Abstract
Introduction: The low-energy Dynamic Quadripolar Radiofrequency or DQRF™ vaginal technology overcomes several problems of manageability and safety experienced with other energy-based vulvovaginal energy-providing technologies by postmenopausal women with symptoms of vulvovaginal atrophy. The proprietary Ultra-Pulsed Radioporation or UPR™ technology has already shown to accrue the benefits of the new radiofrequency technology by facilitating penetration of active principles into the deep layers of vulvar skin and vaginal mucosa and enhancing hydration and trophism. Evaluating the impact on vulvovaginal atrophy symptoms, with vaginal dryness expected to benefit the most from the DQRF/UPR™ synergy, is the goal of this interim study.
Methods: Prospective real-life cohort study on 106 ambulatory women (mean age, 56.8 ± 8.61 years old) with vaginal atrophy and dryness. VVA treatment: four to five 25-min sessions every 14-16 days (coupling gel with hyaluronic acid); one more DQRF/UPR™ maintenance session after six months and a final visit (only assessment, no treatment) after 12 months. Operative temperatures in target tissues during the procedure: 42°C (range 40-43°C). Assessments (baseline and at the end of the treatment cycle): vaginal dryness (primary efficacy parameter, 10-cm impromptu Visual Analogue Scale); dyspareunia, burning and itching (4-score impromptu Likert-like scale) and photographic documentation at baseline at the end of the DQRF/UPR™ treatment cycle.
Results: Vaginal dryness rapidly improved vs baseline (T0), with a highly significant reduction (−83.1%) at the end of the treatment cycle (T1) that steadily persisted after 6 and 12 months (T2 and T3; −79.2% and −64.9%, respectively). All other symptoms similarly improved vs baseline over the year of follow-up: dyspareunia −81.5% (T1) and −70.4% (T3); burning −87.0% (T1) and −65.2% (T3); itching −89.5% (T1) and −68.4% (T3). All treatments were well tolerated, with no troubling pain or other side effects during or after the procedures.
Conclusion: The study confirms, over a one-year follow-up, the previously demonstrated benefits of the Dynamic Quadripolar Radiofrequency (DQRF™) in synergy with Ultra-Pulsed Radioporation (UPR™) as an innovative treatment option of vulvovaginal atrophy/genitourinary syndrome of the menopause symptoms. The novel UPR™ technology facilitates the deep penetration of active topical principles favourably acting on postmenopausal atrophic tissues. The DQRF/UPR™ concept aims to enhance the effects of the DQRF™ technology exploiting the synergy between the double biological effects-by the energy-based DQRF™ and the UPR™ active principle. Long-term studies will confi.
Keywords
Electroporation, Genitourinary syndrome of menopause, Dynamic quadripolar radiofrequency, DQRF™, Ultra-Pulsed Radioporation, UPR™, Vulvovaginal atrophy
Abbreviations
DQRF™: Dynamic Quadripolar Radiofrequency
GSM: Genitourinary Syndrome of Menopause
HA: Hyaluronic Acid
MDa: x106 Dalton
MHz: Megahertz or x106 Hertz
RSS™: Radiofrequency Safety System
SEM: Standard Error of the Mean
UPR™: Ultra-Pulsed Radioporation
VAS: Visual Analogue Scale
VDR™: Vaginal Dynamic Radiofrequency
VVA: Vulvovaginal Atrophy
W: Watt
Introduction
Energy-based vulvovaginal treatment technologies often show manageability and safety difficulties in postmenopausal women with life-disrupting Vulvovaginal Atrophy (VVA) and Genitourinary Syndrome of Menopause (GSM). The low-energy DQRF™ (Dynamic Quadripolar Radiofrequency) technology candidates to overcome such problems in VVA women [1,2]. The four algorithmically controlled radiofrequency electrodes, continuously cycling between receiver and transmitter states (VDR™ or Vaginal Dynamic Radiofrequency™ technology), generate repelling electric fields within the closed electrode system and concentrate their low-energy thermal effects with high topographical precision in precise subepithelial areas without the need for grounding pads.
In addition, the treated area – usually a 4-inch area centred on the hymenal ring -need no systemic analgesia or local anaesthesia thanks to the integrated RSS™ (Radiofrequency Safety System) proprietary technology that steadily tracks the tip movements and local tissue temperature [1,2]. The Novavision Group S.p.A. (Misinto, Monza-Brianza, Italy) holds worldwide rights for the patented DQRF™, VDR™, and RSS™ technologies.
Since 2018, integrating the DQRF™ concept with the proprietary UPR™ (Ultra-Pulsed Radioporation) radiofrequency electroporation technology has been a second technological jump forward. UPR™ modulates the DQRF™ radiofrequency effects and facilitates the transfer of biologically active principles through aqueous channels in vulvar skin and vaginal mucosa cell membranes [3]. The DQRF™ effects on vulvovaginal hypotrophy thus synergise with those of the UPR™-mobilised active principles-for instance, highly hydrating and pro-trophic Hyaluronic Acid (HA) [4]. Counteracting the postmenopausal loss of elasticity and volume with topical HA formulations and HA dermal fillers in women with labia majora hypotrophy has long been a common cosmetic gynaecology practice [5,6]. A double-blind pilot study compared VVA/GSM symptoms and women’s satisfaction with their sexual and couple lives in two random samples of postmenopausal women randomised to either DQRF™ and DQRF/ UPR™ vulvovaginal treatment [3]. The low-molecular-weight HA was interspersed in the coupling gel in the DQRF/ UPR™ treatment group; the study established the DQRF/ UPR™ superior benefits [3].
The interim 12-month DQRF/ UPR™ outcomes on VVA symptoms herein illustrated aim to confirm the previous favourable outcomes over a more extended follow-up period and a more ample postmenopausal women cohort. Vaginal dryness, expected to benefit the most from the UPR™ synergy with DQRF™, was the primary efficacy parameter. The interim DQRF/ UPR™ cohort study herein described is currently being expanded to identify the characteristics of VVA women who will most likely benefit from the advanced DQRF/UPR™ technology.
Methods
Real-life Study Design, Cohort Selection Criteria and Interim Cohort Demographics
All VVA/GSM women enrolled in the prospective DQRF/UPR™ cohort attended specialist departments for postmenopausal disorders in the authors’ private health facilities. Candidate participants in the 45 to 66 years old age range with moderate to severe VVA symptoms (vaginal dryness, itching, burning and dyspareunia) and negative recent Papanicolau and mammography tests should not have reported menstruations for at least 12 months. In addition, they should not have participated in other clinical studies for the last six months. After giving informed consent to the anonymous collection of their data and photographic evidence before the first treatment session, the 106 women underwent their planned DQRF/UPR™ treatment cycle between January 2020 and March 2021. All women had objective evidence of moderate to severe mucosal atrophy with thinning or loss of vaginal rugae and mucosal pallor; an explicit wish for a still-active sexual life was also a must.
Hormonal replacement therapy, pelvic organ prolapses beyond the hymenal ring, vulvodynia or chronic vulvar pain, vulvar dermatitis or dystrophy, viral lesions, including a high risk for human Papillomavirus infections, vaginal infections in the last two months, a Sjögren syndrome diagnosis, and inadequate thickness of the recto-vaginal septum at the pelvic examination-all were exclusion criteria from the study.
All study materials, including informed consent forms and study protocol and case report forms, were peer-reviewed for ethical problems, and the authors always safeguarded the full respect of the ethical standards laid down in the Declaration of Helsinki as revised in Brazil 2013. Participant women also agreed to the publication of the study outcomes.
Operative Procedures
The DQRF™-based EVA™ device (Novavision Group S.p.A., Misinto, Monza-Brianza, Italy) and the proprietary UPR™ technology were previously described [1-3]. The protocol foresaw 4 to 5 treatment sessions spaced 14-16 days as a treatment cycle. First, power was applied for 15 minutes to the vaginal mucosa with hyaluronic acid (1.5 to 2.0 MDa, 0, 2% concentration) mixed with the coupling gel, starting behind the hymenal ring with circular back-and-forth continuous movements and always keeping contact between the tip probe and the mucosa. Then followed another 10 minutes of DQRF™ application for vulvar treatment: in both steps with the power of the EVA™ device set at 20% to 27% of the 55-W maximum emitting power. Previous preparation was limited to an alcohol-free cleanse; all procedures were performed with the woman on the examining table in the dorsal lithotomy position.
With particular attention to pain and discomfort, safety was investigated in all women at each study visit and by telephone over the following days. The treatment protocol foresaw a further DQRF/UPR™ maintenance session after six months and a final visit (only assessment, no treatment) after 12 months. Figure 1 illustrates the sterilisable vaginal and vulvar DQRF™ tips with their medically certified AISI 316 stainless steel dynamic quadripolar electrodes. The electrodes continuously cycle between receiver and transmitter states; the generated active electric fields in subepithelial tissues minimise the delivered energy (only 11 to 15 W), tissue Ohm’s resistances and untoward thermal side effects with the help of the RSS™ safety technology.
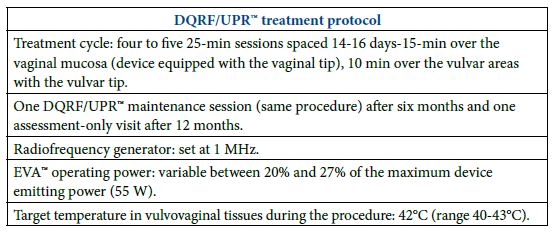

Figure 1: On the left: the EVA™ vaginal tip with the four emitters/receivers DQRF™ electrodes distributed longitudinally to adapt to the vaginal anatomy. On the right: the EVA™ vulvar tip with the four DQRF™ electrodes distributed on the terminal tip plane to adapt ergonomically to the vulvar areas.
Assessments
Vaginal dryness was assessed before the first treatment session (baseline, T0) and at the end of the treatment cycle (T1), together with baseline and end-of-treatment photographs, with the help of a 10-cm impromptu Visual Analogue Scale (VAS). Assessments of itching, burning, and dyspareunia made use of impromptu 4-score Likert-like scales (0=none; 1=mild; 2=moderate; 3= severe), with semi-quantitative score assessments repeated at the two follow-up visits: after 6 and 12 months (T2 and T3, respectively). In addition, all participant women received a Pap-test and a transvaginal echography as further safety control at all visits up to T3.
Statistics
Descriptive data were tabulated as means ± standard errors of the mean. The non-continuous nature of the VAS (vaginal dryness) and Likert-like (other VVA symptoms) semi-quantitative scores and the lack of assumptions about the normal distribution of baseline and final data justified a conservative approach. The general linear model for repeated measures or Kruskal-Wallis test for independent samples (nonparametric one-way ANOVA test) was applied to scores, after correction of means for age and Body Mass Index, to assess for any DQRF/UPR™ effect, with two-sided 95% confidence levels and p <0.05 as a cut-off for significance. Using the nonparametric one-way ANOVA test was justified because the score variances were homogeneous at the Levene’s test. After detecting a significant DQRF/UPR™ effect, pairwise post-hoc Sidak multiple comparisons identified the exact time points of score trend divergence vs baseline during the T1 to T3 period.
Results
Table 1 illustrates the cohort demographics before the first treatment session. The clinical severity of the mail efficacy parameter, vaginal dryness, was alarming for most of the cohort VVA women (56.8 ± 8.61 years old), as highlighted by the high baseline VAS score and the low dispersion of baseline VAS scores (mean ± SEM, 7.7 ± 0.49). All other VVA symptoms were also quite troubling, as shown by the concentration of baseline scores for dyspareunia, but also burning and itching, in the “Moderate” (score 2) and “Severe” (score 3) groups. The baseline scores for dyspareunia and vaginal burning and itching were 2.7 ± 0.56, 2.3 ± 0.475 and 1.9 ± 0.88, respectively, in an impromptu 0-3 Likert-like scale. All women reported dyspareunia at baseline, and almost all intimate burning and itching.
Table 1: DQRF/UPR™ cohort demographics and baseline symptom profile. SEM, standard error of the mean.
|
Baseline Prospective Cohort Data |
||||
| Postmenopausal women (N) |
106 |
|||
| Age (years, mean ± SEM) |
56.8 ± 8.61 |
|||
| Vaginal dryness (VAS scale ± SEM) |
7.7 ± 1.35 |
|||
|
Other VVA symptoms |
Absent |
Mild | Moderate |
Severe |
| Dyspareunia (cohort per cent) |
0 |
5 | 22 |
74 |
| Burning (cohort per cent) |
1 |
14 | 39 |
46 |
| Itching (cohort per cent) |
4 |
32 | 34 |
30 |
Sixty-three women underwent four DQRF/UPR™ sessions, 43 women five treatment sessions. All participant women completed their DQRF/UPR™ treatment program as planned without missing visits and described their experience as always comfortable. All treatments were well tolerated, with no troubling pain, burns or blisters or other fastidious side effects or complications during or after the procedures. All women also resumed their everyday activities and sexual life immediately after the end of their treatment program.
The primary efficacy parameter, vaginal dryness, markedly improved at the end of the DQRF/UPR™ treatment cycle with the relevant VAS score already diverging from the null hypothesis of no-effect trend (mean ± SEM, 1.3 ± 1.35, −83.1% and p <0.001 vs baseline), with 41 women reporting total subjective relief with a zero score for dryness. Furthermore, the benefits for vaginal dryness steadily persisted six months after the end of the treatment cycle (median VAS score 1.0; mean 1.6 ± 1.41, −79.2% and p <0.001 vs baseline) and only slightly deteriorated after 12 months of no DQRF/UPR™ sessions (median 3.0; mean 2.7 ± 1.44, −64.9% and p <0.001 vs baseline) (Figure 2). However, after 12 months, five women still reported no vaginal dryness and 15 only a mild dryness (Figures 3 and 4).
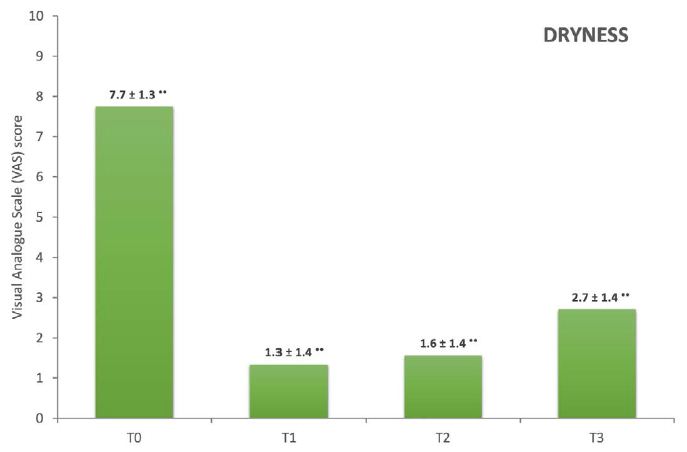
•• p <0.001 vs baseline.
Figure 2: Vaginal dryness VAS scores at T0 (baseline), T1 (after the end of the DQRF/UPR™ treatment cycle), T2 (maintenance and assessment visit after six months), T3 (assessment visit after 12 months); means ± standard errors of the mean.

Figure 3: Per cent distribution of the symptom severity scores at baseline (T0), end of the DQRF/UPR™ treatment cycle (T1), and follow-up visits after 6 and 12 months (T2 and T3, respectively).

Figure 4: Vestibular atrophy at the end of the DQRF/UPR™ cycle, with the evidence of new vestibular rugae as morphological markers of the treatment benefits.
The benefits at T1 were similar for other VVA symptoms (Table 2): dyspareunia −81.5%, burning −87.0%, itching −89.5% vs baseline, all of them already diverging at T1 with high significance from the null hypothesis of no-effect trend.
Table 2: Dyspareunia, burning and itching scores (0-3 Likert-like scales) after the 4-5 DQRF/UPR™ treatment sessions. ••p<0.001 vs. baseline; means ± standard errors of the mean.
|
VVA Symptom |
End of the DQRF/UPR™ treatment cycle (T1) |
|
| Dyspareunia |
0.5 ± 0.52•• (median 0) |
56 women reporting no dyspareunia |
| Burning |
0.3 ± 0.52•• (median 0) |
70 women reporting no vulvovaginal burning |
| Itching |
0.2 ± 0.41•• (median 0) |
84 women reporting no vulvovaginal itching |
The dyspareunia, burning and itching scores also remained steady at the maintenance visit after six months and only marginally deteriorated after 12 months (Table 3). However, the vaginal dryness VAS score was still 64.9% lower than baseline after one year, whilst the dyspareunia and vaginal burning and itching subjective scores were 70.4%, 65.2% and 68.4% lower.
Table 3: VVA severity scores (0-3 Likert-like scales) at the maintenance/assessment visit six months after the end of the DQRF/UPT™ treatment cycle (T2) and the final assessment follow-up after 12 months. ••p<0.001 vs. baseline; means ± standard errors of the mean.
|
VVA symptom |
T2 |
T3 |
| Dyspareunia |
0.5 ± 0.62•• (median 0) |
0.8 ± 0.73•• (median 1) |
| Burning |
0.5 ± 0.62•• (median 0) |
0.8 ± 0.70•• (median 1) |
| Itching |
0.4 ± 0.57•• (median 0) |
0.6 ± 0.68•• (median 0) |
Discussion
The DQRF™-induced variable electrical currents continuously re-orient dipole moments like water molecules in target vulvovaginal tissues. Other biomolecules, facing variable electric impedance and mechanical attrition due to the water viscosity, dissipate their Brownian kinetic energy into heat [7].
Over the years, more and more evidence has highlighted how thermal energy conveyed to vulvovaginal tissue may help reverse the natural ageing processes by stimulating the proliferation of glycogen-enriched epithelium new vessels and collagen formation in the lamina propria and by improving natural lubrication and urination control [7]. The 40°C to 43°C temperature range is critical to activate neocollagenesis by tissue fibroblasts [8].
The burden of bleeding, pain and burning problems may be severe for laser devices [9]. The digitally controlled DQRF™ technology helps to reduce the related discomfort, while the synergy with the UPR™ technology helps the in-depth penetration of hydrating and pro-trophic agents in treated vulvovaginal areas [3].
The study confirms the short-term outcomes of the first DQRF/UPR™ double-blind study over a longer one-year follow-up. The double-blind study already established the UPR™ contribution acting in synergy with the DQRF™ technology [3].
Although the baseline vaginal dryness and overall cohort VVA symptom profile appeared quite severe, most cohort women reported T1 reductions of baseline symptom scores between -81.5% and -89.5%-quite impressive after the relatively short DQRF/UPR™ treatment cycle, at most no more than about 80 days. Indeed, some caution is justified: together with the uncontrolled design, assessing symptom relief from VVA symptoms only through impromptu, non-validated VAS and Likert-like subjective scales is a weak point that deserves consideration before hasty conclusions.
Besides physical discomfort, VVA symptoms may severely affect the postmenopausal woman’s self-perception [10-12]. In clinical situations where even minor clinical improvements may translate into significant perceived relief, benefits may appear magnified due to the placebo effect. Psychological and self-rated measures, mainly if assessed via subjective semi-quantitative scores, are primarily liable to placebo effects-as in this study.
However, the study intended only to confirm the benefits of the DQRF/UPR™ VVA treatment option, which the double-blind trial demonstrated [3], over a one-year follow-up, and its value is unaffected. On the contrary, the study provides new clinically significant information-the subjective VVA benefits persist for one year after a relatively short, four-to-five session treatment cycle, with VVA symptom severity scores still -64.9% and -70.4% vs baseline after twelve months. Interestingly, dyspareunia showed the most remarkable long-term improvement, indirectly highlighting the importance of a gratifying sexual life for the cohort’s postmenopausal women. The open-label nature of the study cannot contribute to defining the contributing role of in-depth radioporation of the lenitive and possibly pro-trophic glucose-hyaluronic acid gel. However, the previous double-blind investigation already demonstrated the DQRF™ and UPR™ synergy [3].
Of course, further long-term studies will confirm these preliminary encouraging results.
Conclusion
The study confirms, over a one-year follow-up, the benefits, previously demonstrated in a double-blind trial, of the Dynamic Quadripolar Radiofrequency (DQRF™) in synergy with Ultra-Pulsed Radioporation (UPR™) of hydrating and pro-trophic hyaluronic acid as an innovative treatment option of the vulvovaginal atrophy, and in the general genitourinary syndrome of the menopause symptoms.
Acknowledgement
The authors declare they have no financial or any other conflict of interest related to the study or the issues discussed in the paper.
References
- Vicariotto F, De Seta F, Faoro V, Raichi M (2017) Dynamic quadripolar radiofrequency treatment of vaginal laxity/menopausal vulvo-vaginal atrophy: 12-month efficacy and safety. Minerva Ginecol 69: 342-349. [crossref]
- Vicariotto F, Raichi M (2016) Technological evolution in the radiofrequency treatment of vaginal laxity and menopausal vulvo-vaginal atrophy and other genitourinary symptoms: first experiences with a novel dynamic quadripolar device. Minerva Ginecol 68: 225-236. [crossref]
- Tranchini R, Raichi M (2018) Ultra-Pulsed Radioporation further enhances the efficacy of Dynamic Quadripolar Radiofrequency in women with post-menopausal vulvo-vaginal atrophy. Clin Obstet Gynecol Reprod Med 4: 1-5.
- Landau M, Fagien S (2015) Science of hyaluronic acid beyond filling: fibroblasts and their response to the extracellular matrix. Plast Reconstr Surg 136: 188S-195S. [crossref]
- Fasola E, Gazzola R (2016) Labia majora augmentation with hyaluronic acid filler: technique and results. Aesthet Surg J 36: 1155-1163. [crossref]
- Tadir Y, Gaspar A, Lev-Sagie A, Alexiades M, Alinsod R, et al. (2017) Light and energy-based therapeutics for genitourinary syndrome of menopause: Consensus and controversies. Lasers Surg Med 49: 137-159. [crossref]
- Dunbar SW, Goldberg DJ (2015) Radiofrequency in cosmetic dermatology: an update. J Drugs Dermatol 14: 1229-1238. [crossref]
- Gaspar A, Addamo G, Brandi H (2011) Vaginal fractional CO2 laser: a minimally invasive option for vaginal rejuvenation. Am J Cosmetic Surg 28: 156-162.
- Beasley KL, Weiss RA (2014) Radiofrequency in cosmetic dermatology. Dermatol Clin 32: 79-90. [crossref]
- Alexiades M, Berube D (2015) Randomized, blinded, 3-arm clinical trial assessing optimal temperature and duration for treatment with minimally invasive fractional radiofrequency. Dermatol Surg 41: 623-632. [crossref]
- Nappi RE, Martini E, Cucinella L, Martella S, Tiranini L, et al. (2019) Addressing vulvovaginal atrophy (VVA)/Genitourinary Syndrome of Menopause (GSM) for healthy aging in women. Front Endocrinol (Lausanne) 10: 561. [crossref]
- Oken BS (2008) Placebo effects: clinical aspects and neurobiology. Brain 131: 2812-2823. [crossref]