Abstract
This review identifies and summarizes the current state of the literature on the reproductive health of women firefighters. Several alarming exposures were noted including chemical, biological, and non-chemical occupational risk factors. The existing literature supports an association between firefighting and higher rates of miscarriage, birth defects, labor and delivery difficulties, fetal mortality, possible fertility issues, and newborn health complications (e.g., jaundice, low birth weight). A significant gap in the literature was identified despite the growing concern among women firefighters regarding reproductive health, signaling the crucial need for further research. Consequently, the lack of research has precipitated uncertainty concerning appropriate firefighting duties during pregnancy and safe return to work post-partum, leading to an absence of effective policy and, in some cases, no policy within fire departments.
Introduction
The fire service is, by nature, an extremely dangerous job. Though touted as an exceptionally close-knit brotherhood, this ‘brotherhood’ employs the fewest women of all tactical occupations (including law enforcement and the military). Even the Marine Corps, where all members must be combat certified, outnumbers the fire service with its prevalence of women (9%) [1]. Women represent 11% of the volunteer fire service and only 5% of the career fire service [2]. With such a relatively small proportion of women, there is little evidence-based information detailing how the dangerous nature of the job impacts them specifically. More explicitly, there is a dearth of data regarding women-specific injury rates, mental health, substance use, cancer, and reproductive health.
As firefighter health research has expanded, there has been emerging interest in the health of women firefighters. Jahnke and colleagues [3] published data from a population-based epidemiologic cohort study that found that overall, women firefighters (n=31) were relatively healthy compared to their male counterparts. For instance, women evidenced a lower rate of overweight and obesity than men firefighters and were less likely to be obese when compared to women in the general population (civilians). Most women firefighters also exhibited good or excellent flexibility (66.6% career and 53.9% volunteer) and were in the “high” range of strength (70.6% career, 69.2% volunteer) on standardized tests of flexibility and torso strength, although the sample size was small, limiting generalizability [3]. Calls for additional research specific to the health of women firefighters and the unique, gender-specific impacts of occupational exposures are noted as critical research needs in the most recent National Fire Service Research Agenda [4].
Concerns about the impact of firefighting on reproductive issues among women were raised in the 1980-90s [5-8], but with little scientific follow-up. Potential reproductive health risks identified as possibly contributing to increased maternal complications include chemical, biological, and radiologic exposures from responding to incidents [5,7-9], as well as non-exposure related risks, such as the unique shift schedules common in the fire service, the extreme physiologic strain of emergency responses, and working in situations with high ambient temperatures and noise volumes [7]. Reproductive health is an emerging area of concern for firefighters, both men and women [10-13].
Currently, no guidelines for physicians and other health care providers outline the dangers of firefighting with specific considerations for pregnant firefighters. As a result, there is widespread confusion among women firefighters regarding when to limit or restrict firefighting duties when pregnant and when it is appropriate to return to work after giving birth. Recent research found that nearly 30% of fire departments do not have a policy for pregnant firefighters [10,12]. Potential injuries to firefighters and their offspring may occur due to insufficient information and guidance. In addition, the lack of literature may impact recruitment and retention in the fire service, further confounding finding reliable workers to fill open positions. The purpose of this project was to conduct a state of the science review of the current research available on women’s reproductive health and occupational exposures to serve as a foundation for additional work and as a reference for firefighters, departmental leadership, health and wellness personnel, occupational medical physicians, and obstetrics/gynecologists.
Methods
Researchers synthesized current literature in a systematic review. PubMed, a free resource containing more than 35 million citations and abstracts of biomedical literature, was used to search the below combinations of key terms (Table 1) in April-May 2022. All fields of publications were searched with any of the key fire terms and any of the reproductive keywords [e.g.: (fire) AND (reproductive health)]; (Table 1). Inclusion criteria included: English version of the abstract available; peer-reviewed article; contains research on firefighter-specific exposures; and included a reproductive health outcome. If more than one article with overlapping populations was retrieved, preference was given to the article with more comprehensive information. Review articles were included. Letters to the editor, commentaries, reports, theses/dissertations, and conference presentations/abstracts were excluded. Articles that did not explicitly include firefighters as their population were not included, though a table was added with several relevant articles as comparisons for discussion and as a source of additional information.
Table 1: Keywords
|
Fire Keywords |
Reproductive Keywords |
| Fire | Reproductive health |
| Firefighter | Maternal and child health |
| Arson investigator | Reproduction |
| Arson investigation | Fertility |
| Fire trainer | |
| Fire instructor | |
| Airport fire | |
| Airport firefighter | |
| Wildland firefighter | |
| Military firefighter |
Results
A total of 1,254 records were returned from the search of PubMed. Duplicate records (n=176) were removed prior to screening (See Figure 1, Prisma Diagram). A total of 1,078 article titles were screened for relevance; 1,056 were excluded (not relevant or did not include firefighters). Twenty-two articles were sought for retrieval, one was not available (there was no abstract or article, only a title/citation). The remaining 21 articles were assessed for eligibility. One report was excluded as it was a letter to the editor and not a peer-reviewed article, and five reports were removed due to relevance (not firefighter specific). A total of 15 articles are included in the review. Additionally, the references (n=44) from an unpublished literature review from Dr. Jahnke, a known expert in the field of firefighter health, were searched. Six reports were sought for retrieval and assessed for eligibility. Six articles were duplicates from the present literature search, and one was not firefighter specific. The remaining article was added to the list of eligible firefighter articles for this review (n=16; Table 2). An additional six studies that were not specific to firefighters are included in a separate table (Table 3) as they provide relevant exposure information related to pregnancy outcomes.
Table 2: Firefighter Studies Included in Review
|
Study ID |
Author (Year) |
Journal |
Article Type |
Country/State |
Number of Participants |
Key Takeaways |
| 1 | Agnew
(1991) |
Am J Ind Med | Review | USA | — | Summary of potential non-chemical hazards on FF reproductive health including heat, physical activity, noise, psychological stress, radiation, and biological agents. |
| 2 | Clarity
(2021) |
Environ Health | Epidemiologic | USA | N=84 women FFs | FFs had higher concentrations of PFOA, PFOS which impacted telomere length. Certain chemical exposures may affect carcinogenesis and other adverse health outcomes. |
| 3 | Davidson (2022) | Int J Environ Res | Epidemiologic | USA | N=106 | Firefighters had a 33% lower AMH value than non-firefighters. Years of firefighting was not associated with a decrease in AMH. |
| 4 | Engelsman (2021) | Reproduction and Fertility | Exploratory epidemiologic | Australia | N=20 male FFs | FF semen parameters were below WHO reference values for men. Increased frequency of fire exposure was associated with a reduction in normal forms, volume, sperm concentration, and count. |
| 5 | Evanoff
(1986) |
Am J Ind Med | Review | USA | — | Summarizes hazards faced by pregnant FFs (i.e.: physical exertion, hyperthermia, toxic agents, irritant gases, asphyxiant gases, other toxins) and recommends policy change. |
| 6 | Jahnke (2018) | Matern Child Health J | Epidemiologic | USA | N=1,821 women FFs | Nearly 25% of pregnancies ended in miscarriage for women FFs and rates of pre-term birth were also high. |
| 7 | Jung (2021) | Environ Health | Epidemiologic | USA | N=3,181 women FFs | 22% of FF pregnancies ended in miscarriage. FFs had 2.33 times greater risk of miscarriage compared to nurses. Structural Vol FFs had 1.42 times greater risk of miscarriage compared to Car. Among WL/WUI FFs, Vol FFs had 2.53 x the risk of miscarriage compared to Car. |
| 8 | Kehler (2018) | IFSJLM | Qualitative | USA | N=87 | Female FF reproductive health is of significant concern among FFs. |
| 9 | McDiarmid (1995) | Occ Med | Review | USA | — | There are male and female-mediated reproductive health effects of firefighting due to a number of different chemical and non-chemical hazards. |
| 10 | McDiarmid (1991) | Am J Ind Med | Review | USA | — | There are a number of chemical exposures that may contribute to adverse reproductive health outcomes in FFs. |
| 11 | Olshan (1990) | Am J Epidemiol | Epidemiologic | Canada | N=22,192 FF offspring | Among 20 birth defect groups studied, an association was found for paternal employment as a FF (relative to all other occupations) and increased risks were observed for ventricular septal defects and atrial septal defects among offspring. |
| 12 | Park (2020) | Ann Occup Environ Med | Epidemiologic | Korea | N=1,766 female FFs | Female FFs showed high rates of puerperium outcomes. Reproductive risks include shift work, sleep disruption, hyperthermia, noise, and physical tension. |
| 13 | Petersen (2019) | Am J Epidemiol | Epidemiologic | Denmark | N=4,710 | Among the full-time firefighters, the risk of male-factor infertility was increased in comparison with the sample of employees. Increase in infertility seemed restricted to duration of time employed as a firefighter. |
| 14 | Trowbridge (2022) | Environ Sci Technol | Epidemiologic | USA | N=86 | Thyroid hormone indicates biological changes potentially related to exposure to toxic chemicals. Women FFs had higher levels of flame retardants than office workers. High BDCPP exposure was associated with decreased thyroid hormone levels. |
| 15 | Trowbridge (2020) | Environ Sci Technol | Epidemiologic | USA | N=86 | FFs had higher mean concentrations of PFAS compared to office workers. It is unknown how PFAS effects reproductive health. |
| 16 | Watkins (2019) | WHI | Epidemiologic | Multiple | N=840 women FFs | There is a need for research and education into gynecological issues, heat exposure, and their effects on women FFs’ fertility and cancer risk. |
Table Notes: FF: firefighter. Vol: Volunteer. PFOA: Perfluorooctanoic Acid. PFOS: Perfluorooctane sulfonic acid. Car: Career. AMH: Anti-Müllerian Hormone. WHO: World Health Organization. WL/WUI: wildland/wildland urban interface. BDCPP: bis(1,3-dichloro-2-propyl)phosphate, a flame retardant metabolite. PFAS: per-and polyfluoroalkyl substances.
Table 3: Non-Firefighter or Non-Reproductive Studies Included in Review
|
ID |
Author (Year) |
Journal |
Article Type |
Country/State |
Number of Participants |
Key Takeaways |
| 17 | Abdo (2019) | Int J Environ Res Public Health | Epidemiologic | USA | N=535,895 | Exposure to wildfire smoke PM2.5 during the 2nd trimester was associated with increased rates of preterm birth. Maternal outcomes (gestational diabetes, hypertension) were also associated with wildfire smoke exposure. |
| 18 | Amjad (2021) | Environ Int | Review | Multiple | — | There is some evidence indicating that maternal wildfire exposure is associated with reduced birth weight and preterm birth. |
| 19 | Di Renzo (2015) | Int J Gynaecol Obstet | Review | International | — | With accumulating evidence of exposures and adverse health impacts related to toxic environmental chemicals, the International Federation of Gynecology and Obstetrics (FIGO) joins other leading reproductive health professionals in calling for action. FIGO recommends that reproductive and other health professionals advocate for policies to prevent exposure to toxic environmental chemicals. |
| 20 | Fabian (2010) | UL | Technical Report | USA | — | There are a number of exposures of concern to FFs that impact respiratory and cardiovascular health. These have been linked to acute and chronic effects. This report explores the size distribution of smoke particles generated in fires and the nature of chemical absorption. |
| 21 | Murphy (2021) | Int J Environ Res Public Health | Review | Multiple | — | Bushfire smoke is associated with poor pregnancy outcomes including reduced birth weight and increased risk of prematurity. |
| 22 | Perera (2005) | Environ Health Perspect | Epidemiologic | USA | N=373 | PAH exposure during pregnancy may have contributed to reduced fetal growth in women exposed to the WTC event. |
| 23 | Treitman (2010) | Am Ind Hyg Assoc J | Epidemiologic | USA | — | The concentrations of eight air contaminants suspected of causing acute and chronic health problems for firefighters were measured in over 200 fires in the City of Boston using a personal air sampler. |
Table Notes: FFs: Firefighters. PM2.5: fine particulate matter. PAH: polycyclic aromatic hydrocarbons. WTC: World Trade Center.
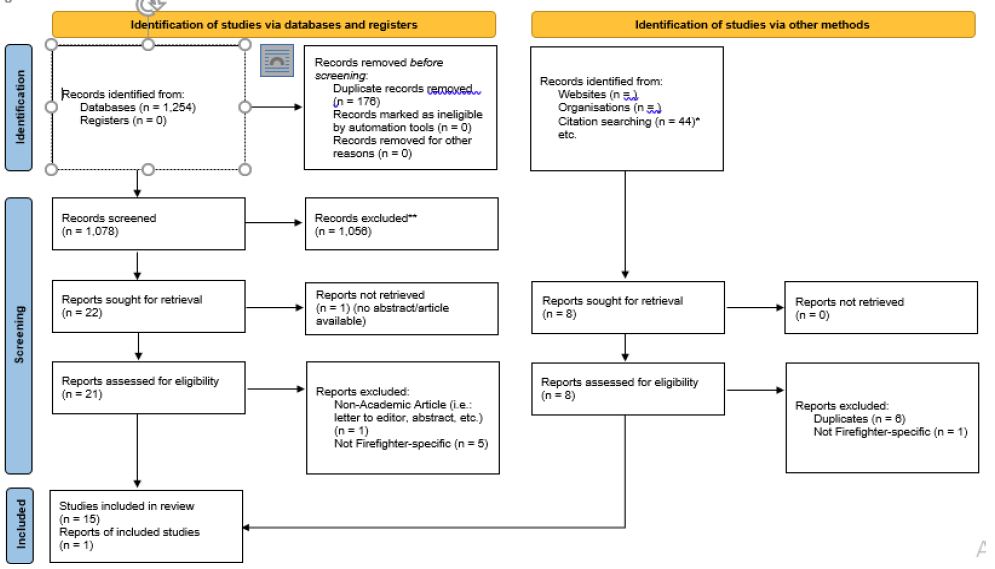
Figure 1: Prisma flow diagram.
*Citations examined from previous unpublished literature review (Jahnke, 2014)
**Records excluded did not meet inclusion criteria (not relevant [non-firefighter related, did not mention reproductive outcomes]; was not a peer-reviewed article; etc.)
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
Current research suggests significant reproductive dangers associated with firefighting can injure firefighters and harm their offspring. McDiarmid and colleagues [8] identified numerous male and female-mediated reproductive health effects due to firefighting, including various chemical and non-chemical hazards. The International Federation of Gynecology and Obstetrics has identified chemical exposures during pregnancy and breastfeeding as a threat to healthy human reproduction and development with implications for fertility, pregnancy, neurodevelopment, and cancer later in life [14]. Firefighters are potentially exposed to a plethora of toxic chemicals, both during active firefighting and while on-scene conducting overhaul activities after the fire is extinguished [15]. Chemicals present on the fireground include allergens and irritants (e.g., ammonia, hydrogen chloride, sulfur dioxide, phenol), asphyxiants (e.g., carbon monoxide, hydrogen sulfide, and carbon dioxide), and known carcinogens (e.g., polycyclic aromatic hydrocarbons and chromium) [5,9,15]. Recent research suggests that sub-micron sized chemical particles are still present during overhaul even when firefighters cannot see visible smoke [15]. In addition to the inhaled chemicals, firefighters face risks associated with exposure to residues of the products of combustion that become embedded in their personal protective equipment and are absorbed on their skin post-incident [15].
Several of the chemicals identified as key risks to pregnant women are the same as those found to be present on the fireground. For instance, preliminary data from the 1980s indicated that exposure to carbon monoxide increases the risk of birth defects among pregnant women firefighters [8,16]. McDiarmid et al. [16] and Evanoff and Rosenstock [5] cited several known products of combustion that are believed to impact reproductive health in either animal or human models including: aldehydes (e.g., acetaldehyde, formaldehyde, acrolein), benzene, carbon dioxide, chloroform, dichlorofluoromethane, hydrogen chloride, hydrogen cyanide, methylene chloride, nitrogen dioxide, nitrogen oxide, perchloroethylene, sulfur dioxide, toluene, trichloroethylene, and trichlorophenol.
Recent concerns regarding perfluoroalkyl substances (PFAS) and firefighter health have emerged. Though evidence is limited regarding how much of these “forever chemicals” are “safe” in the human body, there are concerns related to PFAS and human health. Through the Women Firefighters Biomonitoring Collaborative, Trowbridge and colleagues [17] measured serum concentrations of PFAS in women firefighters compared to office workers and found firefighters had higher mean concentrations of PFAS. Clarity and colleagues [18] measured serum concentrations of PFAS and found significant associations between perfluorooctanoic acid (PFOA) and perfluorooctanesulfonic acid (PFOS; both kinds of PFAS) and telomere length. Telomere length is associated with fertility (longer telomeres indicating fertility). When stratified by occupation, there were stronger associations among firefighters compared to office workers, meaning firefighters were more likely to have reduced telomere length indicating potential infertility. Trowbridge and colleagues [19] also examined exposure to flame retardants (a class of suspected endocrine-disrupting chemicals) and thyroid hormone dysregulation among women firefighters. They found higher levels of flame retardants among women firefighters, which was associated with decreased thyroid hormone levels. Though thyroid hormone dysregulation can lead to endocrine disruption and breast cancer risk, more research is necessary to understand the mechanisms by which exposure to flame retardants may impact firefighter health and fertility.
Davidson and colleagues [13] recently examined anti-mullerian hormone (AMH), which measures ovarian reserve and can indicate fertility. AMH indicates a woman’s ability to produce eggs that can be fertilized for pregnancy; this number peaks during childbearing years and decreases with age. AMH levels help show how many potential egg cells a woman has left and may be a useful biomarker for measuring the effects of exposures that target the ovaries. A reduction in AMH has been associated with inhaled environmental toxicants such as cigarette smoking, burning fuels indoors for cooking, and the use of pesticides. Firefighters had a 33% lower AMH value compared to non-firefighters, potentially indicating issues with fertility [13]. More research is necessary to determine the mechanisms by which firefighting could impact AMH levels and affect fertility.
In addition to fertility, women firefighters are concerned about returning to work and continuing to breastfeed their offspring. Burgess and colleagues released unpublished preliminary results from a small pilot trial examining women firefighters’ breastmilk. Preliminary recommendations suggested that women firefighters who are breastfeeding should not be exposed to “Immediately Dangerous to Life or Health” (IDLH) environments to protect exposing their offspring to toxins (Aryl Hydrocarbon Receptor, AhR) that can be found in breastmilk for up to 72 hours post-incident. However, a larger, more recent study [20] found no variation in polybrominated diphenyl ethers (PBDEs) or AhR response in breastmilk extracts of firefighters and non-firefighters. There was no significant variation after fire exposure, further confounding recommendations for breast feeding after returning to work. It is important to note that these studies only examined specific chemical exposures. Women firefighters may choose to “pump and dump” (pumping to expel breastmilk but discarding it due to potential presence of carcinogens) after returning to work if they have been exposed to live fire conditions (IDLH atmosphere or other chemicals present). More research is necessary to examine all possible chemicals present in breast milk after fire exposure.
Park and colleagues [21] examined hospital admissions for pregnancy, childbirth, and puerperium (the period approximately 6 weeks after childbirth) outcomes among women firefighters in Korea. They found, compared to the general population of women in Korea, the women firefighters’ standardized admission ratios (SARs) were higher in all admissions for puerperium outcomes; pregnancy and abortive outcomes; maternal disorders related to pregnancy; maternal hospitalization for adverse outcomes related to the fetus and amniotic cavity; labor and delivery complications; and complications related to puerperium.
Other non-chemical occupational risks also may impact reproductive health. Evanoff and Rosenstock [5] identified reproductive hazards associated with firefighting as early as 1986. Agnew and colleagues [7] also summarized potential non-chemical hazards associated with firefighter reproductive health in 1991. Collectively, they include heat, physical activity, noise, psychological stress, radiation, and biological agents. The physiologic strain of fire and rescue activities can negatively impact reproductive health [22]. Given the changes in a woman’s body as a result of pregnancy, extreme physical activity can put them at risk for injury [22]. Evidence also suggests that pregnant women’s exposure to loud noises (e.g., air horns, sirens) may lead to lower fetal weight and increased risk of fetal mortality [22,23]. In an international survey of women firefighters, Watkins and colleagues [24] found women firefighters in North America reported a higher prevalence of lower back (49%) and lower limb (51%) injuries than the other groups (United Kingdom, Ireland, Australia, and mainland Europe). North American firefighters reported more heat-related illnesses (45%) than respondents from other countries (36%). Thirty-nine percent of respondents thought their menstrual cycle and menopause affected work. It is important to note that both men and women firefighters suffer from fireground and training injuries and heat illness; however, women firefighters also must accommodate changing hormonal cycles which can impact fertility and the body’s ability to handle heat stress. More research is necessary to ensure women firefighters are protected from these dangers if/when they decide to become pregnant while in the fire service.
Women firefighters have exhibited significant concern regarding their reproductive health [25] and have identified a lack of available resources [10]. In a study of 1,821 women firefighters [10], participants reported between 22.6% and 31.7% of pregnancies ended in miscarriage. The crude overall rate of miscarriage across pregnancies while in the fire service was 27.0%, two times higher than the US national average [10]. Jahnke and colleagues also found high rates of pre-term birth, jaundice, and low birth weight among women firefighters [10]. Alarmingly, nearly a quarter of respondents (23.9%) reported their department had no policy related to pregnancy, and 20% reported their department had no policy related to maternity leave. Jung and colleagues [12] found similar results in a follow-up study; 22% of firefighters in the sample of 1,074 women firefighters had experienced a miscarriage. As women aged, this risk increased; the age-standardized prevalence of miscarriage was 2.33 times greater compared to an occupational cohort of US nurses. Volunteer firefighters had 1.42 times the risk of self-reported miscarriage compared to career firefighters. Among wildland/wildland urban interface (WUI) firefighters, volunteers had 2.53 times the risk of miscarriage compared to their career counterparts [12].
Of note, fireground exposure risks are not limited to women. Research by Olshan and colleagues [23] in a cohort of firefighters suggested that toxic exposures experienced by men firefighters may increase the likelihood of birth defects among their offspring. More recently, Petersen and colleagues [11] found that full-time firefighters had an increased risk of infertility compared to non-firefighters, and this risk appeared to be associated with the length of time in the occupation of firefighting. Engelsman and colleagues [26] examined the fertility of firefighters via survey and semen analysis. In an exploratory study, they found that, overall, firefighter semen parameters were below World Health Organization reference values designated for fertility in men. Firefighters younger than 45 had a higher incidence of abnormal semen parameters (42%) than those aged 45 years or greater (9%). Increased frequency of fire exposure was associated with a reduction in normal forms, volume, sperm concentration, and total sperm count. While this is only an exploratory study (small sample size), results suggest an association between firefighting and male-factor fertility.
Discussion
Firefighting is a known dangerous occupation; however, specific considerations must be paid to firefighter reproductive health, including potential health concerns for firefighters’ offspring. While not specific to firefighters, our literature review returned several articles with relevant exposure data. While firefighters are provided with self-contained breathing apparatus (SCBA) to combat inhaled exposures, the air available is time-limited, and evidence suggests firefighters do not always use them consistently [27]. In particular, many firefighters remove their SCBAs during the overhaul period when the air appears clear [27]. Fent and colleagues have demonstrated the presence of numerous toxicants present in the air and on firefighters’ personal protective ensembles after the fire is extinguished [28-30].
Many of the chemicals and products of combustion associated with firefighting are also associated with adverse reproductive health outcomes, which can lead to miscarriage, low birth weight, developmental disorders, or infertility [31]. In particular, exposures during the first three months have been linked to miscarriage and birth defects, while exposures during the last six months may slow fetal growth, impede brain development, or lead to premature labor [31]. Treitman and associates [32] monitored personal air sampling devices among Boston firefighters and found carbon disulfide, which has been found to lead to changes in the menstrual cycle of women and, in turn, may contribute to fertility issues [31]. Of particular concern is the finding that even small exposures, if they occur during a particularly vulnerable period of time, can trigger lasting adverse health consequences [33].
Of note, the International Agency for Research on Cancer (IARC) recently updated its classification of the occupation of firefighting as “carcinogenic to humans” (Group 1) based on “sufficient” evidence [34]. There was “sufficient” evidence in humans for mesothelioma and bladder cancer. There was “limited” evidence for colon, prostate, and testicular cancers, melanoma, and non-Hodgkin lymphoma. There was also “strong” mechanistic evidence that occupational exposure as a firefighter induces epigenetic alterations, oxidative stress, and chronic inflammation, modulates receptor-mediated effects, and is genotoxic. Prenatal exposure to environmental factors that affect the epigenome (stress, infection, toxins) can disrupt gene expression programming in the embryo/fetus, resulting in developmental deficits, including abnormal brain development that can lead to later-life behavioral disorders [35].
Though not specific to firefighters, shift work has been recognized as deleterious to health by interrupting the body’s circadian rhythms [36,37]. It has been posited that disruptions in the endogenous timing system, through its interaction with the hypothalamic-pituitary axis, can interrupt the reproductive cycle of women working shift work [38]. While results are somewhat mixed, evidence suggests a possible link between shift work and miscarriage, low birth weight, and pre-term delivery [39,40].
While exercise during pregnancy has been found to have a beneficial impact on fetal development overall [41], guidelines recommend caution for strenuous activities such as those required by firefighting and rescue activities [31,42,43] because they may result in spontaneous abortion, pre-term birth, and low birth weight [44-46]. High ambient temperatures such as those experienced by firefighters while wearing encapsulating gear inside fires can increase core temperature to extremely high levels [47]. Evidence suggests even an eighteen-minute bout of firefighting will raise core temperature 1.2°C (0.67°F) [47,48] and that, among instructors exposed to repeated firefighting tasks, core temperature rises to an average of 38.9°C (102.02°F) [48] which is the temperature identified as the threshold for posing a teratogenic effect on an embryo or fetus [42]. Finally, evidence also suggests that pregnant women’s exposure to loud noises (e.g., air horns, sirens) may lead to lower fetal weight, increased risk of fetal mortality [22,23], and increased risk of hearing impairment among their offspring [49].
Another notable concern for women firefighters is the discrimination they experience regarding pregnancy and pregnancy-related issues [50]. While organizations such as the International Association of Firefighters (IAFF), the union which represents the majority of career firefighters, encourages accommodations for all women throughout their pregnancy and after the birth of their children [51], and federal law has protected workers against pregnancy discrimination since 1978 (e.g., Pregnancy Discrimination Act of 1978) [52], it is not clear that departments follow such non-discrimination policies [53]. Research indicates that hostility and discriminatory attitudes are common for women in the workplace, particularly male-dominated professions [54].
Organizations are increasingly sensitive to the challenges women face both physically and emotionally related to pregnancy, and the impact of policy on retention. For instance, the Secretary of the United States Air Force (USAF) recently released a memorandum extending the post-pregnancy deployment deferment from six months to a year to assist new mothers in managing the work/life balance and as a means of increasing diversity in the USAF [55]. In response to the physical challenges resulting from pregnancy, the USAF extended the deferment of participation in fitness testing from six months to a year for new moms and women who have experienced a miscarriage after 20 weeks. Anecdotal evidence and fire service trade journals suggest that similar accommodations have not yet been developed by the fire service [53]. Despite recommendations from national organizations [51], it does not seem that policies are consistently implemented [53], although data on policies nationally is lacking.
This review found a large gap in the literature examining reproductive health outcomes of firefighters published between the early 1990s and the present (starting in 2018). There has been significant work examining the exposures firefighters face (both chemical and non-chemical), and there is non-firefighter data to support the adverse reproductive effects of many of the exposures common on the fireground (chemical, biological, heat, noise, radiation, extreme physical work). Subsequently, there is an absence of information for physicians and healthcare providers to fully grasp the risks women firefighters face. This lack of data specifically on reproductive health for women firefighters has also led to minimal policy recommendations (i.e., when to restrict duties during pregnancy, guidance for breastfeeding, post-partum return to work, etc.) implemented in fire departments, if any at all. Future research should examine other potential hazards of firefighting on reproductive health. Male and female-mediated factors will be essential to examine.
Strengths
Limited research has examined reproductive health among firefighters. Moreover, minimal reviews have been published since the late 1980s and early 1990s. A noted strength of this review is amalgamating the relevant literature into one place and providing a thorough review of what exists and what still needs to be examined. Though limited, the research to date presents consistent findings that there are adverse reproductive health issues associated with the occupation of firefighting. Miscarriage and pre-term birth rates were consistently found among large samples of women firefighters in the US. Research both nationally and internationally highlights concerns for women and men firefighters. More research is necessary to examine specific mechanistic pathways for adverse reproductive health outcomes as well as how this information can impact policy and procedure in the fire service.
Limitations
Though this study has several strengths, the authors also acknowledge limitations. Though researchers used only one database for this literature review, the use of PubMed, which comprises more than 35 million citations for biomedical literature from MEDLINE, life science journals, and online books, provides a comprehensive picture of the available literature. There are also limitations when drawing conclusions from the examination of chemical exposure. The complexity of chemicals associated with firefighting may make it difficult to examine all pregnancy outcomes and chemical relationships properly. For example, while Jung and colleagues [20] recently found no difference in chemicals present in the breastmilk of women firefighters compared to women in the general population, only PBDEs and AhR response were examined. Future research must examine a wider range of chemicals to which firefighters are exposed to determine if they are present in breastmilk after fire exposure. Very little literature exists examining reproductive outcomes of firefighter among men. This is an area for future exploration.
References
- Department of Defense. Portrait of Active Duty Women. Department of Defense Office for Diversity, Equity, and Inclusion; 2021.
- Fahy R, Evarts B, Stein G (2022) US Fire Department Profile 2020. National Fire Protection Association.
- Jahnke S, Poston W, Haddock C, Jitnarin N, Hyder ML, Horvath C (2012) The health of women in the US fire service. BMC Womens Health 12: 39. [crossref]
- National Fallen Firefighters Foundation. 2021 National Fire Service Research Agenda; 2022. http://www.everyonegoeshome.com/wp-content/uploads/sites/2/2022/01/research-agenda-symposium-4-report.pdf.
- Evanoff BA, Rosenstock L (1986) Reproductive Hazards in the Workplace: A Case Study of Women Firefighters. Am J Ind Med 9: 503-515. [crossref]
- Olshan A, Teschke K, Baird P (1990) Birth defects among offsrping of firemen. Am J Epidemiol 131: 312-321. [crossref]
- Agnew J, McDiarmid MA, Lees PSJ, Duffy R (1991) Reproductive hazards of fire fighting I. Non-chemical hazards. Am J Ind Med 19: 433-445. [crossref]
- McDiarmid MA (1995) Reproductive hazards and firefighters. Occup Med 10: 829.
- McDiarmid MA, Lees P, Agnew J, Midzenski M, Duffy R (1991) Reproductive hazards of fire fighting II. Chemical hazards. Am J Ind Med 19: 447-472. [crossref]
- Jahnke SA, Poston W, Jitnarin N, Haddock CK (2018) Maternal and Child Health among Female Firefighters in the U.S. Matern Child Health J 22: 922-931. [crossref]
- Petersen KU, Hansen J, Ebbehoej NE, Bonde JP (2019) Infertility in a Cohort of Male Danish Firefighters: A Register-Based Study. Am J Epidemiol 188: 339-346. [crossref]
- Jung A (2021) Adverse Reproductive Health Outcomes in the US Fire Service: Results from a Survey of Women Firefighters. University of Arizona.
- Davidson S, Jahnke S, Burgess J, Jacobs E, Billheimer D, et al. (2022) Anti-Müllerian Hormone Levels among Female Firefighters. Int J Environ Res Public Health 19: 5981. [crossref]
- Di Renzo GC, Conry JA, Blake J, DeFrancesco MS, DeNicola N, et al. (2015) International Federation of Gynecology and Obstetrics opinion on reproductive health impacts of exposure to toxic environmental chemicals. Int J Gynaecol Obstet 131: 219-225. [crossref]
- Fabian T, Borgerson JL, Kerber SI, et al. (2010) Firefighter Exposure to Smoke Particulates. Underwriters Laboratories.
- McDiarmid MA, Lees PS, Agnew J, Midzenski M, Duffy R (1991) Reproductive hazards of fire fighting II. Chemical hazards. Am J Ind Med 19: 447-472. [crossref]
- Trowbridge J, Gerona R, Lin T, Rudel RA, Bessonneau V, et al. (2020) Exposure to Perfluoroalkyl Substances in a Cohort of Women Firefighters and Office Workers in San Francisco. Environ Sci Technol 54: 3363-3374. [crossref]
- Clarity C, Trowbridge J, Gerona R, Ona K, McMaster M, et al. (2021) Associations between polyfluoroalkyl substance and organophosphate flame retardant exposures and telomere length in a cohort of women firefighters and office workers in San Francisco. Environ Health 20. [crossref]
- Trowbridge J, Gerona R, McMaster M, Ona K, Clarity C, et al. (2022) Organophosphate and Organohalogen Flame-Retardant Exposure and Thyroid Hormone Disruption in a Cross-Sectional Study of Female Firefighters and Office Workers from San Francisco. Environ Sci Technol 56: 440-450. [crossref]
- Jung A, Beitel S, Gutenkunst S, Billheimer D, Jahnke SA, et al. (2023) Excretion of polybrominated diphenyl ethers and AhR activation in breastmilk among firefighters. Toxicol Sci. [crossref]
- Park J, Ahn Y, Kim M (2020) Pregnancy, childbirth, and puerperium outcomes in female firefighters in Korea. Ann Occup Environ Med 32(e8). [crossref]
- Agnew J, McDiarmid MA, Lees PS, Duffy R (1991) Reproductive hazards of fire fighting I. Non-chemical hazards. Am J Ind Med 19: 433-445. [crossref]
- Olshan AF, Teschke K, Baird PA (1990) Birth defects among offspring of firemen. Am J Epidemiol 131: 312-321. [crossref]
- Watkins E, Walker A, Mol E, Jahnke S, Richardson A (2019) Women Firefighters’ Health and Well-Being: An International Survey. Womens Health Issues 29: 424-431. [crossref]
- Kehler A, Jahnke SA, Haddock CK, Poston W, Jitnarin N, et al. (2018) Reproductive Health Concerns Among Female Firefighters. Int Fire Serv J 12: 15-29. [crossref]
- Engelsman M, Toms L, Wang X, Banks A, Blake D (2021) Effects of firefighting on semen parameters: an exploratory study. Reprod Fertil 2: L13-15. [crossref]
- Haddock CK, Jahnke SA, Poston WSC, Jitnarin N, Kaipust CM, et al. (2012) Alcohol use among firefighters in the Central United States. Occup Med Oxf Engl 62: 661-664. [crossref]
- Fent KW, Evans DE, Booher D, Pleil JD, Stiegel MA, et al. (2015) Volatile Organic Compounds Off-gassing from Firefighters’ Personal Protective Equipment Ensembles after Use. J Occup Environ Hyg 12: 404-414. [crossref]
- Fent KW, Evans DE, Babik K, Striley C, Bertke S, et al. (2018) Airborne contaminants during controlled residential fires. J Occup Environ Hyg 15: 399-412. [crossref]
- Fent KW, LaGuardia M, Luellen D, McCormick S, Mayer A, et al. (2020) Flame retardants, dioxins, and furans in air and on firefighters’ protective ensembles during controlled residential firefighting. Environ Int 140: 105756. [crossref]
- National Institute for Occupational Safety and Health (NIOSH). (1999) The Effects of Workplace Hazards on Female Reproductive Health. National Institute of Occupational Safety and Health.
- Treitman RD, Burgess WA, Gold A (1980) Air contaminants encountered by firefighters. Am Ind Hyg Assoc J 41: 796-802. [crossref]
- Grandjean P, Bellinger D, Bergman Å, Cordier S, Davey-Smith G, et al. (2007) The Faroes Statement: Human Health Effects of Developmental Exposure to Chemicals in Our Environment. Basic Clin Pharmacol Toxicol. [crossref]
- Demmers P, DeMarini D, Fent K, Glass DC, Hansen J, et al. (2022) Carcinogenicity of occupational exposure as a firefighter. Lancet Oncol 23: 985-986. [crossref]
- Kundakovic M, Jaric I (2017) The Epigenetic Link between Prenatal Adverse Environments and Neurodevelopmental Disorders. Genes 8: 104. [crossref]
- Amani R, Gill T (2013) Shift working, nutrition and obesity: implications for workforce health- a systematic review. Asia Pac J Clin Nutr 22: 505-515. [crossref]
- Puttonen S, Härmä M, Hublin C (2010) Shift work and cardiovascular disease – pathways from circadian stress to morbidity. Scand J Work Environ Health 36: 96-108. [crossref]
- Mahoney MM (2010) Shift Work, Jet Lag, and Female Reproduction Shift Work, Jet Lag, and Female Reproduction. Int J Endocrinol Int J Endocrinol 2010: e813764. [crossref]
- Mozurkewich EL, Luke B, Avni M, Wolf FM (2000) Working conditions and adverse pregnancy outcome: a meta-analysis. Obstet Gynecol 95: 623-635. [crossref]
- Nurminen T (1998) Shift work and reproductive health. Scand J Work Environ Health 24: 28-34. [crossref]
- Nascimento SL, Surita FG, Cecatti JG (2012) Physical exercise during pregnancy: a systematic review. Curr Opin Obstet Gynecol 24: 387-394. [crossref]
- American Medical Association (AMA) (1984) Effects of pregnancy on work performance. JAMA 251: 1995-1997. [crossref]
- MacDonald LA, Waters TR, Napolitano PG, et al. (2013) Clinical guidelines for occupational lifting in pregnancy: evidence summary and provisional recommendations. Am J Obstet Gynecol 209: 80-88. [crossref]
- Mamelle N, Laumon B, Lazar P (1984) Prematurity and occupational activity during pregnancy. Am J Epidemiol 119: 309-322. [crossref]
- Naeye RL, Peters EC (1982) Working during Pregnancy: Effects on the Fetus. Pediatrics 69: 724-727. [crossref]
- Taskinen H, Lindbohm ML, Hemminki K (1986) Spontaneous abortions among women working in the pharmaceutical industry. Br J Ind Med 43: 199-205. [crossref]
- Horn GP, Blevins S, Fernhall B, Smith DL (2013) Core temperature and heart rate response to repeated bouts of firefighting activities. Ergonomics 56: 1465-1473. [crossref]
- Smith DL, Horn G, Goldstein E, Petruzzello SJ (2008) Firefighter Fatalities and Injuries: The Role of Heat Stress and PPE. University of Illinois Fire Service Institute, Firefighter Life Safety Research Center; 2008. Accessed January 29, 2016.
- Lalande NM, Hétu R, Lambert J (1986) Is occupational noise exposure during pregnancy a risk factor of damage to the auditory system of the fetus? Am J Ind Med 10: 427-435. [crossref]
- Jahnke SA, Haddock CK, Jitnarin N, Kaipust CM, Hollerbach BS, et al. (2019) The Prevalence and Health Impacts of Frequent Work Discrimination and Harassment among Women Firefighters in the US Fire Service. BioMed Res Int 2019: 6740207. [crossref]
- International Association of Firefighters (IAFF). Reproductive Hazards: IAFF Pregnancy Policy. IAFF; 2012.
- S. Equal Employment Opportunity Commission (EEOC). Enforcement Guidance: Pregnancy Discrimination And Related Issues. U.S. Equal Employment Opportunity Commission, 2015.
- Willing L (2013) How to deal with the pregnant firefighter. FireRecruit.com. Published online May 1, 2013. Accessed January 24, 2016.
- Hebl MR, King EB, Glick P, Singletary SL, Kazama S (2007) Hostile and benevolent reactions toward pregnant women: Complementary interpersonal punishments and rewards that maintain traditional roles. J Appl Psychol 92: 1499-1511. [crossref]
- James DL, Welsh M, Cody J (2015) Diversity & Inclusion Initiative. United States Air Force.