DOI: 10.31038/IDT.2022313
Abstract
Balb/c mice were challenged orally with increasing amounts or either B. anthracis Sterne or Ames spores in order to determine lethal gastrointestinal dose levels. Only a single animal succumbed at the 1010 spore challenge dose for Sterne. The oral LD50 for Ames was 108 spores with 100% survival at a challenge dose of 105. Re-challenge of the 109 and 1010 Sterne challenge and the surviving 106, and 107 Ames challenge animals with a lethal aerosol challenge of Ames resulted in all animals succumbing and no increase in mean time to death indicating no lasting immunological response was elicited after survival of oral-dosed spore challenge.
Keywords
Anthrax, Mouse, Oral challenge, Spores
Introduction
The murine-anthrax aerosol challenge model has become a proof of concept standard in the evaluation and development of therapeutics for the treatment of B. anthracis infections [1-6]. Because the model relies on a whole body exposure there have been concerns raised that murine ingestion of the anthrax spores through daily grooming after challenge may lead to gastrointestinal infection via the oral route thus complicating interpretation of study results. Additionally, post therapy survival could be enhanced by elicitation of an immune response through ingestion of anthrax spores [7,8].
Materials and Methods
B. anthracis Ames and Sterne spores were prepared according to the method of Leighton and Doi and were maintained in sterile water for injection [9]. Spores were diluted in sterile water to concentrations ranging from 100 to 1011 CFUs/ml to deliver in a 0.1ml oral volume challenge doses were administered by oral gavage to female Balb/c mice (6-8 weeks old) ranging from 10 to 1010 CFUs/mouse. To verify final bacterial concentrations and exposure doses, colonies were enumerated after serial dilution and plating on sheep blood agar (SBA) plates. The plates are incubated at 35ºC and colonies enumerated. Animals were observed 4 times per day and deaths recorded. All analyses were performed employing a stratified Kaplan-Meyer analysis with a log-rank test as implemented on Prism Version 5, GraphPad Software. Research was conducted under an IACUC approved protocol in compliance with the Animal Welfare Act, PHS Policy, and other Federal statutes and regulations relating to animals and experiments involving animals. The facility where this research was conducted is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care, International and adheres to principles stated in the 8th Edition of the Guide for the Care and Use of Laboratory Animals, National Research Council, 2011.
Surviving animals from the 109 and 1010 CFU Sterne and the 106 and 107 CFU Ames oral challenge groups were re-challenged two months later with an inhaled dose of 50-75 LD50 (LD50 = 3.4 x 104 CFU) of B. anthracis Ames strain spores by whole-body aerosol [1]. Aerosol was generated using a three-jet Collison nebulizer [10]. All aerosol procedures were controlled and monitored using the Automated Bioaerosol Exposure system operating with a whole-body rodent exposure chamber [11]. Integrated air samples were obtained from the chamber during each exposure using an all-glass impinger (AGI). Aerosol spore concentrations were determined from the AGIs by serially dilution and plating on SBA, as described above. The inhaled dose (CFU/mouse) of B. anthracis was estimated using Guyton’s formula [12].
Results
Survival results for the Ames spore oral challenge are shown in Figure 1. All mice receiving oral doses of 105 CFUs and below resulted in no deaths and all animals remained active without any clinical signs of infection. More importantly for oral challenge the development of clinical signs of illness or death was found to be two orders of magnitude above the aerosol LD50 of 3.4 x 104 CFUs for whole body exposure [1]. Animals challenged with spores from the Sterne strain were unaffected with only a single death observed at the highest dose of 1010 CFUs. The remainder of the animals all appeared healthy and active throughout the post challenge period. The lack of afforded protection as measured by survival (Figure 2) using mice pre orally challenged with either Ames or Sterne to a lethal aerosol challenge dose of Ames spores indicates that there is no long term immunity conveyed by orally delivered spores. In addition there was no shift in the calculated mean time to death of 48hrs between any of these groups and the control group, further evidence indicating a lack of protection by orally delivered spores.
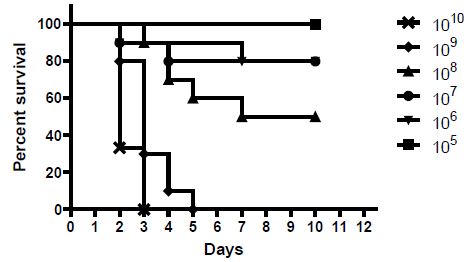
Figure 1: Female Balb/c mice (6-8 weeks old) in groups of 10 animals were challenged with oral doses of spores prepared from the B. anthracis Ames strain. Challenge amounts ranged from 10 to 1010 spores per mouse in 0.1 ml. Animals were observed and deaths recorded. The 10-105 challenges doses resulted in no deaths. A similar experiment was performed with spores of the Sterne strain resulting in only a single death at the 1010 CFU challenge dose (data not shown)
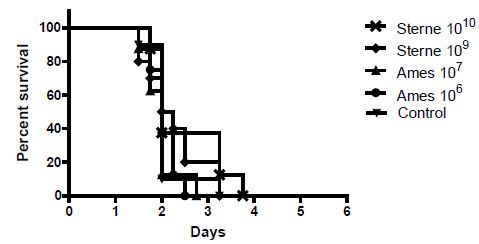
Figure 2: Surviving animals from the oral-LD50 studies were challenged two months after initial oral challenge with multiple LD50s of aerosolized B. anthracis Ames spores
Discussion
The oral LD50 for the Ames strain at 108 CFUs is well above any theoretical ingestion possibility in the aerosol model. Even if one were to assume that an entire aerosol dose would be deposited on only the fur of all the caged mice and one animal groomed itself and all nine of the cage mates, the maximum theoretical oral dose possible would be 105 CFUs which would be still be well below the LD50. Clearly, considering a realistic distribution of the spores during an aerosol challenge experiment, the maximum potential ingested dose would be one or more magnitudes below this predicted 105 CFU limit. In addition, from these experiments the observation of only a single death at only the 1010 CFUs challenge dose for the Sterne strain again indicates the importance of the capsule for virulence in any murine challenge model. These results are also consistent with previously described gastrointestinal models, which used Sterne strain susceptible mouse strains A/J [13] or DBA/2 [14] and required >107 CFUs/mouse in combination with anti-acid addition to achieve an LD50. Therefore the data would indicate that potential ingestion of anthrax spores following whole body aerosol challenge does not affect the currently understood inhalational disease progression as observed in the Balb/c mouse [1]. Additional evidence is in the lack of any pathology associated with the digestive tract following aerosol challenges [1,15(D. Fritz personal communication)]. The lack of any increase in mean time to death would also seem to reduce the possibility that any orally ingested spores would affect therapeutic results and their interpretation. These results do not rule out the possibility of short term stimulation of an innate immune response after aerosol challenge resulting from animal ingestion of spores. However, based on the results from this study, the oral dose would be so low it seems unlikely to invoke a meaningful immunologic response.
Conclusion
In conclusion, potential oral ingestion of anthrax spores after whole-body aerosol challenge is highly unlikely to have any effect on mortality, disease progression, immunity or therapeutic outcomes.
Funding
This research was funded by a Joint Science and Technology Office – Defense Threat Reduction Agency – Chemical Biological Defense grant: CB3848 (CBCALL12-THRFDA1-2-0209) PPE3.
References
- Heine HS, Bassett J, Miller L, Hartings JM, Ivins BE, et al. (2007) Determination of Antibiotic Efficacy against Bacillus anthracis In a Mouse Aerosol Challenge Model. Antimicrob Agents Chemother 51: 1373-1379. [crossref]
- Heine HS, Bassett J, Miller L, Purcell BK, Byrne WR (2010) Efficacy of Daptomycin Against Bacillus anthracis in a Murine Model of Anthrax-Spore Inhalation. Antimicrob Agents Chemother 54: 4471-4473. [crossref]
- Heine HS, Purcell BK, Bassett J, Miller L, Goldstein BP (2010) Activity of Dalbavacin against Bacillus anthracis In Vitro and in a mouse Inhalation Anthrax Model. Antimicrob Agents Chemother 54: 991-996. [crossref]
- Gill SC, Rubino CM, Bassett J, Miller L, Ambrose PG, et al. (2010) Pharmacokinetic-Pharmacodynamic Assessment of Faropenem in a Lethal Murine Bacillus anthracis Inhalation Postexposure Prophylaxis Model Antimicrob Agents Chemother 54: 1678-1683. [crossref]
- Heine HS, Bassett J, Miller L, Bassett A, Ivins BE, et al. (2008) Efficacy Oritavancin in a Murine Model of Bacillus anthracis Spore Inhalation Anthrax. Antimicrob Agents Chemother 52: 3350-3357. [crossref]
- Heine HS, Shadomy SV, Boyer AE, Chuvala L, Riggins R, et al. (2017) Evaluation of combination drug therapy for treatment of antibiotic-resistant inhalational anthrax in a murine model. Antimicrob Agents Chemother 61: e00788-17. [crossref]
- Kathania M, Zadeh M, Lightfoot YL, Roman RM, Sahay B, et al. (2013) Colonic Immune Stimulation by Targeted Oral Vaccine. Plos One 8: e55143. [crossref]
- Glomski IJ, Pris-Gimenez A, Huerre M, Mock M, Goossens PL (2007) Primary involvement of pharynx and peyer’s patch in inhalational and intestinal anthrax. Plos Path 3: e76. [crossref]
- Leighton TJ, Doi RH (1971) The stability of messenger ribonucleic acid during sporulation in Bacillus anthracis. J. Biol. Chem 246: 3189-3195. [crossref]
- May KR (1973) The Collison nebulizer description, performance and applications. J. Aerosol Sci 4:235-243.
- Hartings JM, Roy CJ (2004) The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J Pharm and Toxicol Meth 49:39-55.
- Guyton AC (1947) Measurement of the respiratory volumes of laboratory animals. Am J Physiol 150:70-77. [crossref]
- Xie T, Sun C, Uslu K, Auth RD, Fang H, et al. (2013) A new murine model for gastrointestinal anthrax infection. PLOS one 8: e66943.
- Tonry JH, Popov SG, Narayanan A, Kashanchi F, Hakami RM, et al. (2013). In vivo murine and in vitro M-like cell models of gastrointestinal anthrax. Microbes and Infection 15:37-44. [crossref]
- Lyons CR, Lovchik J, Hutt J, Lipscomb MF, Wang E, et al. (2004) Murine model of pulmonary anthrax: kinetics of dissemination, histopathology, and mouse strain susceptibility. Infect. Immun 72:4801-4809. [crossref]