin F’s proposed mechanism of action and has significant implications for clinical practice particularly in terms of prevention of 1) erosion in DH) and 2) the early carious lesion (white spots) in children and young adults.
Mechanism of Action and Temporal Efficacy Pattern
The comparative analysis of clinical studies reveals a consistent pattern wherein BioMin F demonstrates moderate immediate effectiveness but superior long-term efficacy. This pattern can be explained by examining BioMin F’s unique bioactive glass composition and its interaction with the oral environment.
BioMin F contains calcium, phosphate, and fluoride ions within a phosphosilicate glass matrix, which slowly dissolves in saliva to release these ions at a controlled rate [23]. This is unlike other toothpastes such as Pro-Argin™, which seals exposed dentinal tubules via Arginine- CaCO3 group interactions [24]. Whereas BioMin F requires sustained exposure to the oral environment to achieve maximum efficacy. This may explain the findings of Arshad et al., where BioMin F showed superior efficacy after 6 weeks compared to Pro-Argin in reducing the VAS scores. This outcome aligns with Patel et al., which also reported superior clinical efficacy with BioMin F compared to Pro-Argin™ in reducing air-blast stimulated DH on the VAS scale after one month of application. This suggests that for patients requiring immediate relief, Pro-Argin might be more suitable initial treatment, however, for long term management the effectiveness of BioMin F is significantly enhanced with the remineralisation and long-term occlusion, reinforcing its efficacy over time in DH management. The slow-release mechanism of BioMin F facilitates fluorapatite (FAP) crystals rather than hydroxyapatite (HA) crystals due to the presence of fluoride in its composition. FAP has superior acid resistance compared to carbonated HA, providing longer-lasting protection against DH [25]. This property explains the progressive improvement observed in studies such as Hamouda et al., where SEM analysis showed an increase from 50% tubule occlusion at three weeks to 75% at six weeks.
Gautam and Halwai’s [26] in vivo study further support this claim, who proposed a 4-step mechanism to explain the superiority of 5 % FCPS toothapste: initial chemical bonding of particles to dental structures, controlled dissolution releasing calcium, phosphate and fluoride ions into the oral environment, subsequent precipitation and crystallisation forming FAP crystals, and sustained remineralisation through prolonged fluoride release. This mechanism provides deeper and more complete tubule occlusion through the formation of acid- resistant FAP crystals within the dentinal tubules, creating a more durable and stable barrier against hydrodynamic stimuli compared to other desensitizing agents. A further notable characteristic of BioMin F is the higher phosphate content, with greater content of P₂O₅ compared to conventional bioactive glass material. Mneimne et al. also confirmed that increase in phosphate content results in rapid degradation of the glass lattice and increases the pH in the environment, favouring the formation of FAP crystals rather than fluorite. The results demonstrated that increasing phosphate contents from 1 mol% P₂O₅ to 6 mol%, accelerated the FAP formation from 3 days to 6 hours. Ultimately, this increased deposition of FAP results in improved tubule occlusion thus a faster relief from DH for patients.
Clinical Relevance and Therapeutic Implications
The temporal efficacy pattern of BioMin F has important clinical implications for DH management strategies. The observed delayed onset but superior long-term efficacy suggests that BioMin F may be most appropriate for patients seeking sustained relief rather than immediate symptom management. Hence for patients with acute, severe DH requiring immediate relief, the results from Arshad et al. would indicate that a Pro-Argin™-based toothpaste may be more suitable initial treatment. However, the progressive tubule occlusion demonstrated in SEM analyses across multiple studies suggests that BioMin F not only provides symptomatic relief but also addresses the underlying structural aetiology of DH by physically blocking exposed dentinal tubules. This dual action a) symptomatic relief and b) structural modification represents a comprehensive approach to DH management (Table 5). The studies included in the review would suggest that a Biomin F toothpaste may be beneficial in the management of several clinical conditions such as dentine hypersensitivity, white spot lesions as observed with orthodontic patients (remineralisation). More recently an in vitro study (enamel carious lesions in primary teeth) by Poopirom et [27] compared the remineralization effect of a 530 ppm FBG (Biomin F) 500 ppmF toothpaste to 1000 ppmF and 1500 ppmF (Sodium Fluoride) toothpastes The results indicated that the remineralization effect of the FBG toothpaste was comparable to that of the 1500 ppmF toothpaste and had a greater efficacy than those of the 500 ppmF and 1000 ppmF respectively (based on the surface microhardness (SMH) testing). According to these authors in view of the risk of fluoride toxicity or dental fluorosis in children [28] using a FBG toothpaste may be an alternative option for enhancing remineralization in children (Table 5).
Critical Analysis of Study Limitations
Despite consistent findings demonstrating BioMin F’s efficacy, methodological heterogeneity across studies limits this review. Firstly, the variability in assessment methods, for example Hamouda et al. used multiple stimulation methods including thermal stimuli to assess hypersensitivity, whereas Patel et al. employed VAS for evaluating DH using an air blast stimulus. These variations in stimulus type may significantly influence reported efficacy rates, as different stimuli activate distinct hydrodynamic mechanisms within the dentinal tubules. Another limitation observed was the relatively short time (generally 2 to 6 weeks) intervals used for the follow up period for subjects for most studies and given BioMin F’s gradual formation of FAP crystals over time, longer term studies (>6 months) are required to assess sustained efficacy and long-term benefits. Furthermore, the advantage of the bio- active glass in dissolving faster in an acidic environment enabling the pH to rise towards a neutral pH may be relevant in the prevention of the early carious lesion (white spots) and erosion from dietary acids etc. The studies in this review had relatively small sample sizes and those participants lost to follow up in some studies may also further reduce the sample size, potentially limiting the statistical power and subsequently the outcomes from the studies Finally, evaluating the cost-effectiveness of BioMin F compared to other desensitising agents would aid clinical decision- making especially in resource-limited settings. Future research would therefore, benefit from larger, standardised assessment trials comparing BioMin F directly to other desensitising products over a longer period (>6-8 months) to validate long-term outcomes and the durability of the fluorapatite crystals formed.
Conclusion
The observation from this review indicates that BioMin F exhibits a distinct pattern of efficacy in managing DH, characterised by gradually increasing effectiveness over time rather than immediate relief. This pattern aligns with its proposed mechanism of action involving the slow release of calcium, phosphate, and fluoride ions and the formation of acid-resistant fluorapatite crystals. The clinical implications of these findings suggest that BioMin F may be more appropriate for long-term DH management rather than acute symptom relief. Its superior efficacy in reducing DH over extended periods, as evidenced by multiple clinical studies, positions it as a promising agent for comprehensive DH management. However, methodological limitations in the current evidence base necessitates further research, particularly studies with longer follow-up periods, larger sample sizes, and standardised assessment protocols. Such research would, therefore, enhance our understanding of BioMin F’s long-term efficacy and optimise its clinical application in DH management and remineralisation. In conclusion, while BioMin F demonstrates promising efficacy in managing DH, particularly over extended periods, a more nuanced understanding of its temporal efficacy pattern is essential for optimising its clinical application and maximising patient benefit.
Disclosure
One of the Authors (DG) has one or more patents on bioactive glass formulations as well as cofounder, Non-Executive Director and Clinical Consultant for BioMin Technologies Ltd, UK.
References
- Davari A, Ataei E, Assarzadeh H (2013) Dentin hypersensitivity: etiology, diagnosis and treatment; a literature J Dent (Shiraz) 14: 136-45. [crossref]
- Gillam DG (2021) The Impact of Dentine Hypersensitivity on the Quality of Life: A Clinical Oral Science and Dentistry 4: 1-6.[crossref]
- Zeola LF, Soares PV,Cunha-Cruz J (2019) Prevalence of dentin hypersensitivity: Systematic review and meta-analysis. J Dent, 81: 1-6. [crossref]
- West NX, Sanz M, Lussi A, Bartlett D, Bouchard P, et (2013) Prevalence of dentine hypersensitivity and study of associated factors: A European population-based cross- sectional study. J Dent, 41: 841-851. [crossref]
- Hamouda Y, Elsayed H, Etman W (2021) Biomimetic Mineralization Approach of Dentin Hypersensitivity in Patients with Early Non-Carious Cervical Lesions. Egyptian Dental Journal /Egyptian Dental Journal, 67: 3693-3710.
- Gillam D, Chesters R, Attrill D, Brunton P, Slater M, et al. (2013) Dentine hypersensitivity–guidelines for the management of a common oral health problem. Dent Update 40: 514-6,518-20,523-4. [crossref]
- Schmidlin PR, Sahrmann P (2012) Current management of dentin Clinical Oral Investigations, 17: 55-59.
- Grossman LI (1935) A systematic method for the treatment of hypersensitive J Am Dent Assoc. 22: 592-602.
- Gillam DG (1997) Clinical Trial Designs for Testing of Products for Dentine Hypersensitivity – A Review. Periodontal Abstracts 45: 37-46.[crossref]
- Hill R , Gillam D (2024) Future Strategies for the Development of Desensitising In Dentine Hypersensitivity Advances in Diagnosis, Management, and Treatment.147-172. Springer Nature Switzerland.
- Miglani S, Aggarwal V, Ahuja B (2010) Dentin hypersensitivity: Recent trends in Journal of Conservative Dentistry, 13: 218. [crossref]
- Jang JH, Oh S, Kim HJ, Kim DS (2023) A randomized clinical trial for comparing the efficacy of desensitizing toothpastes on the relief of dentin Scientific Reports, 13.
- Arnold WH, Prange M, Naumova EA (2015) Effectiveness of various toothpastes on dentine tubule occlusion, J Dent, 43: 440-449.[crossref]
- Lavender SA, Petrou I, Heu R, Stranick MA, Cummins D, et (2010) Mode of action studies on a new desensitizing dentifrice containing 8.0% arginine, a high cleaning calcium carbonate system and 1450 ppm fluoride. Am J Dent. Spec No A: 14A-19A. [crossref]
- Da Cruz LPD, Hill RG, Chen X, Gillam DG (2018) Dentine tubule occlusion by novel bioactive Glass-Based toothpastes. International Journal of Dentistry, 1-10. [crossref]
- Samueli A, Hill RG, Gillam DG (2017) Bioactive glasses in the Management of dentine Hypersensitivity: a review. Dental Health Current Research.
- Arshad S, Zaidi SJA, Farooqui WA (2021) Comparative efficacy of BioMin-F, Colgate Sensitive Pro-relief and Sensodyne Rapid Action in relieving dentin hypersensitivity: a randomized controlled BMC Oral Health. [crossref]
- Hussain H, Jan SM, Behal R (2019) CLINICAL COMPARISON OF 5% FLUORO CALCIUM PHOSPHOSILICATE VERSUS 5% CALCIUM SODIUM PHOSPHOSILICATE IN THE TREATMENT OF DENTINAL International Journal of Medical and Biomedical Studies.
- Aggarwal S, Borkar A, Borse N, Acharya A (2019) Comparative evaluation of fluoro calcium phosphosilicate, calcium sodium phosphosilicate, and strontium chloride hexahydrate containing dentifrice for the treatment of dentin hypersensitivity: A randomized single-blind Journal of International Oral Health, 11: 404.
- Saha S, Malagi SK, Abraham DV, Johnson L, Mahilkar S et (2024) ‘Comparative evaluation of the efficacy of strontium chloride and Biomin F with and without diode laser in the treatment of dentinal hypersensitivity: A scanning electron microscopy study’, Journal of Microscopy and Ultrastructure.
- Patel VR, Shettar L, Thakur S, Gillam D, Kamala DN (2019) A randomised clinical trial on the efficacy of 5% fluorocalcium phosphosilicate‐containing novel bioactive glass toothpaste. Journal of Oral Rehabilitation, 46: 1121-1126. [crossref]
- Reddy GV, Surakanti JR, Vemisetty H, Doranala S, Hanumanpally JR, et (2019) Comparative assessment of effectiveness of Biomin, NovaMin, herbal, and potassium nitrate desensitizing agents in the treatment of hypersensitive teeth: A clinical study. Journal of Dr NTR University of Health Sciences, 8: 24.
- Mneimne M, Hill RG, Bushby AJ, Brauer DS (2010) High phosphate content significantly increases apatite formation of fluoride-containing bioactive glasses. Acta Biomaterialia, 7: 1827-1834. [crossref]
- Uraz A, Erol-Simsek O, Pehlivan S, Suludere Z, Bal B (2012) The Efficacy of 8% Arginine-CaCO3 applications on dentine hypersensitivity following periodontal therapy: A clinical and scanning electron microscopic study. Medicina Oral Patología Oral Y Cirugía Bucal,e298-e305. [crossref]
- Brauer DS, Karpukhina N, O’Donnell MD, Law RV, Hill RG (2010) Fluoride- containing bioactive glasses: Effect of glass design and structure on degradation, pH and apatite formation in simulated body Acta Biomaterialia, 6: 3275-3282. [crossref]
- Gautam V, Halwai H (2017) Comparison of clinical efficacy of four dentifrices in the management of dentinal hypersensitivity. INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH, 6.
- Poopirom C, Yimcharoen V, Rirattanapong P (2025) Comparative Analysis of Application of Fluoride Bioactive Glass and Sodium Fluoride Toothpastes for Remineralization of Primary Tooth Enamel J Int Soc Prev Community Dent 15: 34-41.
- Martinez-Mier EA (2012) Fluoride: Its metabolism, toxicity, and role in dental J Evid Based Complement Alternat Med 17: 28-32.