Abstract
EECP (Enhanced External Counterpulsation) has been approved by the FDA (Food and Drug Administration) for management of refractory angina (class IIb). EECP uses 3 sets of pneumatic cuffs that sequentially contract during diastole, increasing aortic diastolic pressure, augmenting coronary blood flow and central venous return. EECP has been shown to improve angina symptoms, reduce nitroglycerin use, and improve exercise tolerance in patients with chronic stable angina. EECP has also been shown to be safe and beneficial in patients with symptomatic stable congestive heart failure. It’s been postulated that cardiac benefits of EECP are mediated though VEGF and Nitric oxide mediated vasodilatation and angiogenesis. The Food and Drug Administration (FDA) has approved EECP therapy for heart failure patients.
Keywords
EECP (Enhanced External Counterpulsation), Angina Pectoris, Congestive Heart Failure, PCI (Percutaneous Coronary Intervention), Myocardial Infarction (MI), the International EECP Patient Registry (IEPR)
Introduction
Enhanced External Counterpulsation (EECP) is a noninvasive technology used in the United States to treat chronic severe angina that is refractory to medical management, especially in patients for whom intervention is contraindicated due to other metabolic conditions. (Class IIB) [1]. It was cleared by U.S. FDA in 1995 [2]. It is currently recommended as class IIB by the American Heart Association, as well as Chinese Medical Association, for refractory angina pectoris [3].
The evaluation of hemodynamic effects of counterpulsation was first studied in the mid-1960s. Water filled bags were wrapped around legs of patients with cardiogenic shock. Soroff and colleagues first studied this technique in humans in 1965 [4].
One course of EECP involves 35 sessions designed as 1 hour sessions per day, 5 days per week
Methods & Materials
The technique involves sequential compression of 3 sets of pneumatic cuffs applied to the calves, thighs, and abdomen which are timed with early diastole of the heart based on EKG monitoring [5]. The patient is attached to finger plethysmograph and cardiac monitoring. Inflation of the cuffs is timed with the R wave on EKG which corresponds with the diastole. This is followed by deflation just before systole. The main purpose is to enhance cardiac coronary perfusion during diastole by enhancing cardiac return and also enhancing backflow into coronaries during diastole. The deflation just before systole reduces the afterload by reducing systolic pressure and creating run-off, thus enhancing the cardiac output with reduced cardiac workload [3].
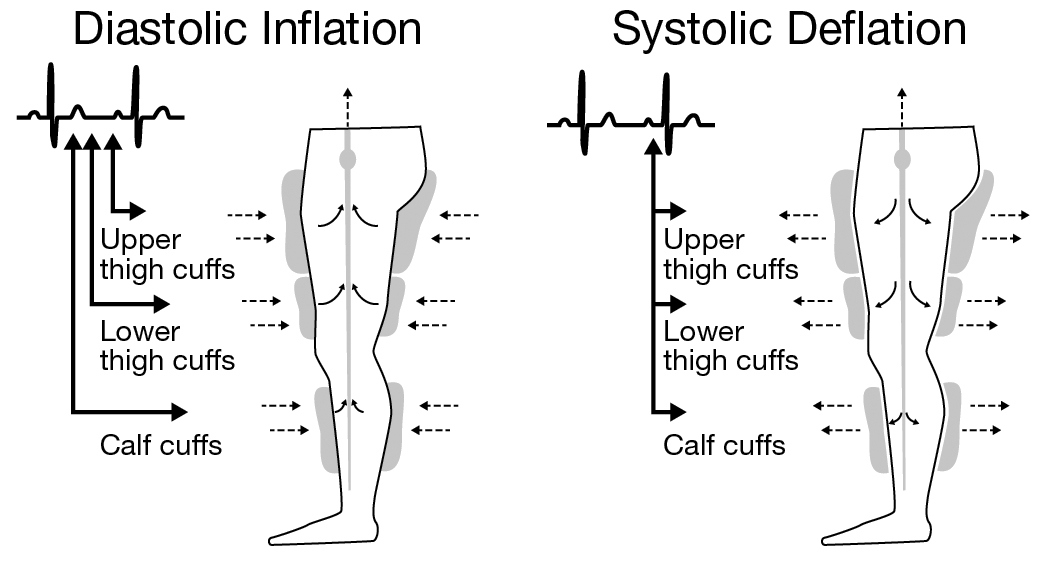
Figure 1. Schematic of the sequential diastolic inflation and systolic deflations of leg cuffs during EECP therapy.
The magnitude of clinical benefit of EECP is measured as a ratio of diastolic to systolic pressure during EECP called Effectiveness Ratio (ER). It has been shown by Suresh, et al that the maximum benefit of EECP is obtained at an ER of 1.5–2. The goal of treatment for coronary disease is diastolic blood pressure /systolic blood pressure =Q>1.2 after counterpulsation [6]. However, Micheals, et al also reported that there is no additional benefit to higher ER with reduction of angina. The clinical relevance of ER is confusing since it has also been shown that there is clinical benefit to patients with EECP in the absence of optimal ER.
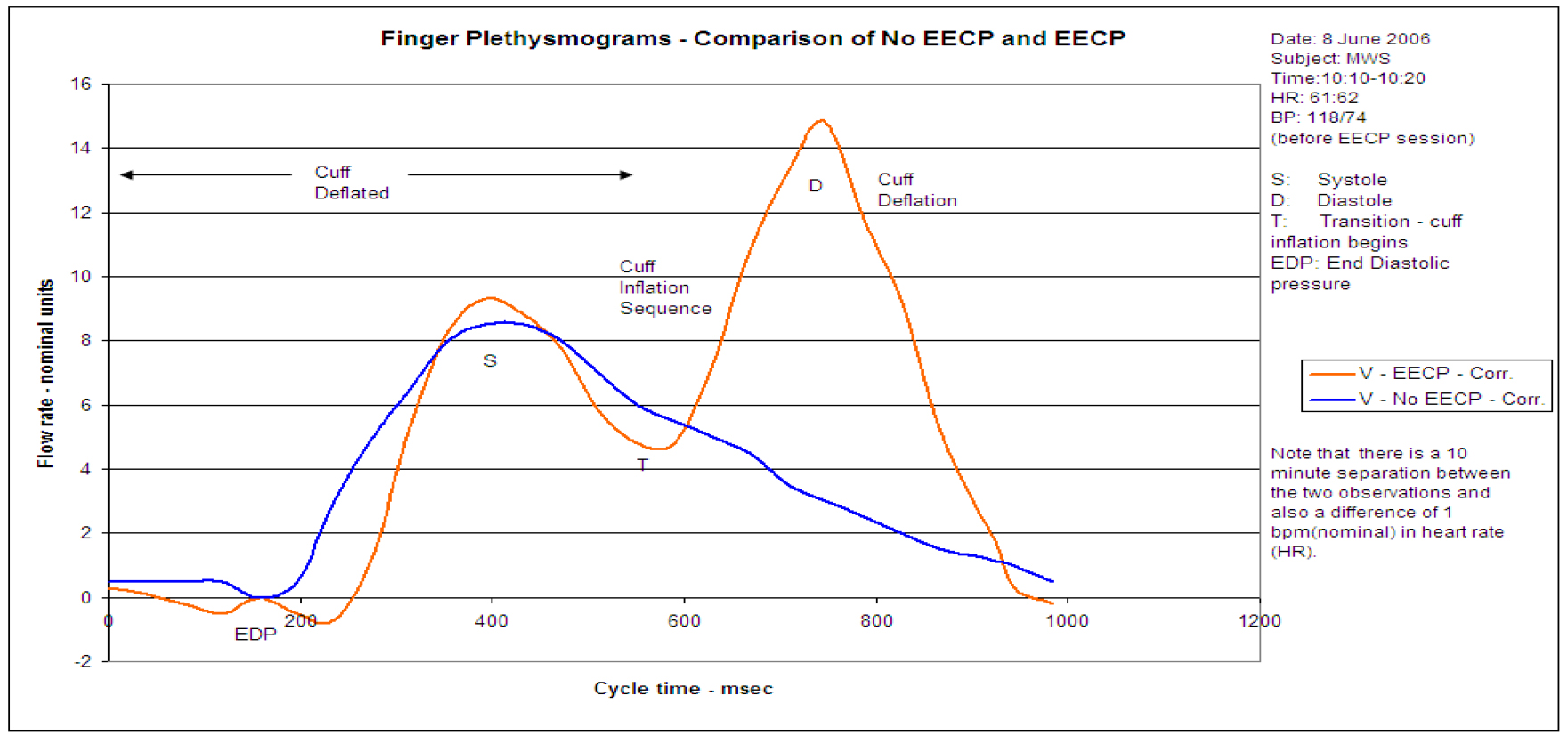
Figure 2. Finger plethysmogram showing the changes in vascular flow rate during EECP therapy; blue curve indicates blood flow without EECP; brown curve shows augmentation of blood flow as EECP cuff is inflated. [S: systole, D: diastole, T: transition (cuff inflation begins), EDP: end-diastolic pressure.]
Patients are screened at the time of referral for potential contraindications which include, but are not limited to, arrhythmias that interfere with machine triggering, bleeding diathesis, active thrombophlebitis, severe lower extremity peripheral vascular disease, presence of a documented aortic aneurysm requiring surgical repair, and pregnancy [1].
The 35-treatment sessions are typically completed once daily, Monday through Friday, for 7 weeks. However, extensions may be warranted for patients who display a late onset of improvement in symptoms. Patients are discouraged from missing scheduled sessions as lack of adherence to protocol may negatively affect the overall results. Body weight, blood pressure, heart rhythm, and symptom assessment are recorded by the technician prior to each treatment session. The intended 60-minute treatment session is completed with as few interruptions as possible to produce the full benefit of the treatment. Although the treatment is generally well tolerated, blistering and bruising of the legs, leg pain, and back pain may occur in some patients [1].
Results
There have been multiple invasive studies that evaluated the hemodynamic effect of EECP on coronary flow. Michaels, et al evaluated the change in diastolic and systolic pressure in the coronaries, aorta, and intracardiac pressure while undergoing EECP with the help of left heart catheterization [7]. Central aortic pressure, intracoronary pressure, and intracoronary Doppler flow was measured while the patient was undergoing EECP in the Catheterization laboratory. The results unequivocally showed that there is a clear increase in coronary blood flow velocity and pressure during diastole with inflation of the cuff representing diastolic augmentation of the blood flow. Left ventricular afterload was reduced during systole with deflation, reducing the left ventricular work.
In a study by Sahebjami, et al, it was found that the frequencies of angina were linearly reduced in both diabetics and non diabetics after EECP therapy, but it was significant only in non-diabetic patients. Furthermore, the angina reduction only started occurring in the 5th week. It appears that diabetes is one of the obstacles for successful EECP therapies [8].
In an arteriogenesis network trial, it was shown that EECP improves fractional flow reserve and coronary collateral flow index. It has also been shown that EECP improves global left ventricular function in patients with coronary artery disease [9]. This was demonstrated by left heart catheterization at baseline and in 7 weeks after EECP therapy in patients with stable coronary artery disease with at least one stenosis amenable to PCI. Invasive measurements of FFR and pressure derived collateral flow index were measured. The results were compared to a control group with no EECP. Results showed direct evidence for stimulation of coronary angiogenesis. This study indicates other modalities of benefit from EECP other than the acute hemodynamic changes.
EECP has also shown to benefit endothelial function by enhancing the release of nitric oxide and regulating endothelin-1 release, both of which play a role in maintaining vascular hemostasis. Masuda et al showed that there is a significant increase in plasma NO levels and reduction in neuro hormonal factors like human ANP and BNP after EECP treatment [10]. It also showed improved perfusion at rest and after dipyridamole in ischemic territories of myocardium on PET study after EECP, suggesting that development and recruitment of collateral vessels is one of the mechanisms of benefit [10].
EECP was shown to be effective in treating angina in patients with ischemic cardiomyopathy after CABG [11] although this is a small study with only 40 subjects. More studies are needed in this group of patients before it can be formally recommended.
Discussion
Further studies are needed to delineate the exact mechanism of both long term and short term benefit from EECP in chronic angina. Wu E et al conducted a qualitative study assessing the experiences of patients undergoing EECP therapy for refractory angina. The study showed that the patients were not that familiar with this treatment option prior to therapy [12]. This demonstrates the need for further education of patients and providers since it is a safe treatment modality with relatively limited side effects for refractory angina pectoris and severe congestive heart failure which also improves quality of life.
References
- Sharma U, Ramsey HK, Tak T (2013) the role of enhanced external counterpulsation therapy in clinical practice. Clin Med Res 11: 226–32.
- Wu E, Broström A, Mårtensson J (2019) Experiences of Undergoing Enhanced External Counterpulsation in Patients with Refractory Angina Pectoris: A Qualitative Study. J Cardiovasc Nurs 34: 147–158.
- Yang DY, Wu GF (2013) Vasculoprotective properties of enhanced external counterpulsation for coronary artery disease: beyond the hemodynamics. Int J Cardiol 166: 38–43.
- Soroff HS, Birtwell WC, Giron F, Collins JA, Deterling RA (1965) Support of the systemic circulation and left ventricular assist by synchronous pulsation of extramural pressure. Surg Forum 16: 148–50.
- Medical Advisory Secretariat (2006) Enhanced External Counterpulsation (EECP): An Evidence-Based Analysis. Ont Health Technol Assess Ser6: 1–70.
- Li B, Chen S, Qi X, Wang W, Mao B, et al (2018) The numerical study on specialized treatment strategies of enhanced external counterpulsation for cardiovascular and cerebrovascular disease. Med Biol Eng Comput 56: 1959–1971.
- Michaels AD, Accad M, Ports TA, Grossman W (2002) Left ventricular systolic unloading and augmentation of intracoronary pressure and Doppler flow during enhanced external counterpulsation. Circulation 106: 1237–42.
- Sahebjami F, Madani FR, Komasi S, Heydarpour B, Saeidi M, et al (2019) Refractory angina frequencies during 7 weeks treatment by enhanced external counterpulsation in coronary artery disease patients with and without diabetes. Ann Card Anaesth 22: 278–282.
- Maryam Esmaeilzadeh, Arsalan Khaledifar, Majid Maleki, Anita Sadeghpour, Niloufar Samiei, et al (2009) Evaluation of left ventricular systolic and diastolic regional function after enhanced external counterpulsation therapy using strain rate imaging. European Journal of Echocardiography 10: 120–126.
- D Masuda, R Nohara, T Hirai, K Kataoka, L.G Chen, et al (2001) Enhanced external counterpulsation improved myocardial perfusion and coronary flow reserve in patients with chronic stable angina. Evaluation by13N-ammonia positron emission tomography. European Heart Journal 22: 1451–1458.
- Abdelwahab AA, Elsaied AM (2018) Can enhanced external counterpulsation as a non-invasive modality be useful in patients with ischemic cardiomyopathy after coronary artery bypass grafting? Egypt Heart J 70: 119–123.
- Wu E, Broström A, Mårtensson J (2019) Experiences of Undergoing Enhanced External Counterpulsation in Patients With Refractory Angina Pectoris: A Qualitative Study. J Cardiovasc Nurs 34:147–158.