Abstract
This study was designed to determine the awareness and knowledge levels of male patients about HPV and the HPV vaccine. This study was planned as a single-center, descriptive and cross-sectional study. This cross-sectional study included 255 patients who presented to the Family Medicine Polyclinic at Tekirdağ Namık Kemal University Hospital. Data were collected between 01.07.2023 and 01.12.2023 with a face-to-face survey form. The content of the survey form included questions about the participants, a survey assessing awareness and knowledge regarding HPV and the HPV vaccine, which we prepared by scanning the literature and whose content validity index was 0.98. The data obtained were evaluated in the 152 (59.6%) of the men stated that they did not have information about HPV, 250 (98.0%) stated that they had not received the HPV vaccine, 102 (40.0%) stated that they did not consider getting the HPV vaccine, and 144 (56,5%) stated they thought it was difficult to access the HPV vaccine. The median (min-max) score of the men in the study group from the survey was 24.0 (6.0-32.0) and the mean (SD) was 23.20. The findings of this study showed that more than half of the men had not heard of the HPV vaccine, almost all of the men had not received the HPV vaccine, and the majority thought it was difficult to access the vaccine. However, men’s general HPV knowledge was average and their knowledge of the current HPV vaccination program was low. In addition, men’s awareness and knowledge survey scores about HPV and the HPV vaccine were at an average level, and HPV knowledge affected men’s attitudes and behaviors. It may be recommended to take initiatives to increase men’s knowledge about general HPV and the HPV vaccine.
Keywords
Man, HPV, HPV vaccine, Knowledge level, Awareness
Introduction
Human Papilloma Virus (HPV) is a DNA virus belonging to the Papillomavirinae family. HPV infects the basal epithelial layer cells of human skin and mucosal surfaces. This virus is a non-enveloped, double-stranded circular DNA virus. The genome of HPV is approximately 8 kilobase pairs long. The replication cycle of HPV is a very slow process. There can be a long period between the onset of HPV infection and the appearance of symptoms, and this period can vary from person to person. It can take weeks or even months from the moment the infection begins to appear for symptoms to appear. HPV can be transmitted directly from cracks in the skin and mucosa, as well as during sexual intercourse. In addition, HPV can be transmitted indirectly from contaminated surfaces (fomites) of shared bathroom floors, towels, clothing or personal belongings, and from the mother to the newborn during birth through the infected birth canal [1-3]. HPV is a common sexually transmitted infection worldwide. There are many different types of HPV, and most types of the virus do not cause any symptoms or health problems in the infected person; however, a small percentage of infections caused by certain types of HPV can persist and cause clinically significant disease. HPV types are classified according to their epidemiological association with cancer. Low-risk HPV types can also cause genital warts and a rare condition called recurrent respiratory papillomatosis. High-risk HPV types are associated with a variety of cancers, including cervical, anal, penile, vaginal, vulvar, and head and neck. Different vaccines have been developed for HPV vaccination, and there are currently three vaccines: bivalent (HPV types 16 and 18), quadrivalent (HPV types 6, 11, 16, and 18), and nonavalent (HPV types 6, 11, 16, 18, 31, 33, 45, 52, and 58). Each HPV vaccine has been shown to be safe and effective against the HPV strains involved [3-6]. HPV vaccines are used as part of national vaccination programs in the United States, Australia, and many European countries. The fact that HPV vaccines are not included in national vaccination programs and are not covered by health insurance affects access to the vaccine and vaccination rates. Parental knowledge, mentality, and income levels affect whether HPV vaccines are widely used. Increasing resistance to vaccination can make it difficult for vaccines to be accepted and implemented in society [5-7]. HPV research generally focuses on understanding the development of cervical cancer and precancerous lesions, as well as how to prevent and control these conditions. This research focuses particularly on women’s health and the prevention of cervical cancer. The administration of HPV vaccines to women has been seen as an effective strategy for preventing cervical cancer. Recent studies have shown that HPV-related cancers pose a significant burden not only to women but also to men. In addition to HPV being linked to cervical cancer in women, HPV infections in areas such as the anus, oral cavity, and oropharynx pose a serious cancer risk in men [8-10]. HPV infections have now become preventable thanks to HPV vaccines. Countries can increase cancer prevention by expanding such vaccines through vaccination programs [1-4]. The aim of this study was to assess the knowledge and behaviors of men aged 18-45 about HPV and the HPV vaccine.
Material and Methods
This study is a cross-sectional descriptive survey. In order to evaluate the level of knowledge and behavior about HPV and HPV vaccine among male patients aged 18-45 who applied to Tekirdağ Namık Kemal University Hospital Family Medicine Outpatient Clinic between July 1, 2023 and December 1, 2023, the Adult Vaccination Knowledge Level Survey consisting of 16 questions was applied on a voluntary basis. Data from a total of 255 participants were analyzed. Before starting the study, approval was obtained from the Namık Kemal University Faculty of Medicine Ethics Committee (protocol no: 223.129.06.15).
Criteria for Including Participants in the Study
- Being between the ages of 18-45
- Having applied to Tekirdağ Namık Kemal University Hospital Family Medicine Polyclinic center
- Being male
- Having mental competence
- Being a volunteer
Criteria for Exclusion of Volunteers from the Study
- Being under the age of 18 and over the age of 45,
- Not having mental competence
- Being a woman
A questionnaire form prepared by the researcher based on literature review at the time of application, which questioned the sociodemographic data of the patients, their knowledge level and behaviors about HPV and HPV vaccine, was filled out by the volunteers.
Validity and Reliability of the Awareness and Knowledge Questionnaire on HPV and HPV Vaccine
A total of 16 items were created to measure awareness and knowledge levels on HPV and HPV vaccine in line with the literature. The suitability and comprehensibility of each scale item was assessed by 10 experts (1 internal medicine, 4 family physicians, 1 emergency, 1 public health, 1 infection, 1 dermatology and 1 gynecology and obstetrics). The experts were asked to evaluate the items in three groups as “important”, “useful but insufficient”, and “unnecessary”. The scope validity rates of the scale ranged from 0.8 to 1.0 and the scope validity index was 0.98.
The Adult Vaccination Knowledge Level Questionnaire, which was created to assess the knowledge level, consists of 16 questions. Factor analysis was used for structural validity. It was performed using Principal Component Analysis (PCA) with Varimax rotation. PCA generally tests the psychometric qualities of structured questionnaires and is a frequently used multivariate statistical technique and is used to determine the structure . The reliability levels expressed by the Cronbach alpha coefficient range were taken into account in the study. For the reliability analyses of the scale, it was calculated again according to the Cronbach alpha coefficient and item total correlation. In the factor analysis, Kaiser-Meyer-Olkin: 0.875, Barlett’s test result was p<0.001. Factor loadings below 0.30 varied between 0.302-0.812, and it was determined that the items collected in a single sub-domain explained 31.63% of the total variance. Cronbach alpha value was determined as 0.814. The item total correlation values for the items in the questionnaire varied between 0.201-0.714. For confirmatory factor analysis, goodness of fit statistic (GFI), adjusted goodness of fit statistic (AGFI), CFI (Comparative fit index), Normed fit index (NFI), Incremental Fit Index (IFI), Relative Fit Index (RFI), Parsimony Fit Index (PNFI), Root Mean Square Error of Approximation (RMSEA) and Standardized Root Mean Square Residual (SRMR) indices were calculated. For the acceptability levels of fit indices, CFI, NFI, IFI and AGFI ≥0.90, RMSEA <0.08 and SRMR ≤0.10 were taken as criteria. As a result of confirmatory factor analysis, no incompatible values were detected for each item for CFI (0.89), NFI (0.81), IFI (0.89), RFI (0.76) and SRMR (0.06). The values were in appropriate ranges. When the fit indices of the model obtained with CFA were examined, it was seen that the X2/df (2.08) value was less than 3, but the CFI (0.89), RFI (0.76), GFI (0.90), AGFI (0.87) and SRMR (0.06) values were at an acceptable level. As a result of the confirmatory factor analysis, these fit indices showed that the model had a good fit [11-14].
The correct answer given to the awareness and knowledge survey items regarding HPV and HPV vaccine was calculated as “2”, the “I don’t know” answer as “1” and the wrong answer as “0”. It was accepted that the awareness and knowledge level increased as the score obtained from the survey increased.
Statistical Analysis
The obtained data were evaluated in the Statistical Package for Social Sciences (SPSS) 25.0 statistical package program. Descriptive statistics were given as mean, standard deviation, median for numerical variables, and number and percentage for categorical variables. In the evaluation of validity and reliability, Exploratory Factor Analysis was applied and factor loadings, item total correlation values, and Cronbach alpha values were calculated for the items. Confirmatory factor analysis was performed using the R studio package program. The conformity of the data to normal distribution was assessed using the Kolmogorov-Smirnov test. Differences between two groups in terms of continuous variables that were not normally distributed were analyzed using the Mann Whitney U test, and differences between multiple groups were analyzed using the Kruskal Wallis test. The results were evaluated at a 95% confidence interval and p<0.05 values were considered significant.
Results
The mean age of the participants was 29.04 ± 6.62 years. 156 (61.2%) of the participants were in the 21-30 age group and 174 (68.2%) were university graduates. 148 (58.0%) of the participants were single, 158 (62.0%) were employed, 73 (28.6) were healthcare workers, and 181 (71.0%) lived in the city center or a metropolitan city. 225 (88.2%) of the participants had no chronic disease and (98.8%) stated that they were heterosexual (Table 1). Of the men, 152 (59.6%) reported that they had not received any information about HPV, 250 (98.0%) had not received the HPV vaccine, 102 (40.0%) did not consider receiving the HPV vaccine, and 144 (56.5%) thought that it was difficult to obtain the HPV vaccine.
Table 1: Distribution of participants according to sociodemographic characteristics and some variables related to HPV.
|
n |
% |
|
| n |
255 |
100 |
| Age group (year) | ||
| 18-20 |
11 |
4.3 |
| 21-25 |
82 |
32.2 |
| 25-30 |
74 |
29 |
| 31-35 |
51 |
20 |
| 36-40 |
16 |
6.3 |
| 41-45 |
21 |
8.2 |
| Marital status | ||
| Single |
148 |
58 |
| Married |
102 |
40 |
| Widow |
5 |
2 |
| Eğitim düzeyi | ||
| Primary – secondary school |
13 |
5.1 |
| High school |
23 |
9 |
| College |
174 |
68.2 |
| Masters |
45 |
17.7 |
| Occupation | ||
| Working |
158 |
62 |
| Not working |
21 |
8.2 |
| Student |
76 |
29.8 |
| Health worker |
73 |
28.6 |
| Place where lived during most of life | ||
| City center |
181 |
71 |
| District |
58 |
22.7 |
| Village |
16 |
6.3 |
| Income level | ||
| Income is less than expenses |
84 |
32.9 |
| Income is equal to expenses |
102 |
40 |
| Income is more than expenses |
69 |
27.1 |
| Has children |
78 |
30.6 |
| Smoking |
96 |
37.6 |
| Comorbidity |
30 |
11.8 |
| Sexual orientation | ||
| Heterosexual |
252 |
98.8 |
| Homosexual |
3 |
1.2 |
| Given information about HPV vaccine |
103 |
40.4 |
| HPV vaccination status | ||
| Not vaccined |
250 |
98 |
|
Gardasil 4/2 dose |
3 |
1.2 |
| Gardasil 9/2 dose |
2 |
0.8 |
| Considering to be vaccined for HPV | ||
| Yes |
55 |
21.6 |
| No |
102 |
40 |
| Undecided |
98 |
38.4 |
| Considers hard to reach HPV vaccine |
111 |
43.5 |
184 (72.2%) of the men in the study group thought that HPV was a very common disease in humans. The item with the highest number of correct answers among men (82.7%) was “Having more than one sexual partner increases the risk of HPV transmission.”, while the item with the lowest number of correct answers (8.6%) was “How many types of HPV vaccines are there?” (Table 2).
Table 2: Distribution of responses to the participants’ awareness and knowledge survey regarding HPV and HPV vaccine.
|
n |
% |
|
| 1. HPV is a virus that is quite common in humans. | ||
| Yes (C) |
184 |
72.2 |
| No |
71 |
27.8 |
| 2. How many types of HPV are there? | ||
| 2 |
2 |
0.7 |
| 4 |
10 |
3.9 |
| 9 |
17 |
6.7 |
| More than 200 (C) |
93 |
36.5 |
| I don’t know |
133 |
52.2 |
| 3. HPV can often be found in a person without any symptoms or signs. | ||
| Yes (C) |
153 |
60 |
| No |
19 |
7.5 |
| I don’t know |
83 |
32.5 |
| 4. HPV does not cause disease anywhere on the body except the genital areas. | ||
| Yes |
21 |
8.2 |
| No (C) |
145 |
56.9 |
| I don’t know |
89 |
34.9 |
| 5. HPV only causes disease in women. | ||
| Yes |
5 |
2 |
| No (C) |
178 |
69.8 |
| I don’t know |
72 |
28.2 |
| 6. HPV can cause mouth, pharynx, anus and penis cancer and genital warts in men. | ||
| Yes (C) |
172 |
67.5 |
| No |
5 |
2 |
| I don’t know |
78 |
30.5 |
| 7. HPV is transmitted only through genital contact. | ||
| Yes |
59 |
23.1 |
| No (C) |
119 |
46.7 |
| I don’t know |
77 |
30.2 |
| 8. Using a condom reduces the risk of HPV infection. | ||
| Yes (C) |
193 |
75.7 |
| No |
13 |
5.1 |
| I don’t know |
49 |
19.2 |
| 9. Having more than one sexual partner increases the risk of contracting HPV. | ||
| Yes (C) |
211 |
82.7 |
| No |
3 |
1.2 |
| I don’t know |
41 |
16.1 |
| 10. Are there any medications that can be used against HPV? | ||
| Yes (C) |
125 |
49 |
| No |
36 |
14.1 |
| I don’t know |
94 |
36.9 |
| 11. How many types of HPV vaccines are there? | ||
| 1 |
8 |
3.1 |
| 2 |
48 |
18.8 |
| 3 (C) |
22 |
8.6 |
| 4 |
18 |
7.1 |
| I don’t know |
159 |
62.4 |
| 12. What is the best age for the first HPV vaccine? | ||
| 9 (C) |
83 |
32.5 |
| 11 |
22 |
8.7 |
| 13 |
28 |
11 |
| 18 |
114 |
44.7 |
| 45 |
8 |
3.1 |
| 13. How many doses of HPV vaccine given after the age of 18 provide immunity? | ||
| 1 |
9 |
3.5 |
| 2 |
35 |
13.8 |
| 3 (C) |
51 |
20 |
| I don’t know |
160 |
62.7 |
| 14. HPV vaccine has side effects that can cause health problems. | ||
| Yes |
48 |
18.8 |
| No (C) |
61 |
23.9 |
| I don’t know |
146 |
57.3 |
| 15. HPV vaccine is only administered to women | ||
| Yes |
10 |
3.9 |
| No (C) |
159 |
62.4 |
| I don’t know |
86 |
33.7 |
| 16. Do you think that HPV vaccination should be given to men? | ||
| Yes (C) |
201 |
78.8 |
| No |
54 |
21.2 |
| 17. HPV vaccine can be administered to men between the ages of 18-45 | ||
| Yes (C) |
146 |
57.2 |
| No |
15 |
5.9 |
| I don’t know |
94 |
36.9 |
| 18. HPV vaccination in men can contribute to the elimination of HPV (having no patients in the community). | ||
| Yes (C) |
146 |
57.3 |
| No |
12 |
4.7 |
| I don’t know |
97 |
38 |
(C): Correct answer.
In the factor analysis for the awareness and knowledge survey about HPV and HPV vaccine, Kaiser-Meyer-Olkin: 0.875, Barlett’s test result was p<0.001. Two items in the survey (Item 13: 0.021 and Item 14: 0.038) were removed from the survey because their factor loadings were below 0.30. The factor loadings ranged between 0.302 and 0.812, and it was determined that the items collected in a single sub-domain explained 31.63% of the total variance. Cronbach’s alpha value was determined as 0.814. The item-total correlation values for the items in the survey ranged between 0.201 and 0.714 . In addition, according to the confirmatory factor analysis results of the awareness and knowledge scale regarding HPV and HPV vaccine, the x2/dF value was determined as 2.08, AGFI as 0.87, RMSEA as 0.07, SRMR as 0.06, and GFI as 0.90. The path diagram showing the model structure and standard regression coefficients is shown in Figure 1. The median (min-max) score of the men in the study group from the survey was 24.0 (6.0-32.0) and the mean (SD) was found to be 23.20. In the study group, those in the 26-30 age group were found to have higher knowledge and awareness scores than those in the 31-35 age group (p=0.032). Singles had higher scores than married individuals (p=0.014). In terms of educational status, those with primary school education had lower scores than those with university and master’s degrees, those with high school education had lower scores than those with university and master’s degrees, and those with university level education had lower scores than those with master’s degrees (p<0.001). Those who were health workers had higher scores than those who were not (p<0.001). Those whose income was equal to expenses had lower scores than those whose income was greater than expenses (p=0.012). Those who did not have children were found to have higher scores than those who did (p=0.002). Those who had information about HPV vaccination had higher scores than those who had not (p<0.001). Those who considered getting HPV vaccination were found to have higher levels of awareness and knowledge about HPV and HPV vaccination than those who did not consider it and were undecided (p<0.001). Those who thought it was difficult to access HPV vaccination were found to have higher scores than those who did not consider it (p<0.001) (Figure 1 and Tables 3-5).
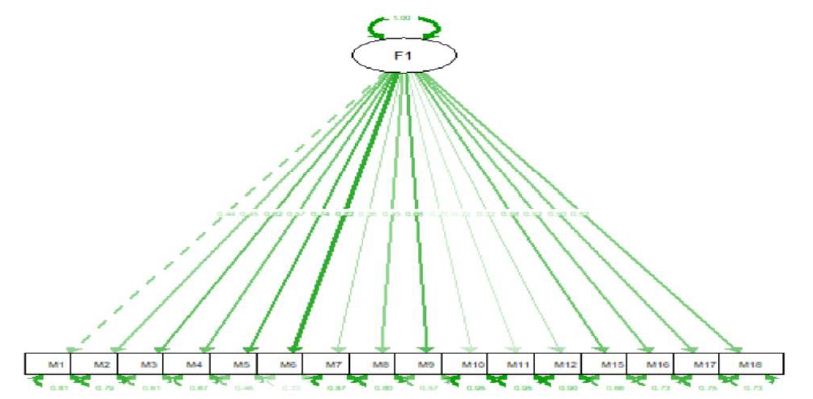
Figure 1: Path diagram showing the model structure and standard regression coefficients.
Table 3: Factor loadings for the questionnaire, correlation between items and Cronbach alpha values when items are removed.
|
Items |
Factor loading | Correlation between items | Cronbach alpha value when item is removed |
| Item 1 | 0.493 | 0.409 |
0.814 |
|
Item 2 |
0.504 | 0.420 | 0.811 |
| Item 3 | 0.657 | 0.561 |
0.803 |
|
Item 4 |
0.615 | 0.523 | 0.805 |
|
Item 5 |
0.749 | 0.645 |
0.801 |
| Item 6 | 0.812 | 0.714 |
0.797 |
|
Item 7 |
0.416 | 0.351 | 0.817 |
| Item 8 | 0.483 | 0.361 |
0.815 |
|
Item 9 |
0.684 | 0.575 | 0.807 |
| Item 10 | 0.302 | 0.201 |
0.827 |
|
Item 11 |
0.305 | 0.203 | 0.823 |
| Item 12 | 0.373 | 0.316 |
0.823 |
|
Item 15 |
0.641 | 0.542 | 0.805 |
| Item 16 | 0.594 | 0.500 |
0.806 |
|
Item 17 |
0.550 | 0.432 | 0.811 |
| Item 18 | 0.473 | 0.476 |
0.808 |
Scale Cronbach alpha value: 0.821.
Table 4: Katılımcıların sosyodemografik özelliklerine göre anketten aldıkları puanın karşılaştırılması.
|
Median (min-max) |
p |
|
| Age group (year) |
0.032* |
|
| 18-20 |
26.0 (18.0-30.0) |
|
| 21-25 |
25.0 (6.0-32.0) |
|
| 26-30 |
26.0 (13.0-32.0) |
|
| 31-35 |
21.0 (13.0-32.0) |
|
| 36-40 |
23.5 (13.0-32.0) |
|
| 41-45 |
20.0 (13.0-32.0) |
|
| Marital status |
0.014* |
|
| Single |
25.0 (6.0-32.0) |
|
| Married |
22.0 (13.0-32.0) |
|
| Widow |
20.0 (15.0-28.0) |
|
| Eğitim düzeyi |
<0.001* |
|
| Primary – secondary school |
16.0 (13.0-22.0) |
|
| High school |
18.0 (13.0-32.0) |
|
| College |
24.0 (6.0-32.0) |
|
| Masters |
28.0 (13.0-32.0) |
|
| Occupation |
0.075* |
|
| Working |
23.0 (13.0-32.0) |
|
| Not working |
22.0 (13.0-30.0) |
|
| Student |
25.0 (6.0-31.0) |
|
| Health worker |
<0.001** |
|
| No |
22.0 (6.0-32.0) |
|
| Yes |
27.0 (13.0-32.0) |
|
| Place where lived during most of life |
0.407* |
|
| City center |
24.0 (6.0-32.0) |
|
| District |
23.0 (12.0-31.0) |
|
| Village |
22.5 (13.0-30.0) |
|
| Income level |
0.012* |
|
| Income is less than expenses |
23.0 (6.0-32.0) |
|
| Income is equal to expenses |
23.0 (12.0-32.0) |
|
| Income is more than expenses |
26.0 (13.0-32.0) |
|
| Has children |
0.002** |
|
| No |
25.0 (6.0-32.0) |
|
| Yes |
20.5 (13.0-32.0) |
|
| Smoking |
0.149** |
|
| No |
24.0 (6.0-32.0) |
|
| Yes |
23.0 (13.0-32.0) |
|
| Comorbidity |
0.837** |
|
| No |
24.0 (6.0-32.0) |
|
| Present |
22.5 (13.0-32.0) |
|
| Sexual orientation |
0.699** |
|
| Heterosexual |
24.0 (6.0-32.0) |
|
| Homosexual |
19,0 (18,0-29,0) |
*Kruskal-Wallis test, **Mann-Whitney U test
Table 5: Comparison of the participants’ scores on the survey according to factors that may be related to them.
|
Median (min-max) |
p |
|
| Given information about HPV vaccine |
<0.001* |
|
| Yes |
28.0 (6.0-32.0) |
|
| No |
21.0 (12.0-32.0) |
|
| HPV vaccination status |
0.320* |
|
| Yes |
26.0 (6.0-32.0) |
|
| No |
24.0 (12.0-32.0) |
|
| HPV vaccination status according to vaccine type |
0.336** |
|
| Not vaccined |
24.0 (12.0-32.0) |
|
| Gardasil 4/2 doz |
25.0 (6.0-32.0) |
|
| Gardasil 9/2 doz |
29.0 (26.0-32.0) |
|
| Considering to be vaccined for HPV |
<0.001** |
|
| Yes |
28.0 (15.0-32.0) |
|
| No |
23.0 (6.0-32.0) |
|
| Undecided |
23.0 (12.0-32.0) |
|
| Considers hard to reach HPV vaccine |
<0.001* |
|
| Yes |
27.0 (13.0-32.0) |
|
| No |
22.0 (6.0-32.0) |
Discussion
Among sexually transmitted diseases, HPV infection is considered the most common worldwide. Persistent HPV infection is associated with more than 5% of all cancers worldwide. One of the main problems with HPV as an oncovirus is the significant difference between the time of diagnosis and the early stages of chronic infection. Early detection of HPV infection and HPV-induced lesions is critical for cancer prevention [1,3,15]. Genital HPV infection is very common among males, with an estimated prevalence of 65.2% in asymptomatic males aged 18–70 [16]. In our survey, most participants correctly answered a similar question: “HPV is a highly prevalent virus in humans.” Regarding risks to daughters, single fathers were significantly more likely to believe that their daughters were at risk for both HPV and cervical cancer. Concerns specific to single fathers included explaining the sexual nature of HPV and taking their daughters to the gynecologist for vaccination. In this respect, the results obtained for single men in our study are similar [17].
In the awareness and knowledge scale regarding HPV and HPV vaccine in this study, it was determined that those with primary school education had lower scores than those with university and master’s degrees, those with high school education had lower scores than those with university and master’s degrees, and those with university education had lower scores than those with master’s degrees. It is known that risky sexual behaviors are directly related to low education levels. Insufficient education levels negatively affect the tendency to this problem. This situation makes it difficult to prevent and treat these diseases. Similar to our findings, a cross-sectional study of 22,974 men in Denmark found that higher education was strongly associated with having heard of HPV. One study reported that men with less than a high school education were approximately 40% more likely to develop HPV infection. A cohort study of men in the United States found that having a college degree or other higher education was significantly associated with a lower risk of new infection with any type of HPV. The effectiveness of medical education has been demonstrated in an experimental study that demonstrated a statistically significant difference between pretest and posttest scores after the implementation of the education. These results support our findings. This suggests that level of education is a factor associated with HPV infection and that educated individuals have easier access to information sources and can use information more effectively. Our study found that those who were healthcare workers had higher scores than those who were not. Aslan and Bakan found that in a descriptive study conducted among health education students, including men, students who had knowledge about sexually transmitted infections had significantly higher levels of HPV knowledge. Lack of knowledge is a significant barrier to the prevention, diagnosis, and treatment of HPV infections and related diseases. The reason for the high level of knowledge among those who were knowledgeable about HPV and HPV vaccines may be attributed to the education men received as students or employees in the health field. In our study, 98% of the participants reported that they had not received HPV vaccination. In a similar study, Loke et al. reported that the HPV vaccination rate among men in the United States and Canada was very low, with rates ranging from 1.1% to 31.7% . This systematic review and meta-analysis showed that compliance with HPV vaccination was low (11% in total) among young men of working age (18-30 years). In addition, in our study, those whose income was equal to their expenses had lower scores than those whose income was greater than their expenses (0: 0.012). When the HPV and HPV vaccine awareness and knowledge level score is low, the rate of HPV vaccination is also low. From this, it is inferred that the lower the socioeconomic level, the lower the rate of HPV vaccination. The results in another study were similar. In this study, the fact that the vaccine is not covered by many health insurance companies makes it difficult for men to access the vaccine [18-24].
In this study, those who considered getting HPV vaccine were found to have higher levels of awareness and knowledge about HPV and HPV vaccine compared to those who were not considering or were undecided (p<0.001). One study found that they were more willing to get vaccinated and had higher awareness about HPV infection and malignancy [25]. Another study found that students who were more willing to get vaccinated had higher HPV knowledge scores [26]. Our findings are supported by similar studies. This situation can be explained by the fact that knowledge about the risk of exposure to HPV, especially in men, increases vaccine acceptance. In fact, when the HPV and HPV vaccine awareness and knowledge score is low, the rate of HPV vaccine application may be low. When the HPV and HPV vaccine awareness and knowledge score is high, the rate of HPV vaccine application is also high [27]. Our results were comparable to a previous study that showed that knowledge and awareness about HPV and HPV vaccine predicted it. The median score (min-max) of the men in this study group from the survey was 24.0 (6.0-32.0) and the mean (SD) was determined as 23.20. In the study group, those in the 26-30 age group were found to have higher knowledge and awareness scores than those in the 31-35 age group. In addition, men who obtained information about the HPV vaccine had higher scores than those who did not. The reason for the high mean score may be that the study was conducted in a university hospital polyclinic and most of the participants who applied were students or workers in the health field. Contrary to our findings, a study reported that 930 Singaporean men had insufficient knowledge and awareness about HPV [28]. In a descriptive study conducted by Aslan and Bakan [22] on health education students, it was found that male students had lower mean scores on the HPV knowledge level. These different results may be due to the recent increase in information about HPV and the HPV vaccine. In this study, more than half of the participants stated that HPV does not only cause diseases in women (69.8%) and that it can also cause mouth, pharynx, anus and penis cancer and genital warts in men (67.5). In a study conducted in Syria, 8.7% stated that HPV can be transmitted to both women and men [29]. According to these studies, it is thought that introducing Human papillomavirus as a cause of cervical cancer in particular may lead to the wrong perception that it is a disease specific to women only. The reason for the different results in our study is thought to be that the majority of the participants in the study are healthcare workers working at a university hospital and that there have been intensive information activities on HPV recently. It is known that HPV is a virus with more than 200 types that can be transmitted directly to the genital area, mouth and throat through sexual contact. In this study, less than half of the participants (47%) answered the question ‘HPV is transmitted only through contact with the genital area.’ correctly. According to literature data, participants stated that HPV can be transmitted sexually with a percentage ranging from 7.4% to 74.1% [30]. As can be seen, the awareness rate regarding the sexual transmission of HPV is generally low, although it varies between countries. Conservative family structures, education levels, and socioeconomic conditions can restrict society’s attitudes toward sexuality and the freedom to conduct research and discuss sexuality. In our study, more than half of the participants had a bachelor’s degree or higher, and the study was conducted in a large city, suggesting that the participants may be more aware of sexuality.
As of 2018, more than 80 countries and regions have implemented HPV vaccination programs. Although international organizations have made significant efforts to expand HPV vaccination programs, HPV vaccination rates remain below 50% in many countries worldwide. In our study, almost all participants (98%) did not receive HPV vaccination. In terms of considering HPV vaccination, the majority (78.4%) said ‘no’ or ‘undecided’. In terms of accessing HPV vaccination, more than half of the participants (56.5%) thought it was difficult. A study from sixteen European countries reported that the rate of participants considering HPV vaccination ranged from 45.6% to 79.5%. Among the Scandinavian countries, Sweden and Iceland have the highest acceptance rates of HPV vaccination. In studies, 7.7% to 37% of participants believed that the HPV vaccine could lead to early sexual orientation, while 7.9% to 68.1% stated that they avoided vaccinating themselves or their children due to safety concerns [6-8,31]. One study revealed that 62.3% of participants had heard of the HPV vaccine and 50.7% agreed to have themselves or their children vaccinated [32]. One study determined that 39.6% of participants did not get vaccinated because they did not have sufficient information and 30.8% did not get vaccinated because they thought it was unnecessary . Concerns about the potential side effects of the vaccine are an effective factor in not reaching the desired level of vaccination rates [6-9]. Research findings also reveal the need for HPV education interventions aimed at men. The level of knowledge about the HPV vaccine can affect an individual’s intention to get vaccinated. In male-specific HPV training, when the incidence of oropharyngeal and penile cancer was emphasized, it was found that men wanted to be vaccinated [33]. In a study conducted in Turkey, it was revealed that 1.1% of the participants had received the HPV vaccine. The reason for this was 94.4% of the participants stated that they were not informed, 18.7% thought it was harmful, and 4% avoided the vaccine because they were afraid of possible side effects [34]. In our study, only five (2%) of the male participants had received the HPV vaccine. In studies conducted in Turkey, the rates of receiving the HPV vaccine ranged from 1.0% to 4.3% [35]. Lack of information about HPV and the HPV vaccine prevents the desired level of interest in the vaccine both in our country and worldwide. In our country, the HPV vaccine has not yet been included in the vaccination calendar of the Ministry of Health. Although the level of knowledge about the HPV vaccine varies by country, it is generally low. Governments should make the Human Papillomavirus vaccine freely available, make it an important part of their national agenda and actively fight against it. There is generally less awareness among men that the HPV vaccine can also protect against various HPV-related cancers in men. HPV-related cancers can be largely prevented through vaccination. Vaccination protects men from developing anogenital condylomas, other malignancies related to the infection, including the penis, anus and base of the tongue. If both sexes are vaccinated, the spread of the virus decreases. Thus, it can be more effective in successfully achieving herd immunity against the virus [5-9]. In our study, most participants answered a similar question correctly. ‘HPV vaccination in men can contribute to the elimination of HPV (no cases in the community)’. HPV vaccination also helps to control the spread of HPV and reduce the overall burden of the virus on health systems. In addition, HPV-related cancer treatments are often costly and require significant resources from health systems, so vaccination against HPV may also provide cost savings in the long term. Primary and school-based HPV vaccination programs at this stage allow for higher vaccination rates and contribute to sociodemographic equality. A good solution to increase vaccination worldwide is to provide catch-up vaccination, preferably in school health systems [7-10]. The biggest problem is the lack of knowledge about preventing HPV-related pathologies. More education on this issue will increase compliance with vaccination campaigns. People who are not recommended for vaccination by their primary care physicians are less likely to receive HPV vaccination than young people who are. Vaccination of men, as well as women, is being integrated into national school-based and primary care vaccination programs worldwide, but vaccination coverage is still patchy, information is insufficient, and misconceptions persist [8-13]. Our study had some limitations. Since the data were collected cross-sectionally at a single university clinic over a specific time period, the results may not be generalizable to the entire population.
When we look at the content of our study, it is seen that healthcare workers, participants with higher income than expenses and undergraduate/graduate degrees scored higher in terms of knowledge and awareness levels about HPV and HPV vaccine. Considering the general structure of the society, male compliance with HPV vaccine is not considered sufficient. This study investigates a population of men aged 18-45, where there is evidence that compliance with vaccines is extremely poor. In order to achieve a higher level of compliance, it is important to give importance to vaccination campaigns and dissemination of information about the benefits of the vaccine as well as the risks of HPV infection.
To date, vaccination is the only way to break the chain of infection, but HPV vaccination programs, especially gender-neutral programs, are still inadequate. This makes it difficult to achieve herd immunity, especially in men who are invited to get vaccinated years after their first vaccination. There is increasing evidence that gender-neutral vaccination alone can significantly control HPV-related diseases in both women and men and can maximize the prevention of cervical cancer, especially if vaccine coverage is not high among girls in a given region. Given the current situation, it is reasonable to assume that secondary prevention will continue to be the basis for cervical cancer prevention. Another global public health goal should also be to provide scientific evidence to determine the most appropriate timing of vaccination to maximize cancer recurrence and improve outcomes of recommended treatments. Finally, health communication should also play an important role. Indeed, standardizing both the quality and quantity of information can lead to increased adherence to various vaccine awareness campaigns, which must already overcome the biases and psychological factors that complicate promotion and prevention interventions. Of course, investing in promotion campaigns, as in the case of polio, will both improve the cost-benefit balance (making this balance even more favorable than that achieved by primary prevention alone) and equalize vaccination coverage between the two sexes.
References
- Zayats R, Murooka TT, McKinnon LR (2022) HPV and the Risk of HIV Acquisition in Women. Front Cell Infect Microbiol 12: 814948. [crossref]
- Muñoz-Bello JO, Carrillo-García A, Lizano M (2022) Epidemiology and Molecular Biology of HPV Variants in Cervical Cancer: The State of the Art in Mexico. Int J Mol Sci 23(15). [crossref]
- Lin G, Li J (2023) Circulating HPV DNA in HPV-associated cancers. Clin Chim Acta 542: 117269. [crossref]
- Võrno T, Lutsar K, Uusküla A, Padrik L, Raud T, et al. (2017) Cost-effectiveness of HPV vaccination in the context of high cervical cancer incidence and low screening coverage. Vaccine 35(46). [crossref]
- de Oliveira CM, Fregnani JHTG, Villa LL (2019) HPV Vaccine: Updates and Highlights. Acta Cytol 63(2). [crossref]
- Conageski C (2023) Human Papillomavirus Vaccines. Clin Obstet Gynecol 66(3). [crossref]
- Marshall S, Fleming A, Sahm LJ, Moore AC (2023) Identifying intervention strategies to improve HPV vaccine decision-making using behaviour change theory. Vaccine 41(7). [crossref]
- Garolla A, Graziani A, Grande G, Ortolani C, Ferlin A (2024) HPV-related diseases in male patients: an underestimated conundrum. J Endocrinol Invest 47(2). [crossref]
- Williamson AL (2023) Recent Developments in Human Papillomavirus (HPV) Vaccinology. Viruses 15(7)[crossref]
- Gamboa-Hoil SI (2023) Human papillomavirus in men. Rev Int Androl 21(1). [crossref]
- Erkorkmaz U, Ozdamar K, Sanisoglu Y (2013) Confirmatory Factor Analysis and Fit Indices: Review. Article in Turkiye Klinikleri Journal of Medical Sciences. Turkiye Klinikleri J Med Sci 33(1)
- Abdi H, Williams LJ (2010) Principal component analysis. Wiley Interdiscip Rev Comput Stat 2: 433–59.
- Kılıç S (2016) Cronbachs alpha reliability coefficient. Psychiatry and Behavioral Sciences 6(1)
- Cakmur H (2012) Measurement-Reliability-Validity in Research. TAF Preventive Medicine Bulletin 11(3)
- Yarbrough ML, Burnham CAD (2016) The ABCs of STIs: An Update on Sexually Transmitted Infections. Clin Chem 62(6). [crossref]
- Spencer JC, Brewer NT, Trogdon JG, Weinberger M, Coyne-Beasley T, Wheeler SB (2020) Cost- effectiveness of Interventions to Increase HPV Vaccine Uptake. Pediatrics 146(6). [crossref]
- Lelliott M, Sahker E, Poudyal H (2023) A Review of Parental Vaccine Hesitancy for Human Papillomavirus in Japan. J Clin Med 12(5). [crossref]
- Nielsen A, Munk C, Liaw KL, Kjær SK .(2009) Awareness of human papillomavirus in 23 000 Danish men from the general male population. European Journal of Cancer Prevention 18(3). [crossref]
- Han JJ, Beltran TH, Song JW, Klaric J, Choi YS (2017) Prevalence of Genital Human Papillomavirus Infection and Human Papillomavirus Vaccination Rates Among US Adult Men: National Health and Nutrition Examination Survey (NHANES) 2013-2014. JAMA Oncol 3(6). [crossref]
- Lu B, Wu Y, Nielson CM, Flores R, Abrahamsen M, et al. (2009) Factors Associated with Acquisition and Clearance of Human Papillomavirus Infection in a Cohort of US Men: A Prospective Study. J Infect Dis 199(3). [crossref]
- Ford ME, Cannady K, Nahhas GJ, Knight KD, Chavis C, et al. (2020) Assessing an intervention to increase knowledge related to cervical cancer and the HPV vaccine. Adv Cancer Res 146: 115–37. [crossref]
- Aslan G, Bakan AB (2021) Identification of the Knowledge Level of Students Receiving Health Education About the Human Papilloma Virus, Screening Tests, and Human Papilloma Virus Vaccination. J Community Health 46(2). [crossref]
- Loke AY, Kwan ML, Wong YT, Wong AKY (2017) The uptake of human papillomavirus vaccination and its associated factors among adolescents: A systematic review. J Prim Care Community Health 8(4). [crossref]
- Chow EPF, Tabrizi SN, Fairley CK, Wigan R, Machalek DA, et al. (2021) Prevalence of human papillomavirus in young men who have sex with men after the implementation of gender-neutral HPV vaccination: a repeated cross-sectional study. Lancet Infect Dis 21(10). [crossref]
- Baloch Z, Yasmeen N, Li Y, Zhang W, Lu H, et al. (2017) Knowledge and awareness of cervical cancer, human papillomavirus (HPV), and HPV vaccine among HPV-infected chinese women. Medical Science Monitor 23: 4269–77. [crossref]
- Varer Akpinar C, Alanya Tosun S (2023) Knowledge and perceptions regarding Human Papillomavirus (HPV) and willingness to receive HPV vaccination among university students in a north-eastern city in Turkey. BMC Womens Health 23(1). [crossref]
- Dönmez S, Öztürk R, Kısa S, Karaoz Weller B, Zeyneloğlu S (2019) Knowledge and perception of female nursing students about human papillomavirus (HPV), cervical cancer, and attitudes toward HPV vaccination. J Am Coll Health 67(5). [crossref]
- Pitts M, Smith A, Croy S, Lyons A, Ryall R, et al. (2009) Singaporean men’s knowledge of cervical cancer and human papillomavirus (HPV) and their attitudes towards HPV vaccination. Vaccine 27(22). [crossref]
- Alsaad MA, Shamsuddin K, Fadzil F (2012) Knowledge towards HPV infection and HPV vaccines among Syrian mothers. Asian Pac J Cancer Prev 13(3). [crossref]
- Koç Z (2015) University students’ knowledge and attitudes regarding cervical cancer, human papillomavirus, and human papillomavirus vaccines in Turkey. J Am Coll Health 63(1). [crossref]
- López N, Garcés-Sánchez M, Panizo MB, De La Cueva IS, Artés MT, et al. (2020) HPV knowledge and vaccine acceptance among European adolescents and their parents: a systematic literature review. Public Health Rev 41. [crossref]
- Ortiz RR, Smith A, Coyne-Beasley T (2019) A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum Vaccin Immunother; 15(7-8). [crossref]
- Bonafide KE, Vanable PA (2015) Male human papillomavirus vaccine acceptance is enhanced by a brief intervention that emphasizes both male-specific vaccine benefits and altruistic motives. Sex Transm Dis 42(2). [crossref]
- Keten HS, Ucer H, Dalgaci AF, Isik O, Ercan Ö, Guvenc N (2021) Knowledge, Attitude, and Behavior of Teachers Regarding HPV (Human Papillomavirus) and Vaccination. J Cancer Educ 36(3). [crossref]
- Karasu AFG, Adanir I, Aydin S, Ilhan GK, Ofli T (2019) Nurses’ Knowledge and Opinions on HPV Vaccination: a Cross-Sectional Study from Istanbul. J Cancer Educ 34(1). [crossref]