Abstract
Introduction: Sense of smell represents an important system with a great impact on our life, since it allows recognizing the chemical signals from the environment and its direct involving in routine life. The loss of smell leads to a critical issue in patients’ life. The olfactory disfunction is a result set up by many etiologies; from posttraumatic to neurodegenerative disorder. Our study focused on patients afflicted by general post viral olfactory deficiency since they represent the largest number and the etiopathogenesis is related to olfactory mucosa degeneration. Idiopathic anosmia and anosmia related to rhinosinusitis were excluded given the unknown cause and the chronic phlogistic process they related to, respectively.
Objective: Human olfactory processing is determinate by the smell perception of the nasal olfactory epithelium, localized in the upper part of nasal cavities. This precious nervous structure can be damaged by multiples agents such as virus, chemical substances. During the years, olfactory training, with its daily exposures to a range of odorants, proved to be an important means to enhance the olfactory disorder. Patients with post viral olfactory disfunction can improve their impaired smell sense through olfactory training practice to restore its physiological function. The objective of our study is to evaluate the effectiveness of an olfactory training made of two substances, the Hyaluronic Acid (HA) and mint flavor in the treatment of post viral olfactory disfunction.
Methods: 150 patients with olfactory disfunction were enrolled in our study and divided in three groups of 50 each one. The patients underwent to a treatment based of hyaluronic acid, known for its reparation tissue quality, and a precise pure olfactory stimulus represented by the mint flavor to stimulate regeneration of olfactory neurons. Every group was submitted to a precise olfactory therapy (hyaluronic acid, mint flavor solo or the dual combination) for three months, twice a day.
Results: The data display the dual treatment of hyaluronic acid combined with mint improved the impaired olfactory perception by 50% of their optimal value. Hyaluronic acid associated with the pure mint olfactory essence found out to be more effective than the use of both materials alone and have a more valuable statistic data (p < 0.001).
Conclusions: Hyaluronic acid, with high molecular weight and hydrophilic nature, can form viscous water solutions and has uninflammatory properties, while mint oil is well-known to stimulate the olfactory and trigeminal nerve. Our study aimed to evaluate the effectiveness of administrating the two substances in the treatment of post viral olfactory pathologies. We concluded the two substances can be associated in the olfactory training with mostly higher results than the two used alone.
Keywords
Anosmia, Hyposmia, Olfactory training, Hyaluronic acid, Mint
Introduction
An unimpaired sense of smell allows us to perceive the chemical signs the environment is made of, by doing this, the sense contributes to determinate significantly the quality of our lives. One of its main characteristics is focus on the attention toward the hazards and positive items ordinary life is characterized. The smell is considered chemical warning sensor for safety issues, and is directly involved in the social relationships [1].
Nowadays it is well known smell disfunction is increasing with age, with a higher prevalence in male than female. The prevalence of the sense disfunction in the population has been reported between 9,5 and 15,3% [2,3].
As it regards the smell nervous processing, the whole system is based on a single cranial nerve that mediates data from the olfactory neuroepithelium to the brain. Olfactory perception starts at the level of the olfactory epithelium in the olfactory cleft, situated in the nasal cavities. The Olfactory Epithelium (OE) of vertebrates has the property to have a highly regenerative neuroepithelium which is maintained in natural conditions by a population of stem, progenitor and Globose Basal Cells (GBCs). Olfactory Receptor Neurons (ORN) are embedded within the respiratory epithelium and the axons through the cribriform plate. The key to olfactory information processing is based on the action of Olfactory Receptors (OR). All ORN converge in the same site within the bulb, called “glomerulus”. Then the fibers directly project to the pyriform and entorhinal cortices as well as to the amygdalae (“limbic system”), in memory and emotional processing [4]. Several causes, from posttraumatic injury to neurodegenerative disorders, can lead to an impaired smell function; each one with different mechanism, still not completely ruled out. Upper Respiratory Tract Infection (URTI) is one of the leading causes of post viral olfactory impairment. The precise mechanism and harm location are still unknown; nevertheless, a direct damage of the olfactory receptor cells is very likely. The affected patients usually report a spontaneous recovery which might occur within 2 years, but the improvement reported to be modest, and likely in younger patients [5]. No prognostic items predict the clinical outcome and up to now, no effective therapy exists. Despite that, a specific olfactory training, applied twice a day over a period of 3 months at least, emerged as a promising therapy in promoting the olfactory regeneration [5]. The patients with olfactory loss due to general post-infectious disease can have an increase of smell sense with olfactory training [6,7]. The pathophysiological mechanism for successful of smell training is due to involve increased regenerative capacity of neurons as a result of repeated odorant exposure and due to plasticity of the olfactory sensor. The exact mechanism is still unknown, but many studies had demonstrated the increase of the smell identification after the specific training with intense odors such as lemon, mint, and cloves. In fact, a pure olfactory stimulus is well known to increase the perception of the aromatic substance by the receptor in smell area and mint oil is renowned to stimulate the olfactory and trigeminal nerve [8]. Starting from this premises giving a pure olfactory stimulus for the smell training (mint odor) could improve olfactory functions, and its association with another regenerator tissue substance as Hyaluronic Acid (HA) could be able to speed up the recovery of the olfactory damage. The study aimed to evaluate the effectiveness of administrating a dual therapy with hyaluronic acid and a mint olfactory in the treatment of URTI post-viral olfactory disorders.
Methods
It is well known to stimulate regeneration of olfactory neurons; it is necessary to administrate a pure olfactory stimulus as a part of the olfactory training. For this reason, we decided to submit a treatment based on hyaluronic acid which is able to increase tissues reparation to a precise pure olfactory stimulus such as mint odorant. A total of 150 patients affected by post-viral hyposmia-anosmia were enrolled, and they were provided for a treatment based on a randomized in a single blind in the various defined groups. A group of 50 patients underwent a treatment with only hyaluronic acid, a group of 50 patients with hyaluronic acid plus mint and a group of 50 patients with only mint in solution. Patients were given a solution by intranasal nebulization made of ha 0.3% in association with mint 0.1% as pure olfactory essence. They were treated twice daily for a period of 3 months.
Before starting the therapy, every patient underwent an endonasal endoscopy in order to verify the absence of organic obstruction at the level of the olfactory fissures and spheno-ethmoidal recess bilaterally. All patients then underwent the Sniffin Sticks test kit from Dresden university which involves: standard identification test (the patient is exposed for a few seconds to 16 felt-tip pens with different smells and has to choose between 4 possibilities), discrimination test (the discrimination test requires to where three olfactory elements are submitted to him with eyes closed, two equal and one different, he must indicate the one different from the two, identification of the substance is not necessary) and threshold test (used to verify the minimum concentration at which the patient can perceive an olfactory substance). The sum of the scores from the three subtests resulted in the TDI-score (Threshold, Discrimination, and Identification) with a maximum of 48 points. The test was performed before the treatment and after one month of the end of the treatment. The primary end point is given by the number of patients who have recovered the olfactory function (Table 1). The secondary end point (Table 2) is given by:
1) The number of patients with the 50% improvement compared to the basal
2) The number of patients with the 25% improvement from baseline.
The statistical analysis used for the data was Fisher’s Exact Test significant for “adjusted” P-Values less than 0.05.
Our study was approved by ethical committee IARA1202015 – 1.2.2015
Table 1: Analysis of Primary Endpoint
|
Statistical Model Information |
|
| Statistical Test | Fisher’s Exact Test |
| Tails for discrete tests | Two-tailed |
| Strata weights | None |
| P-value adjustment | Permutation |
| Number of resamples | 1000 |
| Seed | 764511 |
Statistical data used for analysis
Table 2: Analysis of 1st Secondary Endpoint
|
Statistical Model Information |
|
| Statistical Test | Fisher’s Exact Test |
| Tails for discrete tests | Two-tailed |
| Strata weights | None |
| P-value adjustment | Permutation |
| Number of resamples | 1000 |
| Seed | 764511 |
Statistical data used for secondary endopoint analysis
Results
All groups are homogenous for gender; age and the time of begin of the pathology (Table 3). The medium age is equal in all three groups of patients. The onset of hyposmia is various from 9 to 11 months. The TDI score before the start of the treatments is from 19 to 22 score. All the patients underwent to the therapy and concluded the cycle of therapy, medical control and Sniffin Sticks test. According to the data analysis, HA in association with the pure mint olfactory essence is more effective to improve olfactory perception by 50% of their optimal value than the use of both treatments alone (Figure 1) and it demonstrated to have a more valuable statistic data (p<0.001).
Table 3: Patients data and result of sniffing stick test
|
Hyluronic alone |
Hyluronic + mint |
Mint alone |
|
| Medium age |
54 |
56 |
56 |
| m/f |
25/25 |
27/23 |
24/26 |
| TDI score before treatment |
20 |
19 |
22 |
| TDI score after treatment |
22 |
31 |
23 |
| Time iposmia begining (month) |
10 |
11 |
9 |
| P-value |
P=0.2 |
P<0.001 |
P=0.198 |
| The medium age of the three groups is uniform.
The age of the three groups is uniform. The beginning of iposmia is similar in the three groups. TDI: The better result is in the group of patients treated with hyaluronic acid plus mint, this is statistically significative. |
|||
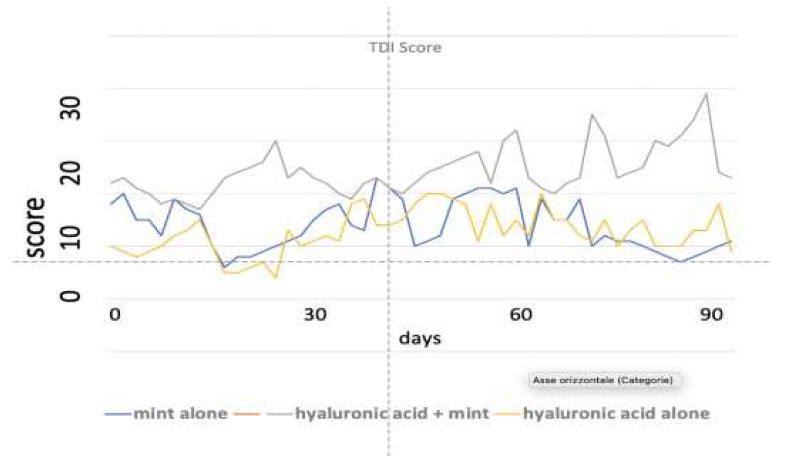
Figure 1: TDI Score.
The value of the TDI of the three groups after therapy. The better results is the group treated with hyluronic acid with mint that results statistical significative p<0.001.
Discussion
Post viral olfactory disorders following Upper Respiratory Tract Infection (URTI) are documented in many studies and typically associated with common cold or influenza. The exact pathogenesis and location of the epithelial damage caused by URTI remains still unclear, even if a damage of the olfactory receptor cells is very likely. The onset of the olfactory disease is typically sudden but many patients delay the medical consultation since they assume the smell deficit is just transient. The olfactory loss is indeed too often underestimated, both from medical and patient points of view. The smell sense is usually considered as a “forgotten sense” and its importance is realized only when it is missing. Furthermore, the diagnosis and treatment of patients come too late in order to be useful to restore proper olfaction’s functionality. For this reason, it is useful to investigate accurately the olfactory loss in every patient referring smell impairment after an URTI episode, so that the damage can be treated as soon as possible. Spontaneous recovery can occur in about one third of patients with postviral olfactory diseases and it is more frequent in younger patients than in the elderly [9]. The individual prognosis is challenging to make and no clinical factors are predictable of a good outcome. It is known the longer the disease has been lasting, the less likely is a recovery, although a timing of 2 years represents the highest chance of recovery [10]. Nowadays, no effective therapy still exists but olfactory training appears to be promising in increasing the regeneration of olfactory function [11]. The olfactory training can be helpful in the recovery of smell loss. The training consists in exposing patients with smell loss with selected odors twice a day for over a period of 12 weeks. The utility of olfactory training in a group of patients with olfactory loss due to post-infectious, posttraumatic or idiopathic etiologies was investigated by Konstantinidis et al. In this study forty of these patients underwent the olfactory training twice-daily with 4 odorants: rose, eucalyptol, lemon, and clove, and they compared the final result, tested with Sniffin Sticks test, with the patients who did not perform olfactory training [12]. They found out the training group significantly improved at 12 weeks, whereas the non-training group did not [12,13]. Even group Geißler et all. demonstrated improved psychophysical test scores following prolonged training (32 weeks) [14]. In a randomized, controlled multicenter study, Damm et al. demonstrate that olfactory training with high odor concentrations resulted in greater improvement than very low odor concentrations [15]. So far olfactory training has gained successful results and suggests it may be a helpful supplement for recovery in patients with smell loss.
As it is known, the damage of smell function is often caused by an injury of the sensory epithelium, the harm, at first, causes alterations in the mucosa and receptors, and often causes alterations of the nerve transmission along the course of the olfactory nerve. The repair of damage in the olfactory area is the first action to be encouraged, keeping in mind that the olfactory area has the intrinsic property of continuously regenerating itself over life’s course. This feature is linked to the presence of a significant amount of stem cells, which have the potential to transform themself into olfactory neurons. Hyaluronic Acid (HA) is an extracellular matrix component consisting of glycosaminoglycans with long polysaccharide chains with molecular weights from 1 kDa up to 8 MDa. HA is produced in the cytoplasmic membrane of mammalian cells by three Hyaluronic Acid Sintetasis HAS membrane enzymes. HAS-1 is responsible for the production of medium to high molecular weight HA (200-2000 kDa), HAS-2 for high molecular weight HA (2000 kDa) and HAS-3 for low molecular weight HA (< 300 kDa) [1,4,7]. HA is continuously extruded through the plasma membrane and it provides a hydrophilic viscous that facilitates cell motility, proliferation and differentiation [5,16]. Its metabolism is regulated by HAS and the plasma concentrations through hyaluronidases enzymes [3,17,18]. The hydrophobic groups and the degree of HA are important for the formation of amphipathic structures to create aggregates in water, generating physical hydrogels [19]. Hydrophobized or crosslink allow HA to have a higher resistance to biodegradation and viscous supplementation [4,20,21]. In literature, many studies had proven the effectiveness of the HA in remodeling the damage of nasal mucosa, facilitating the tissue hydration. In fact, the HA acts as a mucosal lubricant and it is able to influence the nasal bio-mechanical forces, hydric balance, cellular functions, growth factors activity and cytokines behavior. In this way the substance improves the capacity of the cell to carrier the essence to the olfactory area and keep remaining there for longer to stimulate the stem cell to be transform in olfactory receptor [22-24]. It is reported nebulized HA acts positively in determine a significant reduction in nasal exudate and inflammatory cells. It improves the microbiological status, nasal respiratory patency, mucociliary clearance and regulation of mucosal glands secretion in many ENT disorders [25]. HA shown to improve not just the sinonasal symptoms, such as nasal obstruction, but even the olfactory ability in CRSsNP patients [26]. All things considered, HA can be considered effective in modulation of the inflammatory response, being a useful tool for the improvement of reactivation of the normal tissue functions (remodeling) [22-27].
In order to obtain a more successful regeneration of the olfactory tissue, we considered necessary the association of the HA with another substance as a pure olfactory stimulus. For this reason, the dual treatment was created involving HA, capable of accelerating the damage heal at the olfactory level, in association with a precise pure olfactory odorant such as mint odorant. They were submitted to patients as nebulized nasal spray, twice a day. The proposal of our treatment was to stimulate the supposed damaged area of the smell function with an early prompt therapy. The administration of the dual substances improved the olfactory function in the patients group submitted with statistically significant results. For this reason, we can say the synergy action of both elements demonstrated to act in a more effective way than the administration of the solo treatment.
Conclusion
Our study found out the combined action of HA and mint has proven its efficiency in improving the smell functionality in patients with olfactory disfunction after viral damage. Furthermore, nowadays no specific and valid treatment still exists as an option for recovery in these kinds of patients, highlighting the importance of the dual association figured out. Nevertheless, during the years olfactory training emerged as an effective improvement modality with great results in olfactory disease. Therefore, more studies will be necessary to validate this protocol of therapy, such an association with olfactory training.
References
- Stevenson RJ (2010) An initial evaluation of the functions of human olfaction. Chem Senses 35: 3-20. [crossref]
- Murphy C, Schubert CR, Cruickshanks KJ, Klein BE, Klein R, et al. (2002) Prevalence of olfactory impairment in older adults. JAMA 288: 2307-2312. [crossref]
- Nordin S, Brämerson A, Bende M (2004) Prevalence of self-reported poor odor detection sensitivity: the Skövde population-based study. Acta Otolaryngol 124: 1171-1173. [crossref]
- Smith DV, Scott TR (2003) Gustatory neural coding. In: Doty RL, ed. Handbook of Olfaction and Gustation. New York, NY: Marcel Dekker 2003:731-758.
- Duncan HJ, Seiden AM (1995) Long-term follow-up of olfactory loss secondary to head trauma and upper respiratory tract infection. Arch Otolaryngol Head Neck Surg 121: 1183-1187. [crossref]
- Skovbjerg S, Johansen JD, Rasmussen A, Thorsen H, Elberling J (2009) General practitioners’experiences with provision of healthcare to patients with self-reported multiple chemical sensitivity. Scand J Prim Health Care 27: 148-152. [crossref]
- Knaapila A, Tuorila H, Kyvik KO, Wright MJ, Keskitalo K, et al. (2008) Self-ratings of olfactory function reflect odor annoyance rather than olfactory acuity. Laryngoscope 118: 2212-2217. [crossref]
- Moss M, Hewitt S, Moss L, Wesnes K (2008) Modulation of cognitive performance and mood by aromas of peppermint and ylang-ylang Int J Neurosci 118: 59-77. [crossref]
- Hummel T (2000) Perspectives in Olfactory Loss Following Viral Infections of the Upper Respiratory Tract. Arch Otolaryngol Head Neck Surg 126: 802-803. [crossref]
- Reden J, Mueller A, Mueller C, Konstantinidis I, Frasnelli J, Landis BN, Hummel T (2006) Recovery of olfactory function following closed head injury or infections of the upper respiratory tract. Arch Otolaryngol Head Neck Surg 132: 265-269. [crossref]
- Hummel T, Rissom K, Reden J, Hähner A, Weidenbecher M, et al. (2009) Effects of olfactory training in patients with olfactory loss. Laryngoscope 119: 496-499. [crossref]
- Konstantinidis I, et al. (2013) Use of olfactory training in post-traumatic and postinfectious olfactory dysfunction. Laringoscope 123: 2013. [crossref]
- Goodspeed RB, Gent JF, Catalanotto FA (1987) Chemosensory dysfunction. Clinical evaluation results from a taste and smell clinic. Postgrad Med 81: 251-257. [crossref]
- Geissler K, Reimann H, Gudziol H, Bitter T, Guntinas-Lichius O (2014) Olfactory training for patients with olfactory loss after upper respiratory tract infections. Eur Arch Oto- Rhino-Laryngology 271: 1557-1562. [crossref]
- Damm M, Temmel A, Welge-Lüssen A, Eckel H, et al. (2004) Olfactory dysfunctions. Epidemiology and therapy in Germany, Austria and Switzerland. [Article in German] HNO 52: 112-120. [crossref]
- Brämerson A, Johansson L, Ek L, Nordin S, Bende M (2004) Prevalence of olfactory dysfunction: the Skövde population-based study. Laryngoscope 114: 733-737. [crossref]
- Nordin S, Brämerson A (2008) Complaints of olfactory disorders: epidemiology, assessment and clinical implications. Curr Opin Allergy Clin Immunol 8: 10-15. [crossref]
- Shu CH, Hummel T, Lee PL, Chiu CH, Lin SH, et al. (2009) The proportion of self-rated olfactory dysfunction does not change across the life span. Am J Rhinol Allergy 23: 413-416. [crossref]
- Bremner EA, Mainland JD, Khan RM, Sobel N (2003) The prevalence of androstenone anosmia. Chem Senses 28: 423-432. [crossref]
- Tepper BJ (2008) Nutritional implications of genetic taste variation: the role of PROP sensitivity and other taste phenotypes. Annu Rev Nutr 28: 367-388. [crossref]
- Hoffman HJ, Cruickshanks KJ, Davis B (2009) Perspectives on population-based epidemiological studies of olfactory and taste impairment. Ann N Y Acad Sci 1170: 514-530. [crossref]
- Castelnuovo P, Tajana G, Terranova P, Digilio E, Bignami M, et al. (2016) From modeling to remodeling of upper airways: Centrality of hyaluronan (hyaluronic acid). Int J Immunopathol Pharmacol 29: 160-167. [crossref]
- Macchi A, Castelnuovo P, Terranova P, Digilio E (2013) Effects of sodium hyaluronate 9 mg in children with recurrent upper respiratory tract infections: Results from a randomized controlled study. International Journal of Immunology and Pharmacology 26: 127-135. [crossref]
- Macchi A, Gallo S, G.Montrasio, Periolo A, Simoncini D (2017) Anlysys of mucociliar clearance. A new diagnostic methods and therapeutical proposal. The Rhinologist 4: 33. [crossref]
- Pignataro L, Marchisio P, Ibba T, Torretta S (2018) Topically administered hyaluronic acid in the upper airway: A narrative review. Int J Immunopathol Pharmacol 32: 2058738418766739. [crossref]
- Savietto E, Marioni G, Maculan P, Pettorelli A, Scarpa B, et al. (2020) Effectiveness of micronized nasal irrigations with hyaluronic acid/isotonic saline solution in non-polipoid chronic rhinosinusitis: A prospective, randomized, double-blind, controlled study. Am J Otolaryngol 41: 102502. [crossref]
- Isnard N, Legeais JM, Renard G, Robert L (2001) Effect of hyaluronan on MMP expression and activation. Cell Biology International 25: 735-739. [crossref]