Introduction
Coronavirus disease 2019 (COVID-19) is considered a viral syndrome comprising of pneumonia, cough and dyspnea progressing towards acute respiratory distress syndrome. Recently, a hypercoagulable state has been identified in moderate to severely ill patients, most commonly quantified by increased D-dimer levels. Additionally, prolonged prothrombin time and increased fibrinogen levels are associated with a poor prognosis [1]. This has led to concerns of COVID-19 patients being predisposed to clotting complications and discussions of early anticoagulation for pre- emptive management. We present the case of one such patient with complications of COVID-19 coagulopathy.
Case Report
A 43-year-old male presented to the emergency department for ongoing shortness of breath, having completed outpatient azithromycin. Past medical history was significant for hypertension, obesity, daily alcohol usage, and negative for recent travel or sick contacts. The chest x-ray revealed right lower lobe pneumonia and antibiotics were started. The oxygen saturation improved from 80% on 5 L nasal cannula to 95% after a non-rebreather was placed. A COVID-19 polymerase chain reaction (PCR) test was performed, which resulted negative. The patient was admitted to a progressive care unit, but transferred to the intensive care unit the same day for decreased oxygen saturation to 88%. Due to increased oxygen demands and new fever of 101.5°F, a repeat COVID-19 PCR test was performed. Ascorbic acid, chlordiazepoxide, hydroxychloroquine, prophylactic pantoprazole, and prophylactic enoxaparin were ordered. The repeat COVID-19 PCR resulted positive. On day 8, testing revealed a D-Dimer of 3055 ng/mL, fibrinogen >700 mg/dL and platelets of 546,000/mm3. Due to concern for increased risk of thrombosis, the patient was started on therapeutic enoxaparin. The D-dimer continued to trend up (day 11: 3,299 ng/mL; day 12: >3,680 ng/mL), while the fibrinogen and platelets decreased (day 11: 576 mg/ dL and 341,000; day 12: 561 mg/dL and 348,000). Additionally, the patient was intubated on day 6, and extubated on day 12.A transthoracic echocardiography was performed and reported to be normal.
On day 13 right hemiplegia, moderate aphasia, and moderate sensation loss to right upper and lower extremity were noted. Computed tomography imaging found an acute cortical left cerebral and right occipital infarct (Figure 1). A National Institutes of Health Stroke Scale was calculated at 20. Neurology was consulted and enoxaparin was held due to risk of hemorrhagic conversion. Due to the infectious risk of COVID-19, further diagnostic testing was limited. As the time of onset was unknown, thrombolytics and mechanical thrombectomy were not considered. Aspirin, atorvastatin, and prophylactic enoxaparin were ordered. On day 15 an ultrasound of the right upper extremity was performed due to unilateral edema which was positive for a right cephalic vein thrombus. Therapeutic enoxaparin was restarted and continued upon discharge to rehabilitation. Prior to discharge, the patient was regaining function in his right extremities.
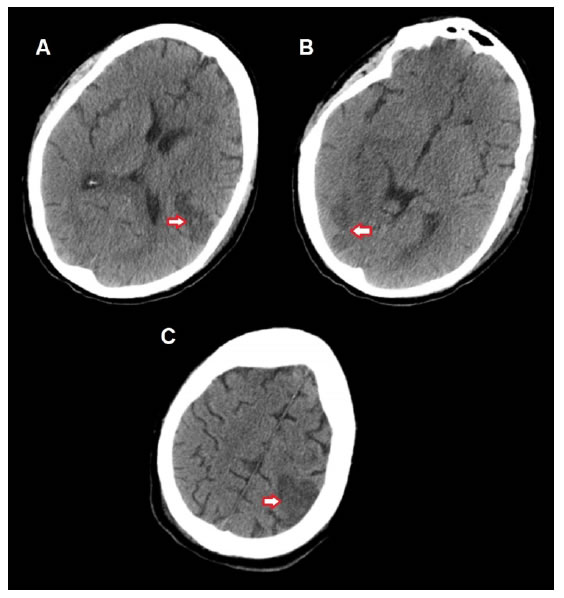
Figure 1. Computed tomography imaging of the brain (non-contrast). A: Left frontoparietal infarct, B: Right occipital infarct, C: Left frontoparietal infarct.
Discussion and Conclusion
We describe the case of a patient with minimal risk factors for stroke and a Well’s criteria of zero. This patient originally presented with severe pulmonary complications of COVID-19 with no evidence of neurologic deficits. Proper prophylaxis and treatment with enoxaparin were utilized. No pharmacologic therapies provided to the patient increased risk of thrombosis. Nonetheless, the patient still developed an acute left cerebral infarct, a right occipital infarct and a right upper extremity thrombosis, clinically consistent with both arterial and venous thrombotic complications.
Limited literature exists which describes stroke as a presenting factor for patients who later tested positive for COVID-19 [2,3]. Our patient on the other hand originally presented with no neurologic symptoms. The late development of significant stroke in our case stresses the importance of a continued thorough neurological examination for severely ill COVID-19 patients throughout their hospital stay. In addition, there appears to be a correlation between stroke and d-dimer, with 7/8 patients having an elevated level. There have been discussions of early anticoagulation strategies for these new thrombotic complications. No anticoagulation was noted prior to stroke for the previously published cases; our patient was started on therapeutic anticoagulation during their hospital stay [2,3]. Tang et al. found that utilization of prophylactic anticoagulation reduced mortality by 19.6% (32.8% vs. 52.4%, p = 0.017) in patients with D-dimer levels greater than six times the upper limit of normal [4]. However, anticoagulation did not prevent thrombosis in our patient, who also had a severely elevated D-dimer. This may point to an alternative form of hypercoagulability due to platelet-rich clots, as was found in an autopsy series from New Orleans [5]. Enoxaparin inhibits factor Xa, which preferentially targets fibrin formation. Potential inclusion of early antiplatelet medications, like aspirin, should be considered.
References
- Han H, Yang L, Liu R, Liu F, Wu KL, et al. (2000) Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. ClinChem Lab Med doi: 10.1515/ cclm-2020-0188. [Crossref]
- Oxley TJ, Mocco J, Majidi S, Christopher PK, Shoirah H, et al. (2020) Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med 382. [Crossref]
- Avula A, Nalleballe K, Narula N, Sapozhnikov S, Dandu V, et al. (2000) COVID-19 presenting as stroke. Brain BehavImmun doi: 10.1016/j.bbi.2020.04.077. [Crossref]
- Tang N, Bai H, Chen X, Gong J, Li D, et al. (2000) Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. Journal of Thrombosis and Haemostasis 18:1094-1099. [Crossref]
- Fox SE, Akmatbekov A, Harbert JL, Guang Li, Quincy BJ, et al. Pulmonary and cardiac pathology in COVID-19: The first autopsy series from New Orleans. medRxiv doi: https://doi.org/10.1101/2020.04.06.20050575.