Abstract
This is a prospective and comparative study over four months between the cold season (January-February) and the hot season (April-May) 2016. It involved 258 patients hospitalized in the department of cardiac medicine during this period in which the diagnosis of cardiovascular pathologies was made. Through this work, we studied the epidemiological, clinical, paraclinical, therapeutic and evolutionary aspects and finally the impact of climatic and seasonal variations on cardiovascular pathologies. Epidemiologically, cardiovascular disease accounts for 55.60% of admission to the service. There is a male predominance of 53.10% compared to 46.90% for females. The average age was 55.17 years. The age range greater than 60 years is the most affected with 54.25%. The admission rate for cardiovascular disease was 43.41% during the cold season compared with 56.59% during the heat season. Clinically, the most common diagnoses were heart failure, stroke and hypertension with 47.28%, respectively; 24.03%; and 8.91%. Therapeutically, the protocol used largely relies on diuretics, ACE inhibitors, antiplatelet agents. On an evolutionary level, 81.79% of the patients had a favorable outcome. The mortality rate is 14.34% with a peak of death during the warm season. Thus, 24 deaths were found, representing a mortality rate of 16.43% and 64.86% of total deaths in the warm season. Indeed, the elevations of temperature lead to an increase in the admissions but also of the mortality related to the cardiovascular diseases.
Keywords
Cardiovascular pathologies, Seasonal climatic variations, Prevalence, Morbimortality, National Hospital of Lamorde Niamey
Introduction
Cardiovascular disease (CVD) is a group of disorders affecting the heart and blood vessels. Nowadays, they pose an important public health problem because they constitute the first cause of death in the world [1]. CVD occurs in Africa in younger people compared to other regions of the world. Their increase is due to an increasing burden of their risk factors (RF) in the adult population [2]. CVD can largely be prevented by effective and efficient interventions directed against the major modifiable RIS [3]. However, apart from classic RFs, other factors influence cardiovascular pathologies, in particular climatic variations such as cold and heat. However, very few studies have been carried out in Niger to assess the impact of climate on cardiovascular pathologies. The aim of our work is to study the impact of seasonal climatic variations on cardiovascular pathologies at HNABD.
Patients and Methods
This was a prospective descriptive, analytical and comparative study over two climatic periods (cold season and hot season) in 2016. It took place over four months in the HNABD medicine-cardiology department. The study population consists of all patients hospitalized in the department during the period. All patients diagnosed with cardiovascular disease who agreed to participate in the study were included. The parameters studied were:
- Epidemiological (frequency; age-sex; level of study; country of origin; provenance; standard of living)
- Clinics (history, RDF, comorbidity, diagnosis)
- Paraclinical (biology, chest x-ray, electrocardiogram (ECG), echocardiography, and brain scan).
- Progressive (length of hospitalization, favorable=improvement of the clinical and/or paraclinical condition with discharge, death)
- Climatic parameters (table 1) such as temperature, humidity, wind regime, were provided by the national meteorological service in Niamey in 2016. Temperature (in degrees Celsius, °C), humidity relative (in percentage,%) and wind speed in m/s. The season was defined from January to February for the cold and from April to May for the heat.
Table 1: Meteorological climatic parameters of the national meteorological service in Niamey in 2016
|
Climatic parameters |
January | Febuary | April |
May |
| Average temperature |
26 ° |
29° | 37° |
38° |
| Average maximal temperature |
32° |
36° | 43° |
43° |
| Minimal temperature |
20° |
22° | 31° |
32° |
| Highest recorded temperature |
39° |
45° | 47° |
47° |
| Lowest recorded temperature |
30° |
37° | 35° |
36° |
| Wind Speed |
29km/h |
26km/h | 22km/h |
22km/h |
| Wind temperature |
20° |
22° | 31° |
32° |
| Average rainfall per day |
0mm |
0mm | 1mm |
1mm |
| One-day rainfall record |
0mm |
0mm | 5mm |
10mm |
| Humidity |
36% |
23% | 22% |
18% |
Km/h: kilometer per hour, mm: millimeter
We proceeded by registering all of the patients hospitalized in the department as they progressed during the study period; The use of patient records as they are admitted. Data collection was manual, through an individual survey form. Data analysis and processing are carried out using the following software: Word 2010, EXCEL 2010, CSPro6.2, IBM SPSS 20. Consent of patients with participated in the study was obtained in advance as well as the approval of the ethics committee of the hospital.
Results
Epidemiological Aspects
A total of 464 patients were admitted during these periods of the study to the department, including 258 cases of cardiovascular disease, or 55.61% of all admissions. The admission rate for cardiovascular pathologies in the department was significantly higher during the hot season compared to the cold season, i.e. 146 patients (56.59%) vs. 112 patients (43.41%) (p=0.0027). Male sex was predominant at 53.10%, with a Sex ratio=1.13. The mean age of the patients was 55.17 years with extremes ranging from 10 to 99 years. The most affected age group is over 60 with 54.25%.
Clinical Aspects
The most common reasons for hospitalization were heart failure (HF) followed by stroke (32.17% and 24.03% respectively). The most common pathological antecedents were HF 37.60%; followed by high blood pressure (HBP) 34.49%; then stroke 9.30%. The most common risk factors were sedentary lifestyle in 62.79%, followed by hypertension in 37.60%. The comorbidities encountered were chronic obstructive pulmonary disease (COPD), human immunodeficiency virus (HIV) infection, tuberculosis, chronic renal failure (IRC), acute renal failure (ARI), hepatitis and cancer with respectively rates of 5.03; 4.26%; 3.12%; 2.71%; 2.32%; 1.94%; 1.16%. The most common functional signs were dyspnea and edema of the lower limbs, with 43.80% and 37.20% respectively. The most common physical signs were hypertension, 40.31% followed by tachycardia 33.72%, then fever 30.23%.
Paraclinical Aspects
Anemia was present in 34.11% of cases; inflammatory syndrome in 17.83% of cases; hyperlipidemia in 16.28% of cases; 15.11% fasting hyperglycemia and finally 8.91% cases of hyper creatinine. Chest x-ray revealed cardiomegaly and signs of acute pulmonary edema (APE) in 23.64% and 19.77%, respectively. ECG revealed 13.17% cases of atrial fibrillation (AF); 5.03% cases of atrioventricular block (AVB); 4.26% cases of myocardial infarction (MI); and 3.49% cases for the other signs. Cardiac ultrasound was performed in 95 patients (36.82%) including 52 cases (54.73%) normal, 14 cases (14.74%) of dilation of the cavities; 9 cases (9.49%) of pericardial effusion; 7 cases (7.36%) of valve disease, 13 cases (13.68%) for other signs. Brain CT was performed in 62 patients (24.03%) and revealed 46 cases (74.20%) ischemic stroke (DALY) and 16 cases (25.80%) hemorrhagic stroke (AVCH). We see that there are about 3 times more DALYs than AVCH. P=0.0012.
Strokes in general are much more frequent during the hot season with 38 cases against 24 cases during the cold season.
Diagnosis Aspect
The most frequent pathologies were HF, stroke, and hypertension, with a frequency of 47.28%, 24.03%, and 8.91%, respectively. However, 53 cases of HTA were associated with hypertension in 43.44% of cases and 28 cases of stroke had hypertension in 45.16% of cases. Of the 258 diagnoses relating to cardiovascular pathologies, 56.59% occur during the hot season vs. 43.41% during the cold season (p=). There is a predominance of cardiovascular pathologies during the hot season (Figure 1).
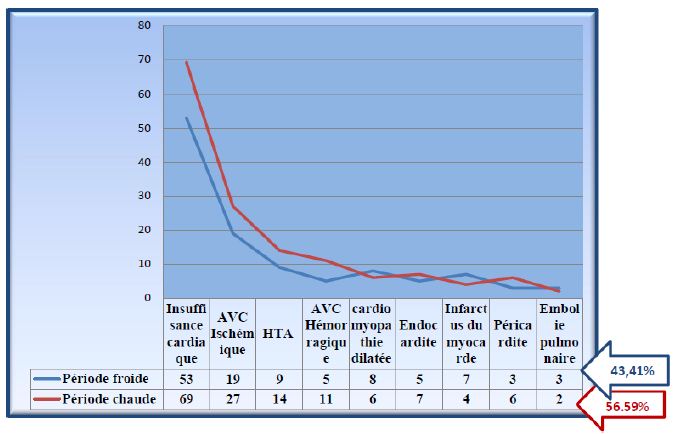
Figure 1: Cardiovascular pathologies according to the period. Km/h: kilometer per hour, mm: millimeter
(Thus, out of the 122 cases of HF, 69 cases were admitted during the hot season vs. 53 cases in the cold season (p=0.04), 23 cases of hypertension, including 14 cases during the hot season vs. 9 cases during the cold season (p=0.14), of the 62 cases of stroke, 38 cases during the hot season against 24 cases in the cold season (p=0.012), of the 14 cases of dilated cardiomyopathy (DCM), 6 were admitted during the heat season against 8 cases in the cold season (p=0.11), 12 cases of endocarditis, of which 7 were admitted during the hot season against 5 cases in the cold season (p=0.41), 11 cases of myocardial infarction including 4 cases during the hot season against 7 cases in the cold season (p=0.20), 9 cases of pericardial effusion including 6 cases during the hot season against 3 cases in the cold season (p=0, 15), 5 cases of pulmonary embolism, including 2 cases during the hot season against 3 cases in the cold season (p=0.52).)
Therapeutical Aspects
Diuretics were administered in 70.93% of patients, antiplatelet agents in 69.37; CE inhibitors in 61.24%, beta blockers in 20.93%; calcium channel blockers in 20.15%; Anticoagulant in 8.60%; central antihypertensive drugs, in 6.58% of patients.
Evolutionary Aspects
An improvement was noted in 211 patients (81.79%) including 96 cases (45.50%) during the cold season vs. 115 cases (54.50%) in the heat season (0.064); 10 patients (3.87%) are transferred to other departments. 83 cases of death overall including 37 cases due to cardiovascular pathologies (44.58%) compared to 46 (55.42%) cases related to other pathologies (p=0.16). Thus among the 37 patients (14.34%) who died from cardiovascular causes, 64.87% had occurred in the heat season vs. 35.13% in the cold season (0.010). Regarding cardiovascular pathologies, a higher admission rate was recorded during the hot season with 146 patients or 56.59% of the sample against 112 patients (43.41%) during the cold season. Likewise, a higher mortality rate was recorded during this period with 24 deaths, i.e. 16.43% against 11.60% during the cold period (p=0.010).
Cardiovascular Pathologies and Climatic Variations
To better analyze the correlation between cardiovascular pathologies and seasonal climatic variations, we crossed the admission and death rate of patients with variation curves of climatic parameters (temperature, humidity, wind speed). Thus, Table 2 and Figures 2-7 summarize the variation in the number of admissions according to meteorological parameters.
Table 2: The number of admissions depending on the season
|
Clinical Parameters |
Cold season
Number of deaths / admitted =13/112 patients (11,60%) |
Hot season Number of deaths / admitted =24/146 patients (16,43%) |
| Average Temperature |
27,5° vs 33,8° |
37,5° vs 33,8° P=0,010 |
| Highest average temperature |
34° vs 38.6° |
43.5° vs 38.6° P=0.0027 |
| Lowest average temperature |
21.4° vs 27.3° |
30.8°vs27.3° |
| Wind speed |
7,5m/s vs 6.38m/s |
6m/s vs 6.38m/s |
| Humidity |
29.5 % vs 31.8% |
20% vs 31.8% |
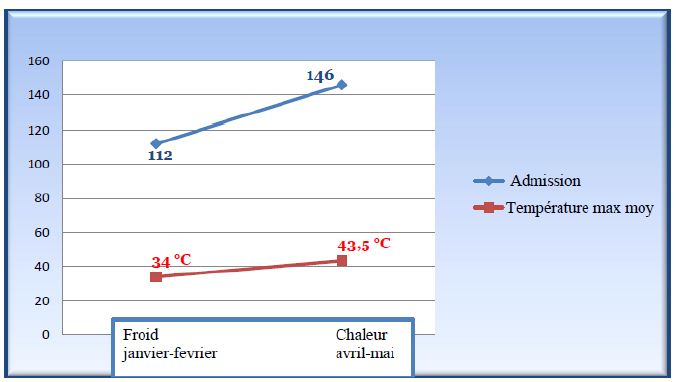
Figure 2: Average maximum temperature and number of inlets
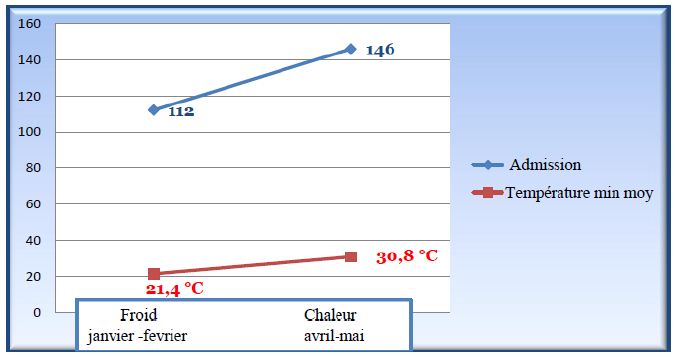
Figure 3: Average minimum temperature and number of inlets

Figure 4: Average humidity and intake number
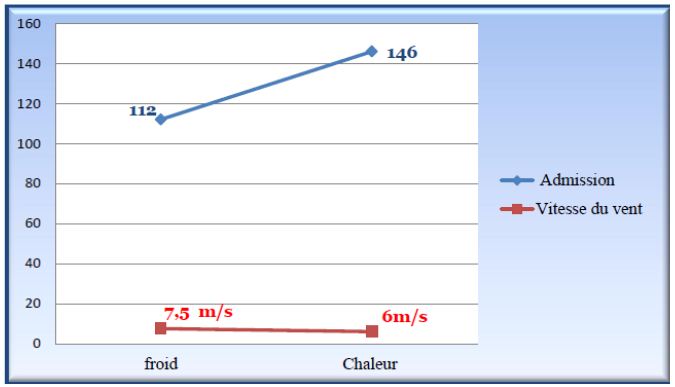
Figure 5: Wind speed and intake number
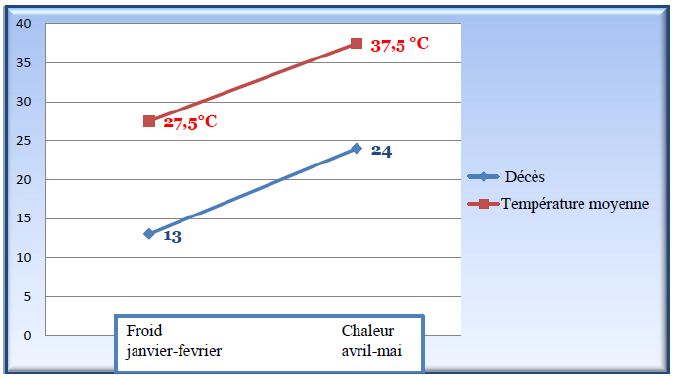
Figure 6: Evolution of the number of deaths and variation of the average temperature
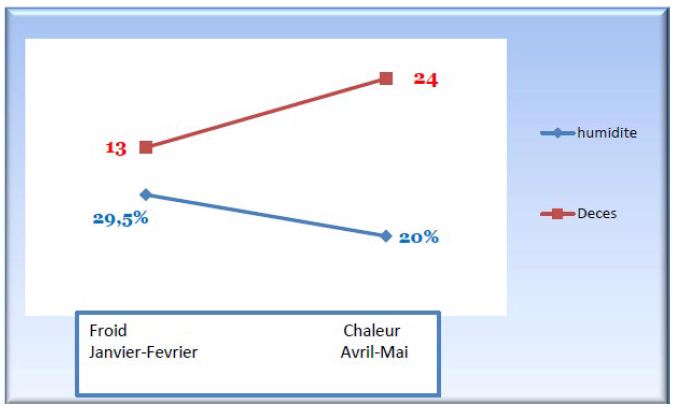
Figure 7: Evolution of the number of deaths and variation in average humidity
The peak intake was recorded during the hot season when the average maximum temperature is 43.5°C. The admission rate during the hot season was significantly higher than that in the cold season (146 vs. 112 cases, p=0.0027) for temperatures:
– respective maximum average of 43,5°C vs. 38,6°C vs. 34°C .
– respective minimum average 30,8°C vs. 27,3°C vs. 21,4°C
A respective average humidity de 20% vs. 31,8% vs. 29,5%
-average wind speed of 6m/s vs. 6,38 m/s vs. 7,5 m/s
The number of deaths was significantly higher in the hot season than in the cold season (16,43% vs. 11,6% cases p=0,010 ) pour des
– respective maximum average temperature of 33,8°C vs. 37,5°C vs. 27,5°C.
-respective minimum average of 30,8°C vs. 27,3°C vs. 21,4°C
– average humidity of 20% vs. 31,8% vs. 29,5%,
– average wind speed of 6 m/s vs. 6,3 m/s vs. 7,5m/s
Comments and Discussions
We registered a total of 464 patients in the department, including 258 patients with cardiovascular disease. The application of chronobiology to the occurrence of cardiovascular pathologies allowed us to observe a fluctuation in the admission rates of these pathologies which were more predominant in the hot season than in the cold season (56.59% vs. 43.41%) with a peak of admission recorded during the hot season. Indeed, CVDs follow a seasonal pattern in many populations. Thus winter peaks and clusters of all broadly defined CVDs subtypes are consistently described after cold snap. Individuals living in colder climates may be more vulnerable to seasonality [4].
In our study these two periods were characterized that year, for the cold season, an average temperature (maximum and minimum), the average relative humidity lower than their annual averages, which proves the relatively cold and dry character of this period. For the hot season, the average temperature (maximum and minimum), average relative humidity were higher than their annual averages, which proves the hot and dry character of the period in Niger. The wind speed is equal to the annual average. Indeed, through the data of several studies, extreme temperatures seem to play a role on cardiovascular risk factors as well as on the risk of occurrence or decompensations of CVD.
Risk Factors for Cardiovascular Pathologies and Seasonal Variations
There are RFs that are the root cause of most CVD. In fact, we found that 85.25% of the patients in our sample had at least one FRD, the most frequent of which was sedentary lifestyle with 62.79%, followed by hypertension 37.60%. Our results are similar to those of Ben Ahmed and col, who have also found sedentary lifestyle as the most frequent RF (76.4%) [5]. However, FINDIBE and AL, found the existence of FDR in 89.3% of patients whose hypertension was the most frequent RF [6]. Just recently a study showed that there is a seasonal variation in risk factors, which found that the RFs studied tend to be higher in winter and lower in summer months. There is considerable evidence that the seasonality of variation in ambient temperature affects blood pressure (BP) levels and the incidence of cardiovascular events. The first evidence showing that ambient temperature is inversely associated with a change in arterial pressure (SBP and DBP) was published by Rose in 1961 [7]. Numerous studies have followed, showing that BP exhibits seasonal variations parallel to seasonal changes in ambient temperature, with lower BP levels at high temperatures and higher BP at lower temperatures [8]. Seasonal variation in BP appears to be a worldwide phenomenon with similar data reported for countries with varying climatic conditions, and affects both sexes, all age groups, normotensive individuals and hypertensive patients, untreated and treated [9]. In most people, the seasonality of the change in BP has no medical relevance. However, in the cases of hypertensive patients treated well controlled in winter, an excessive fall in BP could occur in summer, symptomatic requiring a down titration of drug therapy [10]. In contrast, hypertensive patients treated with controlled BP in summer may show a dramatic increase in BP above the recommended threshold in winter, requiring drug therapy upgrading. Similar fluctuations could occur in people traveling from cold to hot places, or vice versa, in such cases with severe hypotension, or with loss of BP control. In practice, the doctor should check the change in the BP level and should adjust the antihypertensive drug appropriately, aiming to achieve an optimal BP level without symptoms. A recent study showed that 13.5% of the 667 patients who visited a hypertension clinic saw their medication reduced in the summer with the highest drug reduction rate being for diuretics [11]. Due to the lower BP targets currently recommended by hypertension companies and the unusually high temperature recently observed in several studies in the summer, seasonal variation in BP is becoming a common concern in clinical practice. Exposure to cold may increase sympathetic nervous system activation and vasoconstriction, and reduce endothelial function which may contribute to increased BP [1]. Indeed, other factors have also been reported, such as increased plasma levels of fibrinogen, low density protein (LDL) cholesterol, vasoconstriction and blood viscosity, which may increase blood thrombogenicity and the risk of cardiovascular events [10]. Advanced age seems to correspond to an additional RF, although the scientific data in this area are sparse and sparse. For some authors, the impact of extreme winter temperatures appears over a longer term and seems less direct than high summer temperatures [11].
Cardiovascular Pathologies and Seasonal Variations
Extreme weather events can influence cardiovascular health in a number of ways. Too much heat or cold becomes stressful on the human body, especially if it is already stressed by the disease, and can worsen a person’s condition with heart disease. In addition to being a vulnerability factor, CVD can also be exacerbated over a period as short as a heat wave or a very cold period. For example, the loss of water and salt caused by sweat in a context of high heat increases the concentration of other components of the blood (globules, cholesterol, etc.) and thus increases its viscosity, which places l individual at risk of coronary or cerebral thrombosis. It is the same in a context of intense cold, which causes the shutdown of a large part of the blood supply to the skin, which overloads the central organs and increases the viscosity of the blood in the order of 20% [1]. In our study, we found a higher admission rate for cardiovascular pathologies during the hot season (56.59%), however our results are contrary to the literature which reports a higher admission rate in the cold season.
Heart Failure
In our series, HF is the most frequent cardiovascular disease with a frequency of 47.28% (122 cases) and this predominates in the hot season (56.55% vs. 43.45%). Our result is contrary to that of Gallerani et al. in Italia which found that hospitalization for HF is more frequent in winter (28.4%) and lower in summer (20.4%) and that there is a significant peak in January for all the groups [12] but the authors did not find any difference according to sex, age, severity, presence of hypertension, diabetes. In addition, the authors explain that the low admission may be related to the closure of beds in summer and the reduction in the population going on vacation. For hospitalization, there are similar variations with a difference of 30% (+10% in January and -20% in August).
In our study we found a high number of HF associated with hypertension (43.44%). Hirai in a recent work has also made this observation [13] and reports in its multivariate analysis, it is the absence of diuretics in such patients which is correlated with the increase in hospitalization in winter, explain the authors. Kaneko et al. by studying the characteristics of patients with heart failure hospitalized in winter, found that they are older and have a greater prevalence of hypertension and diabetes than patients hospitalized during these other seasons. Preserved ejection fraction (PEF) HFs are more common among patients hospitalized in winter [14].
Temperature variations throughout the day also seem to play a role as reported by Qiu et al. by studying daily weather results and hospitalizations for HF from 2000 to 2007 in Hong Kong. The authors find a peak in hospitalization for HF in winter, but above all they find that a large change in temperature during the day is associated with an increase in hospitalizations. They found that any temperature variation of 1°C increases the risk of hospitalization by 0.86%, especially during the cold season. The phenomenon is more marked among women and the elderly. Thus the others conclude that the large temperature changes in winter during the day are associated with an increase in hospitalizations for HF [15]. In Hong Kong, Winter is mild with average temperatures of 19.5°C. Residents may be more sensitive to temperature changes during the day. There is no heating in most homes. In contrast, during the hot season, people live with air conditioning and do less activity outdoors. They thus reduce the risk of significant temperature variation. This could explain the lack of impact of the temperature change in summer on the other hand in our countries the air conditioning is not accessible to all and that these periods are contemporaneous with power cuts, which means that patients have a longer exposure to heat. In addition, many of these patients continue to take diuretics at the same dose and rarely do blood tests. Exposure to heat and sweating can worsen the side effects of diuretics with ionic imbalances.
However recent studies show that the reality is more complex. Thus Zaoq et al. published in 2013 a study made in China. These authors find two peaks of hospitalization for HF: December (+40%) and August (+23%). In the multivariate study, the blood serum rate (95% CI: 2.132-2.144; p <0.036) is an independent risk factor for hospitalizations in August [16]. Recent publications show a seasonal variation with a peak also in summer Gostman et al. Yamamuto in Japan. Patients hospitalized in summer have a lower ejection fraction (EF), a greater need for dobutamine and die more [17,18].
MI
We recorded 11 cases of MI whose difference was not statistically significant between the two seasons, 4 cases during the hot season versus 7 cases in the cold (p=0.20). In fact, from 1985, Muller et al. showed a circadian variation in the frequency of MI with a peak at 6 a.m. until noon [19]. Twenty years later, Morabito et al. showed a relationship between weather and heart attack [20]. In fact, these authors show that the frequency of MI increases with the drop in temperature. A drop of 10°C during the day is associated with a 19% increase in heart attacks in patients over 65 years of age. Conversely, a high temperature for more than 9 hours also significantly increases the admission for infarction. The authors focus mainly on the notion of dyscomfort or severe discomfort caused by hot or cold climatic conditions rather than temperature. Recent studies find an increase in heart attacks in winter. Finally, in February 2015, Caussin et al. analyzed the association between a brief exposure (between 1 and 7 days) to environmental parameters and the appearance of a heart attack [21]. These authors found a 5% increase in risk of having a heart attack by 10°C drop in maximum temperature and 8.9% during a period of influenza epidemic after adjustment with weekends and days off. Thus the association between low temperatures and myocardial infarction (MI) is stronger during an influenza epidemic. Only the temperature drop is associated with the MI.
On the other hand, the authors do not find any effect of heat despite the fact that the period studied includes the years of heat wave (2003 and 2006). In the United States, an analysis of 259,891 cases of MI from the Second National Myocardial Infarction Registry demonstrated that there were 53% more cases of myocardial infarction (MI) in winter compared to the summer [22]. Udell, in a meta-analysis, shows that influenza vaccination is associated with a reduced risk of coronary heart disease, particularly for patients at risk [23]. The explanation put forward is the severe acute inflammation during influenza, responsible for plaque rupture and hypercoagulability. For the drop in temperature, it is evoked the sympathetic stimulation and the coagulation system. In fact, the cutaneous receptors of the skin stimulate the sympathetic system. Low temperature increases BP due to vasoconstriction. An increase in the sympathetic system will cause tachycardia, an increase in cardiac work, oxygen consumption and reduced coronary flow as well as a prothrombotic effect related to an increase in hematocrit, blood viscosity, blood pressure, fibrinogen, CRP (C-reactive protein) [23].
Stroke
In our series, 62 stroke cases were recorded including 38 cases during the hot season against 24 cases in the cold (p=0.012). Over the past decades, several studies from different countries have examined the seasonal variation of cerebrovascular disease and have led to results [24]. While some authors strongly doubt the existence of a true seasonal relationship, a series of studies suggest fluctuation with a peak during the cold season [24-26]. Recently published data also indicate a possible relationship with a typical winter peak for several factors of etiological relevance for the occurrence of stroke [27]. However, other studies report a peak summer stroke incidence, while others even suggest an inverse seasonal relationship between different types of stroke [28]. Indeed, a seasonal variation of stroke now seems to be widely accepted according to a study carried out in Athens, which included 1299 patients having suffered a stroke for the first time. The monthly distribution of all 1,299 stroke cases showed a decline in stroke admissions, starting in May and reaching its nadir in August, while an increase is seen in November. The stroke in this case remains at almost stable high levels during the cold season of the year (November to April). The authors would expect stroke cases to be evenly distributed over all 12 months of the year. However, the observed number of cases differs considerably from the expected number, indicating the existence of an annual variation in hospital admissions. August and September were the months with the least entries, while January and March were the most affected months. Dividing the year into 4 seasons as described above, we observed a significant drop in stroke incidence during the summer when most stroke cases were recorded, as expected during the cold season. They also examined the distribution of the different stroke subtypes over the 4 seasons of the year. The same seasonal pattern with the peak of incidence in the cold season and its nadir in summer has been identified for both CE and ICH [29].
Therapeutic and Evolving Aspects
Out of a total of 55.60% of patients with cardiovascular pathology, 70.93% had benefited from a diuretic, 69.37% antiplatelet agent, 61.24% CEI, 20.93% beta-blocker, 20.15% calcium channel blocker, 18.60% anticoagulant, and 6.58% central antihypertensive agent.
Evolutionarily, we saw 81.79% improvement over the study period. Thus, 63.56% of patients had a hospital stay of less than 10 days. The number of patients who died in the ward during the study was 83 cases, or 17.88% of all 464 patients hospitalized in the ward. Indeed, the mortality rate for cardiovascular pathologies is 14.34% (37 cases out of 258) and 44.58% of the total deaths.
The death rate from cardiovascular pathologies was higher in the hot season than in the cold season. It was 15.38% of total deaths and 64.86% of deaths due to cardiovascular pathologies.
Our results differ from data in the literature where we see a peak in death during the cold and a peak during the heat. The lack of mortality peak during the cold in Niger can be explained by the rarity of extreme lower temperatures.
Epidemiological studies have consistently shown an increased risk of cardiovascular disease in cold weather. For example, in England and Wales, the peak of winter and summer had 20,000 additional deaths per year [2].
In a time series analysis of 1,826,186 non-accidental deaths in 272 major cities in China, relative to temperature with the minimum mortality (22.8°C), 14.33% of non-accidental mortality was attributed to high temperatures. suboptimal, with moderate cold temperatures (−1.4°C to 22.8°C) for an attributable fraction of 10.49%, while moderate heat temperatures (22.8 to 29.0°C) accounted for an attributable fraction of only 2.08% [2]. In an analysis of 74,225,200 deaths at 384 locations in Australia, Brazil, Canada, China, Italy, Japan, South Korea, Spain, Sweden, Taiwan, Thailand, United Kingdom and United States, deaths attributable to non-hot temperatures. Optimal temperatures, defined as temperatures above or below the minimum mortality point, and extreme temperatures, defined using cutoffs at the 2.5th and 97.5th percentiles, were calculated. The results showed that the risk of death from cold temperatures (7.29%, 7.02-7.49) was higher than those from warm temperatures (0.42%, 0.39-0.44). Interestingly, extreme cold and high temperatures accounted for only 0.86% (0.84-0.87) of the total mortality [30]. Hemodynamic changes associated with cold temperature and increased thrombogenicity may explain both increased cardiovascular risk and seasonal mortality [31]. Exposure to cold induces endothelial dysfunction and increased BP, which may be the main contributors to the increased risk of mortality [6].
Recently, Marti-Soler et al. studied the monthly mortality of 19 countries out of approximately 54 million deaths [32]. The authors calculated the number of expected deaths without seasonal variation. All-cause mortality (cardiovascular and non-cardiovascular/non-cancer) shows a seasonal variation. In both hemispheres, the number of deaths is higher than expected in winter. In countries close to the equator, seasonal variations in all-cause mortality are smaller. For CV mortality, the difference between peak and nadir ranges from 0.185 to 0.466 in the northern hemisphere, from 0.087 to 0.108 near the equator, and from 0.219 to 0.409 in the southern hemisphere. Seasonal variation was not found for cancer mortality in most countries. Indeed, exposure to cold is recognized as one of the factors controlling the incidence and lethality of ischemic heart disease, sudden non-traumatic death. The highest rates of cardiovascular disease are found in the colder winter months as a Dutch study pointed out that mortality increases almost linearly as temperature decreases and is higher with strong winds (Kunst 2001) [33]. Cardiovascular and respiratory pathologies were the main causes of mortality identified in this study. Another study was conducted in the Netherlands between 1979 and 1997 by differentiating the causes of death (neoplasms, diseases and two age groups (0-64 years and over 65 years). During cold spells, excess mortality varies from 10,1 to 26.8%. It is defined as a period of at least 9 consecutive days during which the minimum temperature is below -5°C, or at least 6 consecutive days with a minimum temperature below -10°C. The effects can be more harmful the longer the period is (Huynen et al. 2001) [34]. A French study (Dijon) on daily mortality from 1968 to 1997 compared with the perceived temperature shows that cold spells are indeed associated with excess mortality over a period of about two weeks after the coldest day, with a delay of one to two days. However, the authors point out that because people are more exposed to indoor than outdoor temperatures, the excess mortality may be linked to infectious diseases rather than exposure to cold [35]. According to a Parisian study, scorching temperatures directly contribute to mortality from cardiovascular or respiratory diseases, in particular among the elderly. During the heatwave of summer 2003 in Europe, more than 70,000 additional deaths were recorded [36]. Very low winter temperatures and heat waves are associated with increased mortality, especially in the elderly population. In the elderly, the perception of cold and the performance of the vascular response are different compared to adults. The decompensation of chronic pathologies, more common in the elderly, makes them even more vulnerable to seasonal changes and extreme temperatures. A French study shows that rising temperatures are associated with a greater frequency of cardiovascular decompensations in people over 70 years old [37]. Also in the register of large studies, we must cite the study of Xu carried out in China on 626,950 patients using data from 32 hospitals in Beijing [38]. This study shows that hospitalized heart patients are older during the winter months, with a risk of mortality increasing by 30 to 50% (p <0.01) compared to those hospitalized in other months. This seasonal variation is not found in younger patients. The increase in winter deaths in elderly patients is associated with ischemic disease (RR: 1.22), pulmonary heart (RR: 1.42), arrhythmias (RR: 1.67), heart failure (RR: 1.30), stroke (RR: 1.3) and other brain diseases. Seasonal variability is found, whether the patient has lung disease or not.
In May 2015 in the EHJ, Yang studied seasonal variations in blood pressure and cardiovascular mortality in patients with a history of CV disease. They studied 23,000 people with CV backgrounds and recruited from around ten regions in China from 2004 to 2008. After 7 years of follow-up, 1,484 CV deaths occurred [38]. SBP is significantly higher in winter than in summer (145 vs. 136 mmHg; p <0.001). Below 5°C, each 10°C drop in outdoor temperature is associated with a rise of 6.2 mmHg. Furthermore, SBP predicts CV mortality: every 10 mmHg increase in SBP is associated with a 21% increased risk of CV mortality. The authors find an increase in mortality in winter (+41%) in these patients.
According to a study by SEDJAL [39] heart disease and stroke are two of the three main causes of death in Algeria. According to WHO statistics for 2008, cardiovascular disease was responsible for 29% of all deaths, or 69,648 deaths. In Algeria, cardiovascular disease is the leading cause of death, and is responsible for one in four deaths, according to WHO.
In industrialized countries, CVDs are responsible for 44% of deaths each year and 33% in France [40]. Higher rates are recorded during winter and this explains the increased mortality observed during this season. Approximately half of excess winter mortality is attributable to coronary thrombosis. The interval between a cold snap and the impact on cardiovascular mortality is 7 to 14 days. The heatwave of the summer of 2003 which affected a large part of Europe and the Maghreb countries is considered among the hottest of the last fifty years in France, while a 15-day heat wave killed 15,000 people, mostly elderly people with cardiorespiratory diseases. The analysis of the curves relating to the evolution of cardiac emergencies recorded and studied according to the meteorological parameters in the Wilaya of Oran during the year 2010, shows the existence of a relationship between the temperature drops and the significant peaks. heart problems. This analysis shows that cardiovascular disease is distinctly linked to temperature variations. The same observations have been observed in other studies carried out in Europe showing a correlation between CVD and the influence of temperature and more specifically during falls of the latter [39].
Conclusion
This prospective and comparative study on cardiovascular pathologies and seasonal climatic variations at the Amirou Boubacar Diallo National Hospital shows through the various results collected several observations on the subject and to draw conclusions such as the decompensation of cardiovascular pathologies in general is much more common in the hot season than in the cold season. That the mortality rate of these cardiovascular pathologies is higher during the hot season than during the cold season. Indeed, we see that the climate could play an important role in the morbidity and mortality of cardiovascular pathologies with seasonal variations.
Several studies in Africa and Europe have found the same findings. Likewise, within the service, other retrospective studies have found these findings. Further, more in-depth studies are needed on a larger scale to further confirm these findings.
References
- Sungha P, Kazuomi K, Yook-CC, Yuda T, Chen-H C, et al. (2019) The influence of the ambient temperature on blood pressure and how it will affect the epidemiology of hypertension in Asia. J Clin Hypertens 22: 438-448. [crossref]
- Chen R, Yin P, Wang L, et al. (2018) Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ 363: 4306. [crossref]
- Gasparrini A, Guo Y, Hashizume M, et al. (2015) Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386: 369-375. [crossref]
- Discussions commentaires
- Simon S, Ashley KK, Adele R and John J. V. McMurray (2017) Seasonal variations in cardiovascular disease, CARDIOLOGY 658: 14. [crossref]
- H Ben Ahmed, M Allouche, B Zoghlami, M Shimi, R Razghallah, F Gloulou et al. (2014) Mort subite d’origine cardiaque au nord de la Tunisie: variation circadienne, hebdomadaire et saisonnière, Presse Med.
- FINDIBE D. et al. (2014) Morbidité et mortalité hospitalière des maladies cardiovasculaires en milieu tropicale: exemple du CHU de Lomé (Togo) The Pan African Medical Journal.
- Kuleshova VP, Pulinets SA, Sazanova EA, et al. (2001) Biotropic effects of geomagnetic storms and their seasonal variations. Biofizika 46: 930-934. [crossref]
- Gifford DK (1996) Monthly incidence of stroke in rural Kansas. Kans Nurse 71: 3-4.
- Biller J, Jones MP, Bruno A, et al. (1988) Seasonal variation of stroke—does it exist? Neuroepidemiology 7: 89-98. [crossref]
- Rosenthal T (2004) Seasonal variations in blood pressure. Am J Geriatr Cardiol 13: 267-272.
- Arakawa K, Ibaraki A, Kawamoto Y, Tominaga M, Tsuchihashi T (2019) Antihypertensive drug reduction for treated hypertensive patients during the summer. Clin Exp Hypertens 41:389-393. [crossref]
- Massimo Gallerani; Benedetta Boari; Fabio Manfredini; Roberto Manfredini (2011) Seasonal Variation in Heart Failure Hospitalization. Clin Cardiol 34: 389-394. [crossref]
- Hirai M, Kato M, Kinugasa Y, Sugihara S, Yanagihara Kyamada K, et al. (2015) Clinical scenario 1 is associated with winter onset of acute heart failure. Circ J 79: 129-135. [crossref]
- Qui H, Tak-Sun I, Ah Tse L, Tian L, Wang X, Wai Wong T (2013) Is greater temperature change within a day associated with increased emer- gency hospital admissions for heart failure. Circ Heart Failure 6:930-935. [crossref]
- Zhao Q, Yu S, Huang H, Cui H, Qin M, Kong B, et al. (2013) The seasonal variation in hospita- lizations due to chronic systolic heart failure correlates with blood sodium levels and cardiac function. Exp Clin Cardiol 18: 77-80. [crossref]
- Gostman I, Zwas D, Admon D, Lotan C, Keren A (2010) Seasonal variation in hospital admission in patients with failure and its effect on prog-nosis. Cardiology 117: 268-274. [crossref]
- Yamamoto Y, Shirakabe A, Hata N, Kobayashi N, Shinada T, Tomita K (2014) Seasonal variation in patients with acute heart failure: prognostic impact of admission in the summer. Heart Vessels 78: 911-921. [crossref]
- Muller JE, Stone PH, Turi ZG, Rutherford JD, Czeisler CA, et al. (1985) Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med 313: 1315-1322. [crossref]
- Morabito M, Modesti PA, Cecchi L, Crisci A, Orlandini S, Maracchi G, et al. (2005) Relationships between weather and myocardial infarction: a biometeorological approach. Int J Cardiol 105:288-293. [crossref]
- Caussin C, Escolano S, Mustafic H, Bataille S, Tafflet M, et al. (2015) Short-term exposure to environmental parameters and onset of ST elevation myocardial infarction. The CARDIOARSIF registry. Int J Cardiol 183: 17-23. [crossref]
- Udell JA, Zawi R, Bhatt DL, Keshtkar6jah- romi M, Phrommintikul A, et al. (2013) Association between influenza vaccination and cardio- vascular outcomes in high-risk patients: a meta-analysis. JAMA 310: 1711-20. [crossref]
- Konstantinos S, Kostas NV, Georgios T, Andreas S, Nikolaos Z, et al. (2003) Journal of Stroke and Cerebrovascular Diseases 12: 93-96.
- Oberg AL, Ferguson JA, McIntyre LM, Horner RD (2000) Incidence of stroke and season of the year: evidence of an association. Am J Epidemiol 152: 558-564. [crossref]
- Kochanowicz J, Kulakowska A, Drozdowski W (1999) Seasonal variations in stroke incidence in North-Eastern Poland. Neurol Neurochir Pol 33: 1005-1013.
- Luong TH, Rand JH, Wu XX, Godbold JH, Gascon-Lema M, et al. (2002) Seasonal distribution of antiphospholipid antibodies. Stroke 32: 1707-1711. [crossref]
- McLaren M, Kirk G, Bolton-Smith C, Belch JJF (2000) Seasonal variation in plasma levels of endothelin-1 and nitric oxide. Int Angiol 19: 351-353.
- Woodhouse PR, Khaw KT, Plummer M, Foley A, Meade TW (1994) Seasonal variations of plasma fibrinogen and factor VII activity in the elderly: winter infections and death from cardiovascular disease. Lancet 343: 435-439. [crossref]
- Wang Q, Li C, Guo Y, Barnett AG, Tong S, et al. (2017) Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci Total Environ 575: 276-286. [crossref]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, et al. (2015) Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386: 369-375. [crossref]
- Bhatnagar A (2017) Environmental Determinants of Cardiovascular Disease. Circ Res 121: 162-180. [crossref]
- Stergiou GS, Myrsilidi A, Kollias A, Destounis A, Roussias L, et al. (2015) Seasonal variation in meteorological parameters and office, ambulatory and home blood pressure: predicting factors and clinical implications. Hypertens Res 38: 869-875. [crossref]
- Kunst AE, Looman CW, Mackenbach JP (1993) Outdoor air temperature and mortality in The Netherlands: a time-series analysis. J. Epidemiol 137: 331-341. [crossref]
- Huynen M, Martens P, Schram D, Weijenberg MP, Kunst AE (2001) The Impact of Heat Waves ans Cold Spells on Mortality Rates in the Dutch Population. Environmental Health Perspectives 109: 463-470. [crossref]
- Groupe de travail météo France –laboratoire climat et santé ; faculté de médecine de Dijon,département santé environnement (DSE) de l’institut de veille sanitaire – cellules interrégionales d’épidémiologie (Cire).
- OMS, Deuxième conférence mondiale, Chaleur extrême ;Climat et santé, étude de cas, Paris, 7-8 juillet 2016 .
- NOURHASHEMI F (2008) Influence du climat sur les décompensations des personnes âgées. Service de Médecine Interne et de Gérontologie Clinique, CHU Toulouse.
- SEDJAL W, Paramètres météorologiques et les urgences cardiaques: Etude de cas à Oran 2010. Mémoire en science de l’environnement et climatologie.
- Bouhouita (2012) Mortalité cardiovasculaire. Journal El Watan 7.
- Mercer JB (2003) Cold-an underrated risk factor health. Environ Res.