Abstract
Introduction: Bilateral optic neuropathy caused by the novel coronavirus SARS-CoV2 (COVID-19).
Case report: A 25 years old female COVID-19 (+) applied to our clinic with complaints of bilateral progressive visual loss. Two weeks prior to onset of eye and vision symptoms, she had tested positive for coronavirus disease (COVID-19) virus by nasopharyngeal polymerase chain reaction (PCR) after developing symptoms of shortness of breath and cough. One week prior to her admission, bilateral blurred and vision loss progresivvely. In her ophthalmological examination; right and left visual aquity were 10/200 with blurred vision and ocular tensions were 15 mmHg and 16 mmHg, right and left, respectively. Anterior segment in both eyes were natural, there were no active cells, however, there were optic disc edema and retinal edema in both eyes. The diffusion cranial MR was normal.
Discussion: Optic neuropathies is a clinical diagnosis based on the history and examination findings, generally. Because important findings on funduscopic examination help differentiate typical from atypical cases of optic neuritis, an ophthalmologic examination can be considered in the clinical evaluation. Our patient is believed to have acute bilateral optic neuropathies induced by COVID-19 infection. Ispite of optic neuropathies in young ages are usually associated with MS, our patient is an interesting and rare case induced by COVID-19 infection with bilateral optic neuropathies.
Keywords
The novel coronavirus SARS-CoV2 (COVID-19), Optic neuropathy
Introduction
Optic neuropathies in adults are usually unilateral and commonly linked to multiple sclerosis (MS). It usually occurs as sudden onset of visual loss associated with pain on eye movement and progress in its course to reach its maximum deficit in a week [1]. Diagnosis is usually clinical based on history and examination findings. Brain and orbital imaging such as magnetic resonance imaging (MRI) help in the diagnosis in most cases. After confirmation, treatment is usually standart. Bilateral acute optic neuropathies are seen rarely, particularly in individuals without known systemic inflammatory or autoimmune disorders.
Case Presentation
A 25 years old female COVID-19 (+) (the novel coronavirus SARS-CoV2) patient came to our clinic with bilateral vision loss in august 2021. Two weeks prior to onset of eye and vision symptoms, she had tested positive for coronavirus disease (COVID-19) virus by nasopharyngeal polymerase chain reaction (PCR) after developing symptoms of shortness of breath and cough. She was quarantined at her home and treated symptomatically with improvement; she never required hospitalization for his respiratory illness nor medications including hydroxychloroquine.
One week prior to her admission, bilateral blurred and vision loss progresivvely. She has no past medical history presented from clinic with bilateral eye pain and vision loss and family history of any neurological or immunological diseases. In her ophthalmological examination; right and left visual aquity were 10/200 with blurred vision and ocular tensions were 15 mmHg and 16 mmHg, right and left, respectively. Anterior segment in both eyes were natural, there were no active cells, however, there were optic disc edema and retinal edema in both eyes (Figures 1 and 2), and also seen in optic coherence tomography (OCT) (Figures 3 and 4). The diffusion cranial MR was normal.
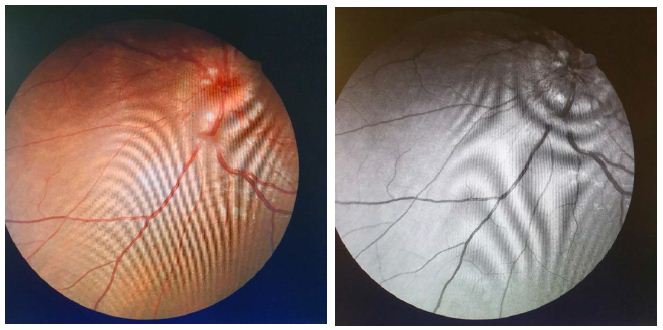
Figure 1: Right eye fundus photography
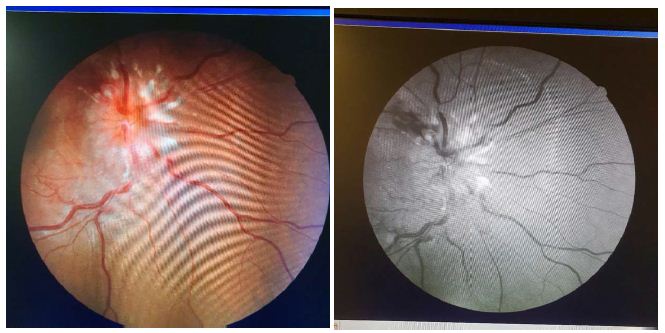
Figure 2: Left eye fundus photography
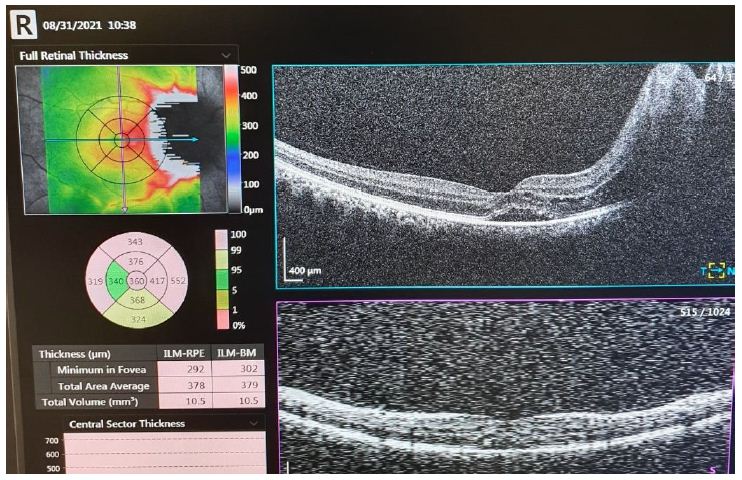
Figure 3: Optic coherence tomography of right eye
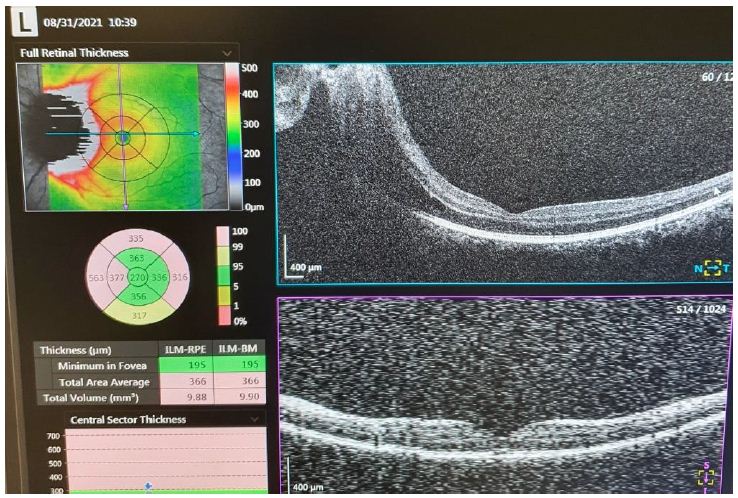
Figure 4: Optic coherence tomography of left eye
Our patient was started on methylprednisolone 1 g every 24 hours for a total of 5 days/doses. Within 48 hours, his vision and eye pain had shown significant improvement. By day of discharge, our patient had complete restoration of vision in the left eye with remarkable but not complete vision recovery in the right eye. He was discharged on a tapering dose of prednisone over 4 weeks with planned follow-up with ophthalmology and neurology.
Discussion
Optic neuropathy is defined as a demyelinating, inflammatory condition that causes acute, usually monocular, visual loss. It is highly associated with MS, and it is the presenting feature in 15% to 20% of these patients and occurs in 50% of them at some time during their illness [2].
It is believed that the demyelination in optic neuropathies is immune-mediated, but the exact targeted antigens remain unknown [3].
Optic neuropathies is a clinical diagnosis based on the history and examination findings, generally. Because important findings on funduscopic examination help differentiate typical from atypical cases of optic neuritis, an ophthalmologic examination can be considered in the clinical evaluation. MRI of the brain and orbits with gadolinium contrast provide a better assessment of the diagnosis in most cases. Further diagnostic testing, such as lumbar puncture, is done to exclude other causes of visual loss in atypical cases. However, around 60% to 80% of patients with acute optic neuropathies have nonspecific findings in the CSF such as lymphocytes and elevated proteins [4].
Our patient is believed to have acute bilateral optic neuropathies induced by COVID-19 infection. Once the diagnosis of optic neuropathies is made, treatment is usually straightforward with intravenous methylprednisolone (typically 1 g per day for 3 days) often followed by oral prednisone (1 mg per kg per day for 11 days), with subsequent tapering over a period of 4 days [2]. Treatment is associated with a more rapid recovery of vision by 2 to 3 weeks with no impact on long-term visual function. Therefore, a follow-up with neurology and ophthalmology after discharge is recommended to reach a final diagnosis in cases like this.
Ispite of optic neuropathies in these young ages are usually associated with MS, our patient is an interesting and rare case induced by COVID-19 infection with bilateral optic neuropathies.
Conclusion
Our patient described in this clinical vignette has signs and symptoms typical of acute bilateral demyelinating optic neuritis on his presentation. His evaluation with brain and orbital MRI along with lumbar puncture to determine the possibility of MS or other autoimmune disease was negative as well as other laboratory assessment. Therefore, we believe his infection with COVID-19 virus has triggered his immune system to present these findings. COVID-19 virus infection is causing a huge impact in the world as pandemic; its extent as clinical disease is still poorly understood and explained.
Declaration of Interest
I have no declaration of interest.
References
- de la Cruz J, Kupersmith MJ (2006) Clinical profile of simultaneous bilateral optic neuritis in adults. Br J Ophthalmol 90: 551-554. [crossref]
- Balcer LJ (2006) Optic neuritis. N Engl J Med 354: 1273-1280. [crossref]
- Söderström M, Link H, Xu Z, Fredriksson S (1993) Optic neuritis and multiple sclerosis: anti-MBP and anti-MBP peptide antibody-secreting cells are accumulated in CSF. Neurology 43: 1215-1222. [crossref]
- Jacobs LD, Kaba SE, Miller CM, Priore RL, Brownscheidle CM (1997) Correlation of clinical, magnetic resonance imaging, and cerebrospinal fluid findings in optic neuritis. Ann Neurol 41: 392-398. [crossref]