Stress fractures of the femoral neck (sFNF) are rare and occur mostly in athletes and military personnel or in the osteoporotic elderly. The incidence rate of sFNFs has been found to be 100/100.000 person-years in a military population, while bilateral sFNFs are much rarer and not presented by an incident rate in the literature. Available literature largely focuses on athletes and military personnel [1-13] as protentional candidate for SFNF. Prospective series show that 8% of stress fractures in competitive track and field athletes are located in the femur and 5% of stress fractures in a military population are in the femoral neck. A more recent registry study found a dominance of stress fractures in younger patients (<60 years) compared to the elderly; 5.8% versus 1.1% of all femoral neck and basocervical fractures. Fullerton described the symptoms and clinical findings in 49 military recruits with sFNFs.
87% had anterior groin pain and 19% nightly pain and was preceded by a long run or march in 40% of patients. Tenderness to inguinal palpation was present in 62% of cases and 79% had pain in extremes of hip range of motion while heel percussion very rarely elicited pain [1-14].
Early diagnosis is important to prevent progression into a displaced fracture. In a series of 19 military recruits with displaced sFNFs, 6 patients developed necrosis of the femoral head despite surgery and a total of 13 patients eventually developed osteoarthritis of the hip. Other military series describes femoral head necrosis in 23.8% of patients with a displaced sFNFs during a 28 month follow up period despite surgery [15]. Primary x-rays (antero-posterior and axial) may be inconclusive and can cause a delay in diagnosis. This was evident in a study where 90% of military recruits with an MRI-confirmed sFNF had a negative plain radiograph prior to the MRI [16]. Another military study found a sensitivity of only 37% for plain radiography in detecting pelvic or hip stress fractures [7], while MR has a sensitivity of 100%.
Case Report
This case report concerns a 55-year-old female who developed bilateral sFNF sequentially with osteopenia as the only risk factor. The patient was initially referred for an evaluation at our orthopedic outpatients clinic with complaints of right-sided deep groin pain, c-shaped pain and a feeling of the hip ”giving in” for the past 10 weeks. Recent x-ray showed no fracture. An earlier x-ray of the hip and pelvis two years prior had revealed minimal arthrosis and retroversion of the acetabulum. No valgus or varus malalignment was found. Labral injury was suspected and an MRI-arthrography was ordered but failed to visualize the labrum due to extracapsular placement of contrast fluid. Surprisingly, the scan revealed minimal callus formation at the right femoral neck as a sign of a healed fracture. Due to already being healed, the right-sided sFNF was treated conservatively. The patient was admitted to the emergency department 2½ years later with identical symptoms now arising from her left hip. Plain radiographs and CT-scan of pelvis and the hip showed no fracture. MR revealed an incomplete tension-sided fissure in the femoral neck involving less than 50% of femoral neck width. The patient was in pain and signs of healing were absent on the MRI. The left sFNF was therefore treated surgically, to prevent further displacement.
The patient was postmenopausal and had a family history with disposition to osteoporosis. BMI was 28,4. Prior to the first orthopedic evaluation, 2.5 years earlier, a DEXA-scan showed osteopenia with a T-score of the spine of -2,0 and the hips of -1,9/-1,7. The patient described a normal diet with supplemental calcium and magnesium tablets but had not previously received pharmacological treatment for osteopenia. She had ceased smoking several years prior and rarely consumed alcohol. Because of the right sided sFNF, she was examined thoroughly by an endocrinologist. Blood tests showed normal levels of vitamin D and calcium and no disturbance in kidney function or thyroid and parathyroid. Indicators of auto-immune disease or myelomatosis were normal. She had a slightly elevated ALAT which was deemed unrelated. By advice from the endocrinologist the patient started yearly zoledronic acid treatment.
Between the two hip fractures, she was diagnosed with a stress fracture of the left 2nd metatarsal and low-energy fractures of a single rib and a right-sided distal radius fracture. All were treated conservatively. The right sFFN was treated conservatively because of the late clinical diagnosis.16 weeks after onset of symptoms, the patient was painless and ambulatory. She was advised against sports for another four months. The left sFFN was, on the contrary, surgically treated with 3 parallel screws on the day of admittance to the emergency department and she was allowed full weight-bearing postoperatively. The patient felt an immediate reduction in pain after surgery. After two months the patient still had a pain rating of NRS 3-4 during physical therapy but was able to walk 5 kilometers. Walking distance increased with physical therapy and she was free of pain and started jogging 6 months postoperatively (Figures 1 and 2).
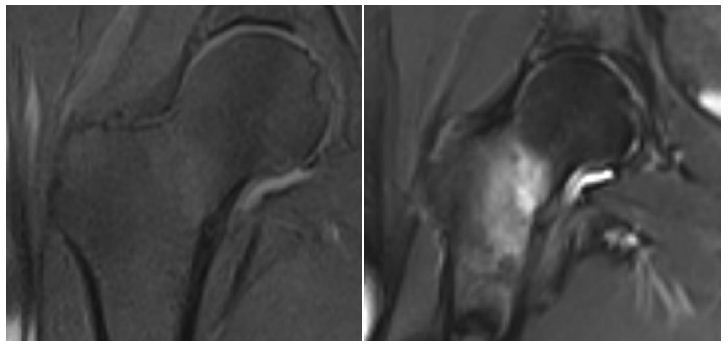
Figure 1: MRI of the right hip showing a stress fracture of the femoral neck with callus formation on the medial side. The fracture line is incomplete, and it is visible on the medial side and does not extend to the opposite cortex. A: T1 weighted TSE sequence B: T1 weighted TIRM sequence.
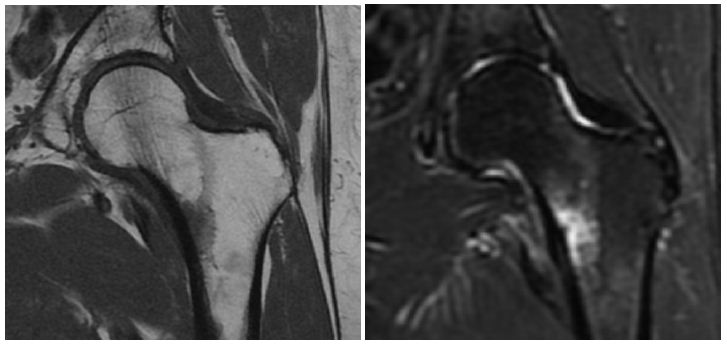
Figure 2: Left hip MRI showing bone edema in the medial distal collum femoris. A: Coronal T1 weighted MRI with low signal in the affected area. B: Coronal STIR MRI with high signal. A small fissure is visible and interpreted as an incomplete fracture line.
Discussion
Treatment of undisplaced sFNFs is debated, and surgeons must weigh the risks and benefits of conservative treatment versus surgery. Conservative treatment requires a period of reduced activity and carries a risk of displacement. In a Swedish registry study on undisplaced or minimally displaced sFNF and basocervical fractures, 3 og 17 patients that were treated non-operatively would later require internal fixation due to fracture displacement. Another 3 patients received late surgical treatment for persistent pain or femoral head necrosis, which in total corresponds to 35% of patients treated surgically following a choice of primary non-operative treatment. This was higher than the overall rate of reoperation or late surgery of 28% and higher than the reoperation rate of 10% for the patients primarily treated with internal fixation for displaced or undisplaced fractures.
Osteosynthesis seems effective in preventing secondary displacement and allows for early weight bearing but carries a risk of surgical complications. Removal of implants at a second operation due to pain occurs as often as 14% in sFNFs (both displaced and undisplaced). Surgical site infection (SSI) is also a concern. Although incidence of SSI is difficult to estimate in sFNFs, extrapolation from studies including traumatic femoral neck fractures may provide an indication of the frequency of infection in stress fractures. In patients below 60 years of age with all-cause femoral neck fractures, the risk of surgical site infection in retrospective studies is 5.1% [17]. Incidence rates in traumatic versus stress fractures may differ due to differences in surrounding tissue damage from trauma and differences in patient characteristics. Furthermore, risk of avascular necrosis and non-union is not completely eliminated with internal fixation and fixation failure can occur [18]. Two relatively large retrospective MRI studies have identified prognostic fracture characteristics that may help guide the surgeon in choice of treatment.
Quinquilla et al. [19] reviewed 156 cases of sFNF in a military population and divided fractures into 4 grades based on MRI. Grades I and II had bone marrow edema of less or more than 6mm but no fracture line. Grades III and IV had fracture lines of less or more than 50% of neck width on coronal MRI. Conservative treatment of sFNFs of grades I, II and III did not result in displacement or even progression to a higher fracture grade. 3 of 21 patients with a fracture line of >50% of neck width (grade IV) were treated conservatively while the remaining 18 had surgical fixation.
There was no report of displacement in the conservatively treated fractures indicating this treatment option is viable in the military population.
Steele et al. [20] retrospectively reviewed 305 cases of sFNFs in a military population. In this cohort, patients were treated non-operatively with toe-touch-weight bearing with crutches if they had bone marrow edema or a fracture line <50% of femoral neck width on MRI and surgically if they had a fracture line of >50% of the femoral neck width. On subsequent progression on MRI at 6 weeks follow-up, conservatively treated patients would require surgery. A total of 75 (24.6%) patients required surgery and of these patients 48 had primary operations and 27 after the MRI at 6 weeks follow up. No patients who initially had edema without fracture line would later need surgery per protocol. Out of those patients with a fracture line <50% of femoral neck width, 27 of 103 (26%) progressed on follow-up MRI and were treated surgically secondarily. Effusion on primary MRI was correlated with later progression with a relative risk of 8.02 (CI 2.99-21.5; p<0.0001) and in these patients, surgery should strongly be considered. No patients with an undisplaced sFNF progressed to displacement.
In the case presented here, surgical treatment was chosen for the left side even though the fracture line was <50% of femoral neck width. Despite the retrospective studies by Steele and Quinquilla suggest similar fractures are able to heal without surgery, 26% would require surgery due to progression on follow-up MRI. Furthermore, extrapolating from young military recruits to a postmenopausal woman with repeated stress fractures is uncertain and avoiding displacement is crucial. Surgery was performed to allow immediate weight-bearing and to prevent dislocation.
Conclusion
This is a rare case of bilateral sFNFs in a middle-aged woman with and osteopenia as the only risk factor. Stress fractures of the femoral neck may have an insidious onset of symptoms and absence of trauma and the primary x-ray is often negative while MRI is gold standard. Treatment can be conservative or surgical depending on fracture pattern and patient characteristics.
References
- Egol KA, Koval KJ, Kummer F, Frankel VH (1998) Stress Fractures of the Femoral Neck. Clinical Orthipaedics and Related Research 348: 72-78. [crossref]
- Niva MH, Kiuru MJ, Haataja R, Pihlajamäki HK (2005) Fatigue injuries of the femur. Journal of Bone and Joint Surgery – Series B 87: 1385-1390. [crossref]
- Sundkvist J, Möller M, Rogmark C, Wolf O, Mukka S (2022) Stress fractures of the femoral neck in adults: an observational study on epidemiology, treatment, and reoperations from the Swedish Fracture Register. Acta Orthop 93: 413-416. [crossref]
- Kuhn KM, Riccio AI, Saldua NS, Cassidy J (2010) Acetabular retroversion in military recruits with femoral neck stress fractures. Clin Orthop Relat Res 468: 846-851. [crossref]
- Snyder RA, Koester MC, Dunn WR (2006) Epidemiology of stress fractures. Clin Sports Med 25: 37-52. [crossref]
- Pihlajamaki H, Ruohola J, Kiuru M, Visuri T (2006) Fractures in Military Recruits. J Bone Joint Surg Am 88: 1989-1997.
- Kiuru MJ, Pihlajamaki HK, Ahovuo JA (2003) Fatigue stress injuries of the pelvic bones and proximal femur: Evaluation with MR imaging. Eur Radiol 13: 605-611.
- Kiuru MJ, Pihlajamaki HK, Hietanen HJ, Ahovuo JA (2002) MR imaging, bone scintigraphy, and radiography in bone stress injuries of the pelvis and the lower extremity. Acta Radiol 43: 207-212.
- Pihlajamäki HK, Ruohola JP, Weckström M, Kiuru MJ, Visuri TI (2006) Long-term outcome of undisplaced fatigue fractures of the femoral neck in young male adults. Journal of Bone and Joint Surgery – Series B 88: 1574-1579. [crossref]
- Fullerton LRJ, Snowdy HA (1988) Femoral Neck Stress Fractures. Am J Sports Med 16(4). [crossref]
- May LA, Chen DC, Bui-Mansfield LT, O’Brien SD (2017) Rapid magnetic resonance imaging evaluation of femoral neck stress fractures in a U.S. active duty military population. Mil Med 182: e1619-e1625. [crossref]
- Matheson GO, Clement DB, Mckenzie DC, Taunton JE, Lloyd-Smith DR, et al (1987) Stress fractures in athletes: A study of 320 cases. Am J Sports Med 15: 46-58. [crossref]
- Neubauer T, Brand J, Lidder S, Krawany M (2016) Stress fractures of the femoral neck in runners: a review. Research in Sports Medicine 24: 185-199. [crossref]
- Bennell KL, Malcolm SA, Thomas SA, Wark JD, Brukner PD (1996) The incidence and distribution of stress fractures in competitive track and field athletes: A twelve-month prospective study. American Journal of Sports Medicine 24: 211-217.
- Lee CH, Huang GS, Chao KH, Jean JL, Wu SS (2003) Surgical treatment of displaced stress fractures of the femoral neck in military recruits: A report of 42 case. Arch Orthop Trauma Surg 123: 527-533. [crossref]
- May LA, Chen DC, Bui-Mansfield LT, O’Brien SD (2017) Rapid magnetic resonance imaging evaluation of femoral neck stress fractures in a U.S. active duty military population. Mil Med 182: e1619-e1625. [crossref]
- Slobogean GP, Sprague SA, Scott T, Bhandari M (2015) Complications following young femoral neck Injury 46: 484-491. [crossref]
- Sundkvist J, Möller M, Rogmark C, Wolf O, Mukka S (2022) Stress fractures of the femoral neck in adults: an observational study on epidemiology, treatment, and reoperations from the Swedish Fracture Register. Acta Orthop 93: 413-416. [crossref]
- Rohena-Quinquilla IR, Rohena-Quinquilla FJ, Scully WF, Evanson JRL (2018) Femoral neck stress injuries: Analysis of 156 cases in a U.S. military population and proposal of a new mri classification system. American Journal of Roentgenology 210: 601-607. [crossref]
- Steele CE, Cochran G, Renninger C, Deafenbaugh B, Kuhn KM (2018) Femoral neck stress fractures: MRI risk factors for progression. Journal of Bone and Joint Surgery – American Volume 100: 1496-1502. [crossref]